Intramuscular Capillary Haemangioma of the Temporalis Muscle: A Rare Case with A Review of the Literature
Nikhil Arora1, Eishaan Kamta Bhargava2, Arif Kavungal Nambillath3, Ravi Meher4
1 Senior Resident, Department of Otorhinolaryngology – Head and Neck Surgery, Maulana Azad Medical College and Associated Loknayak, G.N.E.C., and G.B. Pant Hospitals, New Delhi, India.
2 Senior Resident, Department of Otorhinolaryngology – Head and Neck Surgery, Maulana Azad Medical College and Associated Loknayak, G.N.E.C., and G.B. Pant Hospitals, New Delhi, India.
3 Junior Resident, Department of Otorhinolaryngology – Head and Neck Surgery, Maulana Azad Medical College and Associated Loknayak, G.N.E.C., and G.B. Pant Hospitals, New Delhi, India.
4 Professor, Department of Otorhinolaryngology – Head and Neck Surgery, Maulana Azad Medical College and Associated Loknayak, G.N.E.C., and G.B. Pant Hospitals, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Eishaan Kamta Bhargava, 123, Sunder Nagar, New Delhi – 110003, India.
E-mail: eishaan@gmail.com
An Intramuscular Haemangioma (IMH) is a benign mesenchymal tumour of the endothelial cells that accounts for less than 1% of all haemangiomas. Here we report the case of a capillary type intramuscular haemangioma in a five-year-old boy, only the fourth such case reported in literature, along with a relevant review of the literature. The lesion was surgically managed, with no recurrence in the follow up period till date.
Male child, Muscle neoplasms/radiography, Temporal muscle/pathology
Case Report
A five-year-old boy was brought to the Department of Otorhinolaryngology outpatient department with a painless swelling behind the left ear that had been gradually increasing in size for two years, with no other complaints.
Physical examination revealed a single, soft, non-tender swelling, 4x3 cm in size, in the left post-aural region pushing the pinna forward, with visible dilated vessels on the surface of the swelling [Table/Fig-1]. The external auditory canal and tympanic membrane were normal.
A single swelling, 4x3 cm in size, in the left post-aural region pushing the pinna forward, with visible dilated vessels on the surface of the swelling.

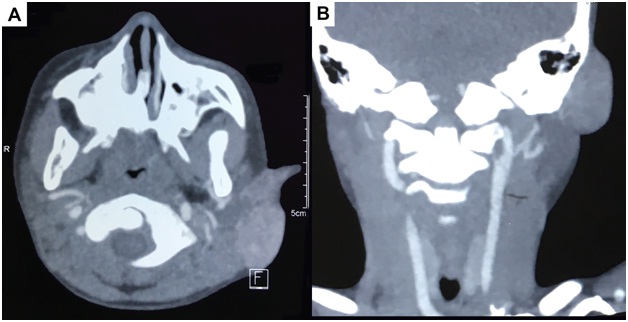
Ultrasound examination showed a soft tissue mass with intense vascularity on colour doppler and an arterial waveform on spectral doppler. Fine Needle Aspiration Cytology (FNAC) of the lesion was non-diagnostic on account of a bloody specimen. Computed Tomography (CT) angiography revealed a vascular malformation of size 35 x 25 x 15 mm in the left post-aural region with feeders from the posterior auricular and occipital branches of left external carotid artery [Table/Fig-2].
CT angiography revealed a vascular malformation of size 35 x 25 x 15 mm in the left post-aural region with feeders from the posterior auricular and occipital branches of left external carotid artery.
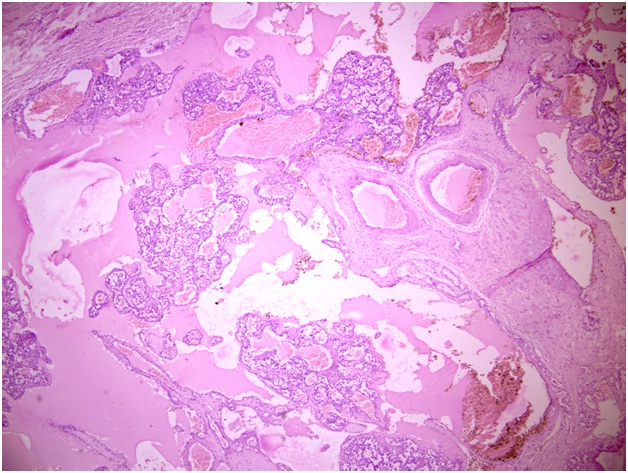
The mass was excised en-bloc under General Anesthesia after ligation of feeder vessels, with an uneventful postoperative recovery. Histopathological analysis revealed scattered skeletal muscle interspersed with thin-walled vessels, consistent with intramuscular capillary haemangioma [Table/Fig-3]. The patient has been regularly following up for 16 months with no evidence of local recurrence.
Histopathological examination (H&E Stain) reveals scattered skeletal muscle interspersed with thin-walled vessels, consistent with intramuscular capillary haemangioma (10X magnification).
Discussion
An Intra Muscular Haemangioma (IMH) is a benign mesenchymal tumour of the endothelial cells. Accounting for only 0.8% of all haemangiomas. A total of 14% of IMH have been reported in the head and neck region, with the masseter (36%) and trapezius (24%) being the most commonly affected muscles [1]. IMH of the temporalis muscle is extremely rare with only 21 well documented cases in international literature, and only three reported cases of intramuscular capillary haemangioma [Table/Fig-4] [2–4].
Details of reported cases of intramuscular capillary haemangioma in english literature [2–4].
| Case | Author/Year | Age (years)/Sex | Treatment |
|---|
| 1 | Sharma et al., 1991 [2] | 21/M | Surgery |
| 2 | Benateau et al., 1997 [3] | 61/F | Surgery |
| 3 | Sharma et al., 2001 [4] | 27/M | Surgery |
| 4. | Present case | 5/M | Surgery |
Liston, in 1843, was the first to describe an IMH [5]. In 1972, Allen and Enzinger classified them on the basis of vessel size into capillary, cavernous and mixed types, with capillary variant being the most commonly encountered [6].
A number of theories exist to explain the aetiology of the tumour; however, none are accepted universally till date. It has been hypothesized that these tumours may be of congenital origin due to the high incidence in the early years of life, with trauma and hormonal changes considered as important additional factors for the proliferation of embryonic vascular tissue [1].
IMH often present as a slow growing mass with distinct margins, without pulsations or discolouration of the overlying skin. Due to their rarity and absence of the above-mentioned vascular signs, it is difficult to diagnose IMH without radiological investigations. Due to its presentation as a soft to firm non-tender mobile mass, a number of pathologies may be considered in the differential diagnosis, including enlarged lymph nodes, neurofibroma, lipoma, dermoid cyst, soft-tissue sarcoma, temporal arteritis, and myositis ossificans [1,7]. IMH may be readily differentiated from these pathologies with the help of different modes of imaging. Computed tomography helps to define the size and relations of the tumour. Magnetic Resonance Imaging (MRI) is more useful in defining its vascular nature, with the tumour appearing hyperintense on T2-weighted imaging due to volume of stagnant blood that is easily distinguished from surrounding muscle [8]. Angiography helps to detect feeder vessels, and is useful for planning preoperative embolization.
To the best of our knowledge, only 25 cases of intramuscular haemangioma of temporalis have been reported in English literature, only 21 of which are well documented [7]. Majority of these cases (85.6%) were either mixed or cavernous haemangiomas, with only three cases of capillary type (14.4%). A slight female predominance was seen (sex ratio of 0.82), with a mean age of 33.7 years [7]. Generally, surgical excision along with a rim of normal tissue was the mainstay of treatment in majority of the cases, with only one case kept under long-term follow-up without surgical intervention. Use of corticosteroids, sclerosing agents and radiotherapy have also been proposed in the past as an alternative or adjunct to surgical excision for reduction in tumour bulk [9].
Local recurrences have been reported, and are more common with the mixed (28%) and capillary varieties (20%); only 9% of cavernous types recurred [10].
Conclusion
Intramuscular haemangioma of the temporal region, although rare, is an important differential diagnosis that must be kept in mind when dealing with a post-aural swelling. The importance of identifying them lies in their ease of excision once the feeding vessels are identified and ligated, and the possibility of local recurrence is long term, especially in the capillary or mixed varieties. Thus, a meticulous long-term clinical and radiological follow-up is necessary in cases of IMH.
[1]. Bucci T, De Giulio F, Romano A, Insabato L, Califano L, Cavernous haemangioma of the temporalis muscle: case report and review of the literatureActa Otorhinolaryngol Ital 2008 28(2):83-86. [Google Scholar]
[2]. Sharma BS, Chari PS, Joshi K, Rajvanshi A, Haemangioma of the temporalis muscleAnn Otol Rhinol Laryngol 1991 100:76-78. [Google Scholar]
[3]. Benateau H, Labbe D, Kaluzinski E, Theron J, Mandard JC, Compere JF, Intramuscular capillary-venous angioma extending into the infratemporal fossa. A propos of a caseRev Stomatol Chir Maxillofac 1997 98:258-62. [Google Scholar]
[4]. Sharma RR, Netalkar AS, Pawar SJ, Musa MM, Lad SD, Congenital and late-onset primary haemangiomas of the temporalis muscle: case reportBr J Oral Maxillofac Surg 2001 39:52-54. [Google Scholar]
[5]. Liston R, Case of erectile tumour in the popliteal space: removalMed Chir Trans 1843 26:120-32. [Google Scholar]
[6]. Allen PW, Enzinger FM, Haemangioma of skeletal muscle. An analysis of 89 casesCancer 1972 29:8-22. [Google Scholar]
[7]. Kim JH, Lew BL, Sim WY, Intramuscular vascular malformation of the temporalis muscle: A case report and review of the literatureAnn Dermatol 2014 26(3):428-30. [Google Scholar]
[8]. Buetow PC, Kransdorf MJ, Moser RP, Jelinek JS, Berrey BH, Radiologic appearance of intramuscular haemangioma with emphasis on MR imagingAm J Roentgenol 1990 154:563-67. [Google Scholar]
[9]. Giudice M, Piazza C, Bolzoni A, Peretti G, Head and neck intramuscular haemangioma: report of two cases with unusual localizationEur Arch Otorhinolaryngol 2003 260:498-501. [Google Scholar]
[10]. Lopez-Cedrun JL, Urtasun Fernandez J, Melendez Baltanas J, Lopez Garcia JA, Haemangioma of the temporalis muscle: a case report and review of the literatureJ Oral Maxillofac Surg 1996 54:1130-32. [Google Scholar]