BMV is one of the methods of treatment for haemodynamically significant rheumatic mitral stenosis if the valve anatomy is suitable for balloon dilatation. BMV with inoue balloon is the most common technique being followed worldwide [1–3]. Over the wire BMV is a modified technique using JOMIVA balloon and is being followed in certain centres [4]. There are studies assessing the short term as well as long term outcome of BMV using JOMIVA balloon [4,5]. Significant MR is the most common serious complication after BMV [6]. Mechanism of significant post-procedure MR as well as incidence, short term and long term follow-up of patients who developed significant MR following BMV with inoue balloon has been well reported [7–10]. There are no studies so far assessing the mechanism of significant MR following BMV using JOMIVA balloon. In this study we have assessed the mechanism of significant MR and immediate clinical outcome of significant MR following BMV with JOMIVA balloon.
Materials and Methods
Echocardiographic and clinical parameters of patients who underwent elective BMV in PSG Institute of Medical Sciences, Tamil Nadu, India from Jan 2010 to Dec 2014 and developed significant MR post procedure were analyzed retrospectively. Patients who underwent emergency BMV under mechanical ventilation were excluded from the study.
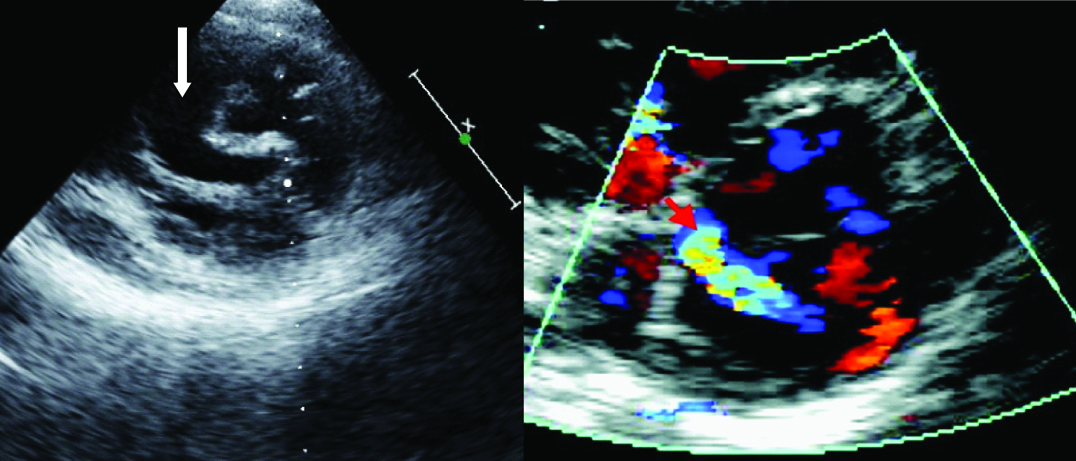
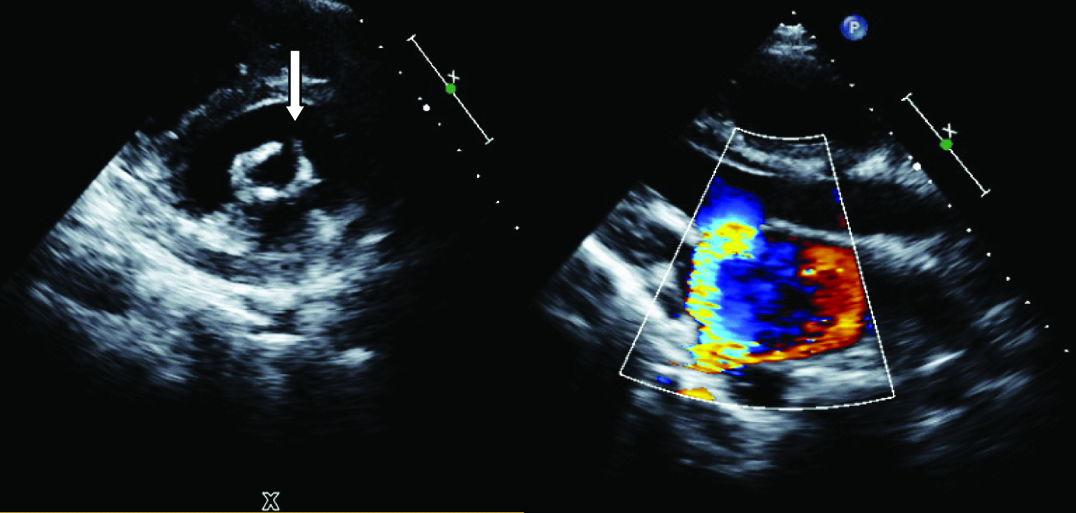
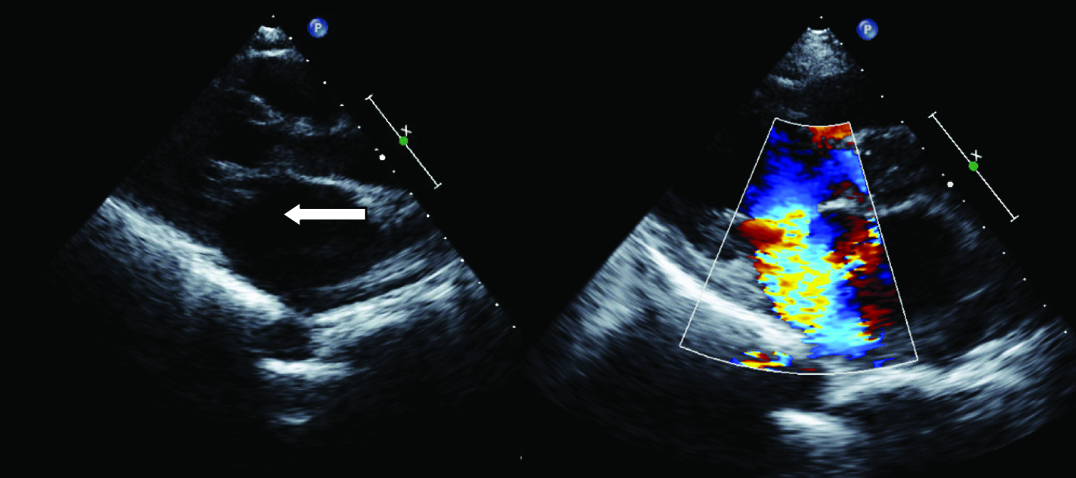
A detailed analysis of pre-procedural echocardiographic parameters which included severity of the mitral stenosis, morphological analysis of the valve and Wilkin scoring were done. Severity of mitral stenosis was assessed by 2 dimensional mitral valve area and gradient across the mitral valve. Wilkin scoring included analysis of valve thickness, mobility of leaflets, leaflet calcium and subvalvular disease. A score of 0 to 4 was given to each parameter with 0 being normal or absent and 4 being severe or extensive [11]. Post- procedure echocardiography was done. MR was graded as mild, moderate and severe according to the jet area and width of vena contracta whichever estimates the severity more. MR was graded as mild, moderate and severe when the jet area occupies less than 20%, 20-40% and more than 40% of left atrium respectively. Width of vena contracta less than 0.3 cm, 0.3-0.7 cm, more than or equal to 0.7 cm classifies MR as mild, moderate and severe respectively [12]. Patient is considered to have significant MR when it is moderate or severe. Diagnosis of commissural MR was based on a jet of MR that is clearly originating at any one of the commisures [Table/Fig-1]. Leaflet tear was diagnosed when there is laceration of any one of the leaflet with jet of MR originating at the site of echocardiographic dropout [Table/Fig-2]. Chordal rupture was diagnosed when there is a flail tip of the leaflet with MR jet originating at the site of the flail segment [Table/Fig-3].
Transthoracic echocardiographic image showing severe mitral regurgitation because of commissural separation after BMV. Left sided image showing parasternal short axis view with an echocardiographic dropout at the medial commissure (down facing arrow). Right sided image showing a clearly definable jet of MR originating at the medial commissure was shown by colour Doppler flow mapping.
Transthoracic echocardiographic image showing severe mitral regurgitation because of leaflet tear after BMV. Left sided image showing a parasternal short axis view with an echocardiographic dropout in the anterior mitral leaflet (down facing arrow). Right sided image showing a mitral regurgitation jet which is originating at the site of leaflet tear in the anterior mitral leaflet.
Transthoracic echocardiographic image showing severe mitral regurgitation because of chordal rupture after BMV. Left sided image showing a parasternal long axis view with a dangling structure attached to the posterior mitral leaflet protruding into the left atrial cavity during systole (left facing arrow). Mitral regurgitation jet is originating at the site of prolapsing leaflet tip.
Symptom status of the patient after the procedure which included presence of clinical evidence of pulmonary oedema and New York Heart Association functional class status were noted. Need for emergency mitral valve replacement was also included in the analysis. Institute ethical committee clearance was obtained.
Procedure:
All the patients were given prophylactic antibiotics before the procedure. Femoral arterial and venous access were taken. Atrial septal puncture was done with Brocken brough needle [13]. A Mullin sheath and dilator was tracked inside the left atrium. Subsequently a Swan Ganz catheter was taken inside the left atrium through the Mullin sheath. Mitral valve was crossed with the Swan Ganz catheter. A support wire was taken across the mitral valve through the Swan Ganz catheter. An appropriate sized JOMIVA balloon catheter was taken across the mitral valve over the support wire and the valve was dilated. Procedure was considered successful if the gradient across the mitral valve reduced by 50%, valve area increased more than 1.5 cm2 and no increase in MR by more than 2 grades.
Statistical Analysis
Statistical analysis was carried out using SPSS version 21.0 Categorical variables like causes of MR and immediate clinical parameters are expressed as percentages. Continuous variables are presented as mean and standard deviation.
Results
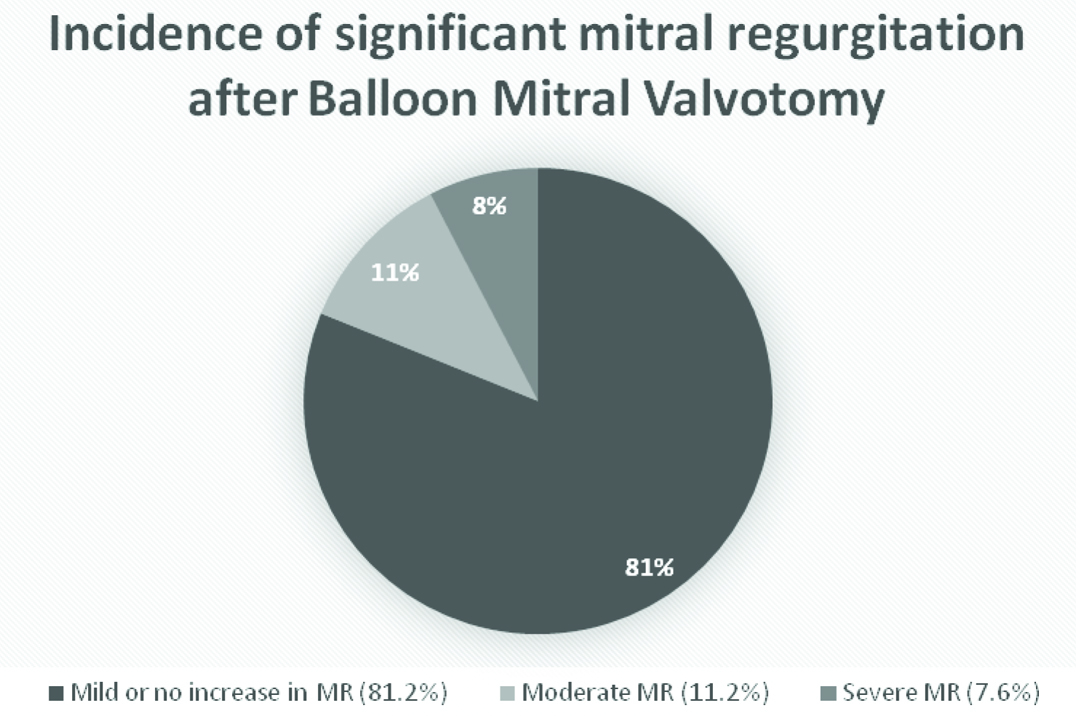
Incidence of significant mitral regurgitation after balloon mitral valvuloplasty using JOMIVA balloon: Totally 249 patients underwent BMV between 2010 and 2014 in our institute with JOMIVA balloon. All 48 patients who developed significant MR (moderate to severe) post procedure were included in the analysis. Baseline characteristics of patients who developed significant MR are shown in [Table/Fig-4]. Severe MR was documented after the procedure in 19 (7.6%) patients and 29 (11.2%) patients developed moderate MR [Table/Fig-5]. Echocardiographic analysis of the valve pre-procedure has shown that the mean Wilkin score was more than eight in patients who developed significant mitral regurgitation. Many of the patients (31%) had mild MR before the procedure itself as assessed by echocardiography.
Showing the baseline characteristics of patients who developed significant mitral regurgitation after balloon mitral valvotomy.
| Parameters | Moderate MR29 Patients | Severe MR19 Patients |
|---|
| Age | 35±12 | 41±7 |
| Sex | M: 8 (28.57%) | M: 6 (31.57%) |
| F: 21 (71.42%) | F: 13 (68.42%) |
| Past history of BMV/CMV | BMV : 1 (3.57%) | BMV : 4 (21.05%) |
| CMV : 3 (10.71%) | CMV : 2 (10.52%) |
| Atrial fibrillation | 4 (14.28 %) | 4 (21.05%) |
| Mean mitral valve area (cm2) | 0.9±0.2 | 0.8±0.3 |
| Mean gradient across mitral valve | 17±9 | 18±8 |
| Echocardiographic score | 8.2±1.3 | 8.4±1.2 |
| Thickness | 1.9±0.6 | 1.8±0.5 |
| Mobility | 2.3±0.5 | 2.2±0.4 |
| Calcium | 2.1±0.6 | 2.2±0.6 |
| Subvalvular fusion | 1.9±0.6 | 2.0±0.4 |
| Pre existing mitral regurgitation | 8 (28.57%) | 7 (36.84%) |
| Left atrial appendage clot | 1 (3.57%) | 0 |
BMV-Balloon mitral valvuloplasty, CMV- Commissural mitral valvuloplasty
Showing the incidence of significant Mitral Regurgitation (MR) after Balloon Mitral Valvuloplasty (BMV) with JOMIVA balloon.
Morphological analysis of valve by echocardiography in patients who developed significant mitral regurgitation: Commisural MR which was caused by a wide separation of medial or lateral commissure was the most common reason for significant MR in our study population. Commisural MR had contributed to 73.68% (14) of patients with severe MR and 85.71% (24) of patients with moderate MR [Table/Fig-6,7].
Showing the morphological changes in the valve responsible for Mitral Regurgitation (MR) in patients with moderate (left) and severe MR (right).
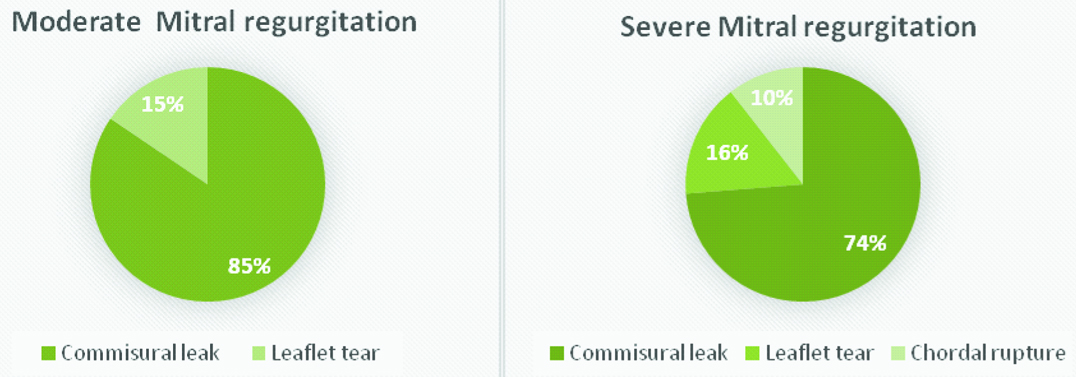
Morphological characteristics of the mitral valve of patients who developed significant mitral regurgitation after Balloon Mitral Valvotomy (BMV).
| Cause of Mitral Regurgitation | Moderate Mitral Regurgitation | Severe Mitral Regurgitation |
|---|
| Commisural separation | 24(85.71%) | 14(73.68%) |
| Leaflet tear | 4(14.28%) | 3 (15.78%) |
| Chordal rupture | Nil | 2(10.52%) |
| Papillary muscle rupture | Nil | Nil |
Leaflet tear causing significant MR was the second most common reason which had contributed to 15.78% of patients with severe MR and 14.28% of patients with moderate MR. Anterior mitral leaflet tear was the most common which was noted in two and three patients with severe and moderate MR respectively. Rest of the patients with leaflet tear had posterior leaflet involvement.
Chordal rupture was noted in two (10.5%) patients with severe MR. None of the patients with moderate MR noted to have chordal rupture. Papillary muscle rupture was not noted in any of the cases with moderate or severe MR.
Clinical outcome of patients who developed significant MR: Among the patients who developed severe MR one patient had significant worsening of breathlessness which could not be managed medically and had to be referred for mitral valve replacement during index hospitalization [Table/Fig-8]. Five (26.3%) patients with severe MR had worsening breathlessness after the procedure which could be managed medically and did not warrant mitral valve replacement during index hospitalization. Other patients (68.4%) with severe MR had symptomatic improvement after the procedure. None of the patients with moderate MR had symptomatic worsening after the procedure.
Adverse clinical outcomes of patients who developed significant mitral regurgitation after balloon mitral valvotomy.
| Symptoms | Moderate Mitral Regurgitation | Severe Mitral Regurgitation |
|---|
| Pulmonary oedema after the procedure | Nil | 2 (10.52%) |
| Worsening breathlessness after the procedure | Nil | 6 (31.57%) |
| Mitral valve replacement during index hospitalization | Nil | 1 (5.26%) |
Discussion
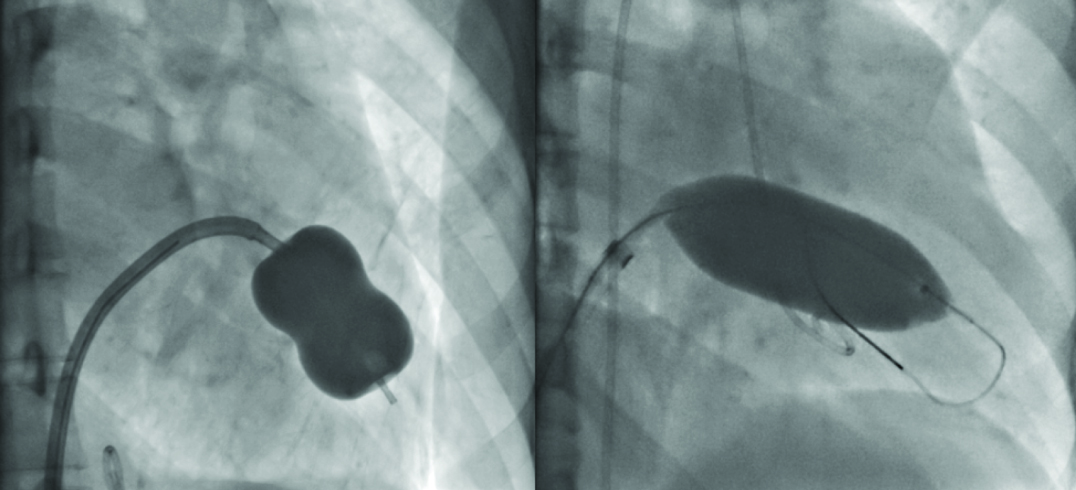
Over the wire BMV using JOMIVA was shown to be a cost effective alternative to the widely followed inoue technique [4,5]. JOMIVA balloon catheter is different from inoue balloon in a way that it is a cylindrical balloon and not a dumbbell shaped balloon [Table/Fig-9]. Mechanism of mitral regurgitation following JOMIVA BMV was not described earlier.
Images showing Inoue balloon: a) With a central waist when inflated and JOMIVA balloon; b) Which is cylindrical when inflated.
Baseline characteristics of patients who developed significant MR following BMV showed that, the mean echocardiographic score (Wilkin score) was more than eight in patients with moderate as well as severe MR. Pre-existing MR was noted in many (31%) of the patients. This shows that the patients had a higher risk mitral valve before the procedure.
Incidence of severe MR following BMV with inoue balloon reported earlier was varying between 3.5-12% [7]. Incidence of significant MR following JOMIVA BMV was again reported earlier and was 11% [4,5]. In our study, the incidence of significant mitral regurgitation was found to be higher than the previous studies which is explained by the higher baseline echocardiographic score (Wilkin’s score) of patients.
Morphological changes in the valve which lead on to MR after BMV were analyzed. MR following BMV could be due to chordal rupture, leaflet tear or commissural separation itself. Mechanism of MR following JOMIVA balloon is likely to be different for inoue balloon since JOMIVA balloon being a cylindrical balloon in contrast to inoue balloon [Table/Fig-9]. In a study by Kim MJ et al., has shown that, commissural separation was the most common cause for significant MR following BMV which contributed to 57% of patients, chordal rupture contributed to 26% of patients and leaflet laceration contributed to 17% [7]. Herrmann HC et al., in his study has shown that chordal rupture being the most common cause of mitral regurgitation and less often by leaflet tear [9]. In our study, commisural MR which was caused by separation of medial or lateral commissures was the most common cause for MR which contributed to 80.8% (38 patients) of patients with significant MR. Leaflet tear was the second most common cause for significant MR which had contributed to 14.5% (seven patients) of mitral regurgitation. Chordal rupture was noted in only two cases (4.1%) of significant MR. JOMIVA balloon when inflated it expands uniformly when compared to inoue balloon in which the proximal and distal end expands more than the central portion [Table/Fig-9]. Hence, JOMIVA balloon is less likely to cause damage to the subvalvular apparatus.
Among the patients who developed significant MR one patient (0.2%) had significant worsening of breathlessness and clinical features of pulmonary congestion which was refractory for medical management. So that, patient had to be referred for mitral valve replacement during index hospitalization. Earlier studies of BMV using inoue balloon showed that, the requirement of mitral valve replacement shortly after BMV was 3.2% [10]. In spite of severe MR after the procedure many (68% of patients with severe MR) patients had symptomatic improvement. None of the patients with moderate MR developed symptomatic worsening. This shows that, moderate MR is unlikely to be of clinical significance at least at the time of discharge. Various studies in the past enumerating the clinical and haemodynamic parameters which could predict the severity of MR immediately after BMV. Presence of hypotension, pulmonary oedema, orthopnoea immediately after BMV was shown to suggest the occurrence of severe MR immediately after the procedure [14]. Our study result helps us to understand the mechanism of significant MR after BMV with JOMIVA balloon which is different from that of inoue balloon. This study also helps us to understand immediate outcome of significant MR after BMV so that we can plan for further management and follow up strategies.
Limitation
Total number of patients included in the analysis were small which may not represent the entire set of patients who develop significant mitral regurgitation after BMV with JOMIVA balloon. Our study being a retrospective one it has its own limitations.
Conclusion
Severe MR following JOMIVA BMV results most commonly due to wide separation of commisures. JOMIVA balloon is less likely to cause damage to subvalvular structures than inoue balloon. Most patients who develop severe MR do not require emergency mitral valve replacement. Moderate MR is well tolerated clinically.
BMV-Balloon mitral valvuloplasty, CMV- Commissural mitral valvuloplasty