Accidental and iatrogenic foreign body injuries to heart require immediate attention and its timely management is cornerstone to the life of an individual. We describe in detail five cases of Accidental and iatrogenic foreign body injuries to heart encountered between January 2013 and July 2016. Our series included the following: needle stick injury to the right atrium (1 case) retained catheter fragments in the distal main pulmonary artery (1 case), right ventricle injury during catheterisation study (1 case), right ventricle injury during permanent pacemaker lead placement (1 case), device migration in atrial septal defect closure (1 case). Foreign bodies were removed from the cardiac cavities when the patient presented with features of infection (1 case), cardiac tamponade (2 case), anxiety (1 case), and haemodynamic instability (1 case). The management of accidental and iatrogenic foreign body injuries to heart requires immediate attention. Foreign bodies in the heart should be removed irrespective of their location and symptomatology. Asymptomatic foreign bodies diagnosed immediately after the injury with associated risk factors should be removed; asymptomatic foreign bodies without associated risks factors or diagnosed accidentally after the injury also need surgical intervention to allay fears of anxiety in patient and their relatives, to prevent any late complications and also for medico-legal purpose.
Introduction
The injury to the heart due to foreign bodies may be accidental or iatrogenic. Recently the incidence of iatrogenic injury to heart has increased due to more availability and advancement of interventional cardiology in the field of catheter-based diagnostic and therapeutic procedures [1]. The incidence is more with debulking devices and migration of guide wires [2]. Iatrogenic inadvertent cardiac perforation often leads to life threatening cardiac tamponade. In case of cardiac tamponade the echo-guided pericardiocentesis has been shown to be effective and primary management, but the procedure itself may become a source of iatrogenic injury to the heart [3]. There are instances reported when foreign body injuries to the heart may also be observed occasionally years later after the cardiac insult [4]. The foreign body should be removed either through a surgical or percutaneous approach [5,6].
Case Series
A total of five cases are discussed who suffered the injuries between January 2013-July 2016. There were two male patients and three female patients. All of them were symptomatic and surgery was performed in all of the cases. These are described in details in [Table/Fig-1].
Description of patient details, symptoms, surgery and follow-up
| Age(y) | Sex | Time between injury and treatment initiation | Urgency | Symptoms | Localisation | Type | Surgery | Follow up(month) |
| 2 | F | 1 month | Elective | Fever | Right atrium | Needle stick | Without CPB | 48 |
| 42 | F | 6 hours | Emergency | Anxiety | Pulmonary artery | Catheter fragment | With CPB | 36 |
| 4 | M | 1 hour | Emergency | Cardiac tamponade | Right ventricle | Pigtail catheter | Without CPB | 24 |
| 60 | F | 1 hour | Emergency | Cardiac tamponade | Right ventricle | Pacemaker lead | Without CPB | 6 |
| 7 | M | 1hour | Emergency | Haemodynamic instability, device migration | Tricuspid valve orifice | Amplatzer device | With CPB | 3 |
CPB- Cardiopulmonary bypass
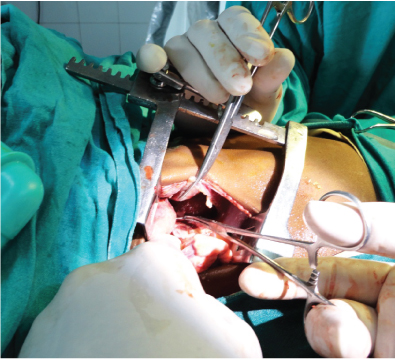
Patient 1
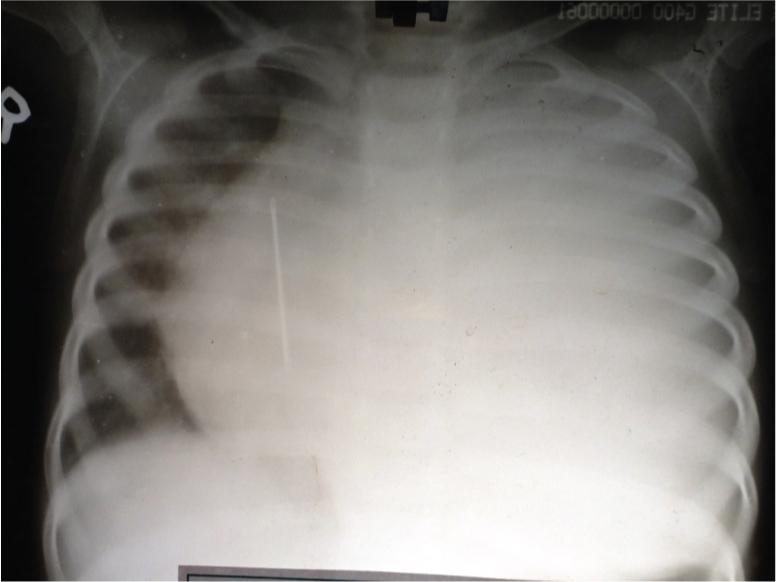
Foreign body in the right atrium- A two-year-old female baby presented to our cardiothoracic emergency department with chief complaints of respiratory distress, fever and features of sepsis for the last one month. On examination, she was drowsy, irritable, emaciated, with signs of dehydration. She was febrile, tachypneic, with a pulse rate of 138 per minute, blood pressure- 64/40 mm of Hg. The chest was clear but had diminished breath sounds on the left hemithorax. Her cardiovascular findings were normal except for the muffled heart sounds. On general body examination a small healed pinpoint scar mark was noted over the anterior chest wall on the right side. An urgent chest X-Ray was done which showed a mediastinal widening with a surprising finding of a foreign body in the mediastinum [Table/Fig-2]. She was resuscitated with fluids and an empirical antibiotic was started and shifted to emergency operation theatre. A left sided tube thoracostomy was done as this side of the hemithorax had diminished breath sounds. A right anterior thoracotomy through fourth intercostals space was performed. The right lung was normal with no collection in the pleural cavity; neither any foreign body could be noted. The pericardium was bulging; pericardiotomy was performed and around a litre of pus with fluid was drained out. After intense search we noted a shining blunt end of a metallic needle about 2 mm in length on the roof of the right atrial appendage [Table/Fig-3]. It was removed. It was a rusted sewing needle of about 5 cm in length. She recovered gradually and was discharged on the seventh postoperative day.
Chest X-Ray showing mediastinal widening with a foreign body in the mediastinum.
A shining blunt end of a metallic needle on the roof of the right atrial appendage.
Patient 2
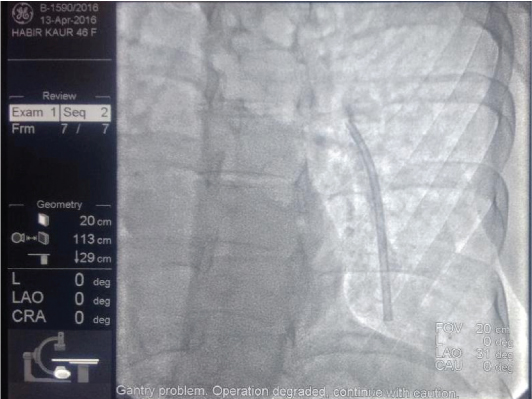
A 42-year-old lady undergoing adjuvant chemoradiation treatment for carcinoma of right breast with a Hickman Central venous catheter inserted through right subclavian vein for administration of chemotherapy presented to us in anxious state one hour after the removal of the catheter. It was noticed that a fragment of the catheter might still be inside her body. An urgent chest X-Ray was done to ascertain the size and site of fragment migration and it was noted that a 10 cm long fragment of a catheter over the cardiac silhouette was present. Subsequently an urgent fluoroscopy was done which revealed it to be migrated to the distal main pulmonary artery [Table/Fig-4]. This patient was transferred to our operation theatre. She underwent surgery though median sternotomy and on CPB with cardioplegic arrest of the heart the fragment was retrieved via a right atriotomy incision. Postoperative recovery was uneventful.
Fluoroscopic image of fragment of central venous catheter in main pulmonary artery.
Patient 3
A four-year-old male patient with echocardiography diagnosis of Tetralogy of Fallot was posted for diagnostic catheterization study. A guide wire was introduced through right femoral vein over which NIH catheter was inserted to Right Ventricle (RV). Once the dye was injected through the catheter, it started rapidly spreading into the pericardial cavity which can be clearly seen in fluoroscopy. There was perforation of RV and dye mixed blood extravasated to pericardium. Non Invasive Blood Pressure (NIBP) suddenly dropped to 42/34 mmHg and heart rate decreased (44/min) and she suffered cardiac arrest. She was intubated and cardiopulmonary resuscitation was started. Transthoracic echocardiography (TTE) showed cardiac tamponade with collapse of right ventricle. Immediately pericardiocentesis was attempted under the guidance of echocardiography and 150 ml of blood was aspirated. Haemodynamic parameters started to improve as the heart started to contract again, but hypotension still persisted. Blood transfusion was started and patient’s vitals were improved. TTE was done again, but this time there was no further pericardial collection. As a precautionary measure the cardiologist decided to put an intrapericardial sheath to aspirate if further collection occurs. A guide wire through subxiphoid region was attempted multiple times as there was a resistance felt while introducing it. Then multiple attempts were needed under fluoroscopic guidance to insert the sheath. Patient’s condition started deteriorating again, with NIBP 40/30 mmHg and HR 140/min. TTE revealed again some collection and 70 ml of blood was aspirated out immediately. The patient was shifted to operation theatre for surgical exploration. After exploration by midline sternotomy, about 80 ml blood drained out. Surprisingly, it was found that the perforated site of RV has stopped bleeding spontaneously by the hypertrophied RV muscle mass effect, but there was continuous bleeding from a lacerated epicardial vessel which contributed to the pericardial collection leading to further tamponade effect. This new epicardial vessel injury was caused by the multiple attempts to insert guide wire for introduction of the sheath. This second iatrogenic injury complicated the management of the first iatrogenic cardiac perforation and, thereby, created a life-threatening situation which needed immediate surgical exploration. Pericardial pledged repair of the epicardial vessel was done. Postoperative recovery was uneventful.
Patient 4
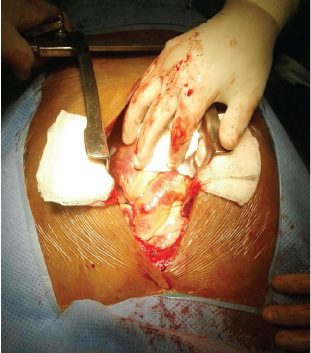
A 60-year-old lady with symptomatic bradycardia was taken for permanent pacemaker implantation. During the procedure she had a sudden collapse with tachycardia, severe hypotension. TTE revealed pericardial tamponade, collapse of right ventricle. She was referred to us for emergency surgical exploration. Through median sternotomy and pericardiotomy, blood and blood clots of approximately 400 ml was removed and it was noted that a lead of the device protruding through the diaphragmatic surface of the right ventricle into the pericardial cavity [Table/Fig-5]. A defect was approximated with 5-0 pledgeted polypropylene suture before removing the lead wire. After the defect was encircled around the lead, it was taken out through the femoral venous route and the defect was approximated with the suture without CPB [Table/Fig-6]. The haemostasis was secured. In the same sitting an epicardial pacemaker was implanted. Postoperatively the patient is doing well.
Tip of pacemaker lead perforating the diaphragmatic surface of the right ventricle.
Pledgeted sutures taken to repair the defect in right ventricle.
Patient 5
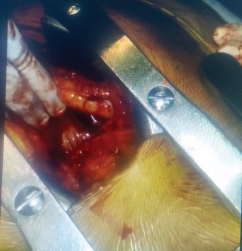
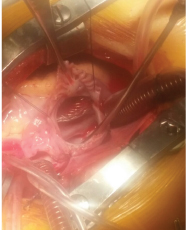
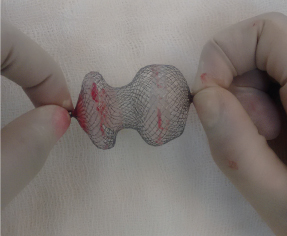
A seven-year-old male patient was taken for device closure of ostium secundum atrial septal defect (OS-ASD). An amplatzer device was placed through the defect. After one hour of the device placement the patient suddenly deteriorated with symptoms of breathlessness, tachycardia and hypotension. He was again taken to the cathlab and under fluoroscopic examination it was noted that the device had migrated out of the defect. He was immediately shifted to the operation theatre for device explantation. A median sternotomy was performed and the procedure was conducted under CPB and cardioplegia arrest of the heart. Through right atriotomy the device was found engaging at the tricuspid valve annulus totally occluding the orifice and entangled with the tricuspid valve chordae [Table/Fig-7]. The device was explanted [Table/Fig-8] and the OS-ASD margin was assessed and it was found that the inferior venacava rim was deficient which could be the reason for the non fixing of the defect to the defect margin. The defect was closed with tanned pericardial patch. The patient came off CPB well and the postoperative recovery was well.
Amplatzer device migration to tricuspid orifice.
Explanted amplatzer device.
Discussion
Foreign body injuries to the heart are getting more focussed due to the recent advancement and the low threshold for various procedures in the field of intervention cardiology. Foreign body injuries to the heart which are not visible after pericardiotomy necessitates the help of cardiopulmonary bypass circuit to arrest the heart and to prevent excess bleeding as well as for timely extraction of intact foreign bodies. Injuries to heart may result from either direct impact or from embolization from distal penetration sites or during some device implantation procedures [7–9].
Foreign body in mediastinum is uncommon. There are increasing reports of iatrogenic cause of foreign body injuries to the heart [10]. Though an accidental trauma to the right atrium leading to a life threatening sepsis in paediatric age group is very rare, it necessitates a thorough clinical examination of the whole body in these groups of patients who cannot communicate their symptoms. Recent scar marks on the body surface may guide as a site of wound of entry in these injuries. A simple chest X-Ray can direct us regarding the suspicion and diagnosing the position of any foreign body in the chambers of the heart and there is no need for other high radiation diagnostic modalities in this age group. Foreign bodies noted in the chambers of heart need urgent intervention. Foreign bodies in the right atrium can be taken out through right thoracotomy without the use of cardiopulmonary bypass thus avoiding sternotomy [11].
Removal of foreign bodies from the superior vena cava and right atrium without thoracotomy may also be performed under fluoroscopic guidance in few cases [12]. But there is a risk of radiation hazards in paediatric age group patients and hence should be avoided. Paediatric patients presenting with sepsis and any external injury mark should warrant a strong suspicion for foreign body injury. A right anterior thoracotomy through fourth intercostal space gives best exposure for the foreign bodies in the right chambers of heart.
Percutaneous insertion of central venous catheter is a routine hospital practice for patients needing long term intravenous therapy. Well documented complications of the procedure like arterial puncture leading to massive haemorrhage, pneumothorax, cardiovascular side-effects, risks of infection, thrombosis are not new [13]. Various complications like catheter fractures and catheter migration [14–17] is uncommon but serious with a prevalence of approximately 0.1% [18]. Penetration of a foreign body into the heart may result from either a direct injury to the heart or from embolization to the heart from distal penetration sites. The foreign body in this case may enter the right side of the heart or the pulmonary artery, embolizing through the venous blood flow [4–6].
Some patients become anxious about the presence of a cardiac foreign body, as observed in one case in our experience. This symptomatology, in our opinion, also stands as an absolute indication for surgical removal [4,19,20].
Sometimes a simple diagnostic cardiac catheterisation may become life threatening because of the procedure related complications. One of the serious life threatening complications of these injuries is cardiac perforation with an overall incidence of 0.01% [21]. Iatrogenic cardiac perforation may lead to life-threatening situation, and immediate surgical exploration is the only way to save the patient. Echo-guided pericardiocentesis is effective to manage such complications, thereby saving the patient. In our patient, the echo-guided aspiration was effective and markedly improved haemodynamically. The epicardial vessel injury by the sharp metal tip guide wire is rare but is a potential complication which might lead to a rapid cardiac tamponade and cardiac arrest as we have encountered in our case. Pericardiocentesis is an emergency therapeutic procedure in these patients; this procedure demands a high level of expertise in small children. Paediatric patients have less cardiopulmonary reserve; and may succumb to acute tamponade. The usual cause of tamponade after right ventricular perforation is bleeding from the right ventricle, but in our case the second tamponade was not due to bleeding from the right ventricle but was rather from new laceration injury of epicardial vessels which was undiagnosed till exploration. These complications leading to tamponade effect warrants prompt diagnosis and early treatment. Multiple attempts of guide wire insertion are very dangerous and should always be avoided. Interventions must be steady and smooth in all cases, especially in paediatric ones as delay between diagnosis and resuscitation endangers the life of a baby. Permanent pacemaker insertion is one of the common therapeutic interventions by the intervention cardiologists. However this implantation technique may sometimes cause cardiac injury leading to cardiac tamponade which is a life threatening situation [22]. It is reported that the incidence of cardiac tamponade following permanent pacemaker is more common in female gender [23]. Cardiac perforation with tamponade is a rare complication of device lead implantation and may mimic as ST elevation myocardial infarction [24]. The incidence of Cardiac Perforation has been reported to occur in up to 1% of pacemaker implantations. Symptoms of perforation include pleuritic chest pain and in the presence of pericardial effusion, patients may develop shortness of breath and hypotension as tamponade develops [25]. Device function is warranted though lead parameters are often within normal limits [26].
Transcatheter occlusion of secundum type ASD is a minimally invasive procedure which provides good cosmesis and avoids the need for cardiac surgery. But this technique has complications such as distal migration and residual shunts. Unfavourable anatomy and device diameter are the main reason for device migration. Over sizing the device also increases the risk of migration [27].
Percutaneous ASD closure has become an increasingly simplified procedure over the past decade [28]. The use of ASD device closure needs expertise in this field to lower the risk of device dislodgement, migration or embolization [29,30]. A cause of failure is early embolization [31]. The percentage of this early embolization is around 0.5% [32]. In symptomatic patients, the presence of symptoms is a primary indication for surgery, especially in case of cardiac tamponade or after blunt trauma [33]. The most common symptoms are fever, pericarditis and pericardial effusion, arrhythmia, thrombi, and neurotic manifestations, mainly anxiety. Among symptoms, fever may result from infection of pericardium or endocardium or sepsis, particularly from contaminated fragments [34,35].
Finally, the iatrogenic nature of some foreign bodies is associated with medico-legal implications that sometimes can influence the choice between surgical or conservative treatment. Surgical options depend on the localization of the foreign body and the need for cardiopulmonary bypass. Some authors suggest a median sternotomy approach in particular if pericardiectomy is needed [36]. It is also found that in these cases median sternotomy results in decreased morbidity and reduced hospitalization compared with thoracotomy [36,37].
Conclusion
The management of accidental and iatrogenic foreign body injuries to heart should be dealt without losing time. Symptomatic foreign bodies manifesting with infection, arrhythmia, or neurotic manifestations should be removed irrespective of their location. Asymptomatic foreign bodies diagnosed immediately after the injury with an associated risk of infection, embolization, or erosion should be removed. Life threatening complications of foreign body injuries like cardiac tamponade is a surgical emergency and no time should be lost further in the intervention room and urgent surgery is the only mode of therapy in these high risk individuals.
CPB- Cardiopulmonary bypass
[1]. Stolt V, Cook S, Räber L, Wani S, Garachamani A, Vogel R, Amplatzer septal occluder to treat iatrogenic cardiac perforationsCathet Cardiovasc Intervent 2012 79:263-70. [Google Scholar]
[2]. Witzke CF, Martin-Herrero F, Clarke SC, Pomerantzev E, Palacios IF, The changing pattern of coronary perforation during percutaneous coronary intervention in the new device eraJ Invasive Cardiol 2004 16(6):257-301. [Google Scholar]
[3]. Vaitkus PT, Herrmann HC, LeWinter MM, Treatment of malignant pericardial effusionJAMA 1994 272(1):59-64. [Google Scholar]
[4]. Hasegawa J, Noguchi N, Yamasaki J, Kotake H, Mashiba H, Sasaki S, Delayed cardiac tamponade and haemothorax induced by an acupuncture needleCardiology 1991 78:58-63. [Google Scholar]
[5]. Best IM, Transfemoral extraction of an intracardiac bullet embolusAm Surg 2001 67(4):361-63. [Google Scholar]
[6]. Kaushik VS, Mandal AK, Non-surgical retrieval of a bullet embolus from the right heartCatheter Cardiovasc Interv 1999 47(1):55-57. [Google Scholar]
[7]. Symbas PN, Picone AL, Hatcher CR, Vlasis-Hale SE, Cardiac missiles. A review of the literature and personal experienceAnn Surg 1990 211(5):639-47. [Google Scholar]
[8]. Mattox KL, Beall AC Jr, Ennix CL, DeBakey ME, Intravascular migratory bulletsAm J Surg 1979 137(2):192-95. [Google Scholar]
[9]. Ledgerwood AM, The wandering bulletSurg Clin North Am 1977 57(1):97-109. [Google Scholar]
[10]. Lillehei CW, Bonnabeau RC Jr, Grossling S, Removal of iatrogenic foreign bodies within cardiac chambers and great vesselsCirculation 1965 32(5):782-87. [Google Scholar]
[11]. Kim KH, Ahn H, Intracardiac foreign body: a sewing needle in right ventricleEur J Cardiothorac Surg 2001 19(4):513 [Google Scholar]
[12]. Actis Dato GM, Arslanian A, Di Marzio P, Filosso PL, Ruffini E, Posttraumatic and iatrogenic foreign bodies in the heart: report of fourteen cases and review of the literatureJ Thorac Cardiovasc Surg 2003 126(2):408-14. [Google Scholar]
[13]. Mahadeva S, Cohen A, Bellamy M, The stuck central venous catheter: beware of potential hazardsBr J Anaesth 2002 89(4):650-52. [Google Scholar]
[14]. Iannelli A, Kianmanesh R, Msika S, Marano A, Levesque M, Grandjean M, Hay JM, Post-traumatic fracture and migration in the pulmonary artery of the catheter of a totally implantable venous access device. Unusual complicationMinerva chirurgica 2001 56(3):303-06. [Google Scholar]
[15]. di Carlo I, Fisichella P, Russello D, Puleo S, Latteri F, Catheter fracture and cardiac migration: a rare complication of totally implantable venous devicesJ Surg Oncol 2000 73(3):172-73. [Google Scholar]
[16]. Hou WY, Sun WZ, Chen YA, Wu SM, Lin SY, “Pinch-off sign” and spontaneous fracture of an implanted central venous catheter: report of a caseJ Formos Med Assoc 1994 93(suppl 1):S65-S69. [Google Scholar]
[17]. Kapadia S, Parakh R, Grover T, Yadav A, Catheter fracture and cardiac migration of a totally implantable venous deviceIndian J Cancer 2005 42(3):155-57. [Google Scholar]
[18]. Chang CL, Chen HH, Lin SE, Catheter fracture and cardiac migration–an unusual fracture site of totally implantable venous devices: report of two casesChang Gung Med J 2005 28(6):425-30. [Google Scholar]
[19]. Morton JR, Reul GJ, Arbegast NR, Okies JE, Beall AC Jr, Bullet embolus to the right ventricle. Report of three casesAm J Surg 1971 122(5):584-90. [Google Scholar]
[20]. Van Way CW III, Intrathoracic and intravascular migratory foreign bodiesSurg Clin North Am 1989 69(1):125-33. [Google Scholar]
[21]. Friedrich SP, Berman AD, Baim DS, Diver DJ, Myocardial perforation in the cardiac catheterization laboratory: incidence, presentation, diagnosis, and managementCathet Cardiovasc Diagn 1994 32(2):99-107. [Google Scholar]
[22]. Moazzami K, Dolmatova E, Mazza V, Klapholz M, Waller A, Trends in cardiac tamponade among recipients of permanent pacemakers in the united states: 2008 to 2012J Am Coll Cardiol 2016 67(13):776 [Google Scholar]
[23]. Dolmatova E, Moazzami K, Mazza V, Klapholz M, Waller A, Predictors of cardiac tamponade from permanent pacemaker implantation: Analysis of 1,014,713 proceduresJ Am Coll Cardiol 2016 67(13):706 [Google Scholar]
[24]. Qian P, Orr Y, Davis L, An unusual cause of localised ST elevation following insertion of a permanent pacemakerHeart Lung Circ 2016 25(10):e140-e142. [Google Scholar]
[25]. Hirschl DA, Jain VR, Spindola-Franco H, Gross JN, Haramati LB, Prevalence and characterization of asymptomatic pacemaker and ICD lead perforation on CTPacing Clin Electrophysiol 2007 30(1):28-32. [Google Scholar]
[26]. Wang NC, Williams JL, Jain SK, Shalaby A, Images in radiology. Post-pacemaker pulsationsAm J Med 2009 122(4):345-47. [Google Scholar]
[27]. Yetkin U, Yurekli I, Akyildiz ZI, Gokalp O, Tetik O, Lafci B, Emergency surgical approach to device emboli due to migration of the atrial septal defect occluderArch Med Sci 2014 10(3):464-69. [Google Scholar]
[28]. Chessa M, Carminati M, Butera G, Roberta M B, Manuela D, Luca R, Early and late complications associated with transcatheter occlusion of secundum atrial septal defectJ Am Coll Cardiol 2002 39(6):1061-65. [Google Scholar]
[29]. Motreff P, Dauphin C, Souteyrand G, Cardiac perforation and tamponade 3 months after transcatheter PFO closure by STARFlex device: A case reportCatheter Cardiovasc Interv 2008 71(3):412-16. [Google Scholar]
[30]. Meier B, Closure of patent foramen ovale: technique, pitfalls, complications, and follow-upHeart 2005 91(4):444-48. [Google Scholar]
[31]. Guérin P, Lambert V, Godart F, Legendre A, Petit J, Bourlon F, Transcatheter closure of patent foramen ovale in patients with platypnea-orthodeoxia: results of a multicentric French registryCardiovasc Intervent Radiol 2005 28(2):164-68. [Google Scholar]
[32]. Ueda H, Yanagi S, Nakamura H, Ueno K, Gatayama R, Asou T, Device closure of atrial septal defect: immediate and mid-term resultsCirc J 2012 76(5):1229-34. [Google Scholar]
[33]. Gandhi SK, Marts BC, Mistry BM, Brown JW, Durham RM, Mazuski JE, Selective management of embolized intracardiac missilesAnn Thorac Surg 1996 62(1):290-92. [Google Scholar]
[34]. Balbi M, Bertero G, Bellotti S, Rolandelli ML, Caponnetto S, Right-sided valvular endocarditis supported by an unexpected intracardiac foreign bodyChest 1990 97(6):1486-88. [Google Scholar]
[35]. Hong-Barco P, O’Toole J, Gerber ML, Domat I, Moquin M, Jackson SC, Endocarditis due to six entrapped pacemaker leads and concomitant recurrent coronary arteriosclerosisAnn Thorac Surg 1988 46(1):97-99. [Google Scholar]
[36]. Culliford A.T, Surgery for chronic constrictive pericarditis. A.J. Roberts (Ed.)Difficult problems in adult cardiac surgery 1985 ChicagoYear Book Medical Publishers:317-324. [Google Scholar]
[37]. LeMaire SA, Wall MJ Jr, Mattox KL, Needle embolus causing cardiac puncture and chronic constrictive pericarditisAnn Thorac Surg 1998 65(6):1786-87. [Google Scholar]