Acute appendicitis is the most common indication for emergent surgery and affects a wide range of patients at any age group. The lifetime risk of appendicitis is 8.6% for males and 6.7% for females, and the lifetime risk of appendectomy is 12.0% for males and 23.1% for females [1]. Inspite of the presence of various imaging modalities, biochemical markers, and scoring systems the negative appendectomy rate remain high. Laboratory studies along with the clinical presentation can help in the diagnosis of acute appendicitis. However, all clinical and laboratory variables are weak discriminators individually though they can achieve a high discriminatory power when combined.
It is well known that serum fibrinogen is an acute inflammatory mediator. The level of serum fibrinogen is usually raised in any acute inflammatory condition and the same is expected to rise in acute appendicitis also. It is already proven and known that the level of serum fibrinogen is raised in certain acute conditions like acute myocardial infarction and acute cerebrovascular incidents [2]. Apart from its action on hemostasis, the fibrinopeptide can operate as a chemoattractant and has the potent activity to recruit both Polymorpho Nuclear cells (PMN) and fibroblast [3]. Fibrinogen-related proteins are an important participants in leukocyte trafficking and tissue remodeling. They are involved in the signaling and activation of mononuclear phagocytes from altered coagulation or fibrinolysis in an inflamed tissue or organ [4].
Many attempts have been made to determine ways of decreasing the negative laparotomy rate in clinically suspected acute appendicitis. Unfortunately, there is no single laboratory value for true, certain and specific diagnosis of appendicitis. In medical practice, leukocyte and left shift are the most widely used laboratory parameters in the diagnosis of appendicitis, and although they can be helpful in the diagnosis and exclusion of appendicitis they are not absolute [5]. Although the influence and utility of C-reactive protein on diagnostic decision-making has not been investigated much, yet the available resource shows that it has relatively low specificity and sensitivity. The level of C-reactive protein alone does not influence the decision to confirm or exclude the diagnosis of acute appendicitis safely or sufficiently [6,7]. Thus, a stronger parameter of confidence in doubtful cases is needed.
Some studies were also conducted which showed that the rate of negative appendectomy can be reduced further if the level of serum fibrinogen is also taken into consideration [8–10]. Thus, this study was undertaken to determine the predictive value of serum fibrinogen level in deciding immediate appendectomy or otherwise so as to minimize the negative appendectomy rate.
Materials and Methods
A cross-sectional study was conducted on 82 patients, who were admitted with clinical signs and symptoms suggestive of acute appendicitis and who underwent emergency appendectomy in the Department of Surgery, Regional Institute of Medical Sciences, Imphal, Manipur, India, from October 2013 to September 2015. Approval of the Institutional Ethical Committee and informed consent were taken from all the participants.
Inclusion Criteria: All patients presenting with signs and symptoms suggestive of acute appendicitis and all cases of acute abdomen with USG/CT findings suggestive of acute appendicitis and who underwent emergency appendectomy.
Exclusion Criteria: Patients found to be suffering from other acute infections, those patients found to be having acute appendicitis but managed conservatively.
Clinical signs and symptoms and white blood cell count were taken into consideration. Patient symptoms included migratory pain, anorexia, right lower quadrant pain, nausea, vomiting, body temperature >37.3°C. Ultrasound of the abdomen was done in all patients. All removed appendix specimens were examined by a routine protocol and the final diagnosis was based on the histopathological results.
Blood samples, 1.8 ml for determining the serum fibrinogen level were collected personally in a sodium citrate vial 30 minutes before the surgical procedure. The fibrinogen level was measured in the Fibrinogen (FBG) program on the semi-automated instrument-coagulometer (CA-50-Sysmex). All patients underwent open appendectomy and the appendix specimen sent for histopathological evaluation.
Statistical Analysis
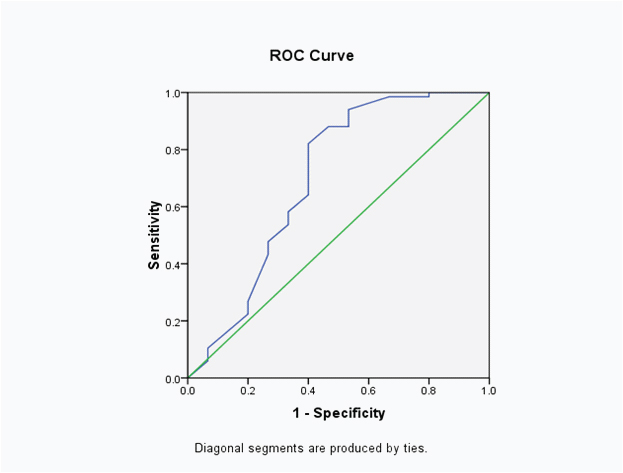
Statistical analysis was done by using data based programme. Descriptive statistics such as mean, standard deviation and percentage were used. Receiver Operating Characteristic (ROC) curves and the related areas under the curve were calculated [Table/Fig-1]. The result of the study was interpreted using SPSS version 20.0 software. A p-value of <0.05 was taken as significant.
ROC of fibrinogen level against HPE report.
Results
A total number of 82 patients suspected to be suffering from acute appendicitis who underwent emergency appendectomy were studied and the sensitivity, specificity, p-value calculated. The age distribution, clinical features and total leukocyte count were also evaluated. The serum fibrinogen level was evaluated and cut off value was taken at different levels.
The patient’s age ranged from 10 to 63 years. The majority of the patients were from the age group 10-20 years (28.1%) followed by 21-30 years (26.8%). Mean age was 37.26 years with a standard deviation of 1.6 years.
All the respondents presented with pain in the right iliac fossa (100%), anorexia, nausea and vomiting and migratory pain were present in 98.8%, 79.3 %, 70.3 % and 50% respectively. Leucocyte count was found normal in 19.7% and raised leucocyte count was observed in 80.3%.
Majority of the patients on gross intraoperative evaluation were found to be suffering from uncomplicated appendicitis (63.4%). Complicated appendicitis which includes ruptured appendix and gangrenous appendix were found to be present in 30.4%, and grossly normal looking appendix was found in 6.2%. On histopathological examination 18.3% (n=15) of the had normal appendix while 81.7% (n=67) had acute appendicitis.
The normal serum fibrinogen level was taken a 400 mg/dl. The mean fibrinogen level was found to be higher in patient with acute appendicitis (436.6±40.6) than those with normal appendicitis (391.91±66.54), on analysis it was found to be statistically significant (p<0.05) as shown on [Table/Fig-2].
Fibrinogen levels in acute appendicitis and normal appendicitis patients.
| HPE report | Fibrinogen Mean±SD | T-test |
|---|
| Acute appendicitis | 436.6±40.6 | t= 3.418p-0.001 |
| Normal appendix | 391.91±66.54 |
HPE-Histopathological examination
The area under the ROC curve was 0.697 i.e., it has an accuracy of around 70% and this was statistically significant (p=0.018). On further sub-analysis when the cut off level of fibrinogen level was reduced to 397 it was found that the sensitivity increases to 82% with a specificity of 60% and if the level was further lowered to 375 then it gives a sensitivity of 88% and specificity of 55%.
Discussion
The study investigated the role of serum fibrinogen level in the diagnosis of acute appendicitis and to see whether it can play an important role in reducing the negative appendectomy rate. The study was designed to find out the sensitivity and specificity of serum fibrinogen level in the diagnosis of acute appendicitis and to study the correlation of serum fibrinogen level with the incidence of negative appendectomy rate.
Early diagnosis of acute appendicitis is not always easy as it appear to be. It poses a serious dilemma to surgeons regarding the decision to observe the patient until the diagnosis is confirmed or to operate early to prevent complications like perforation and peritonitis. It therefore, becomes very important to differentiate early appendicitis from other causes of acute abdominal pathologies. Acute appendicitis remains a diagnostic challenge as indicated by the high rate of unnecessary surgery. Although in recent years progress in diagnostic techniques with detailed history, physical examinations and laboratory studies has resulted in a decrease in the number of perforations and negative appendectomies, it is still inevitable to face difficulty in the diagnosis of atypical cases, and the challenge whether to observe or to operate with atypical signs still remains, and furthermore, a delay in the diagnosis and failure to act promptly and operate will do more harm than good and may lead to a devastating morbidity and mortality which otherwise could have been averted. However, routine early operation may also result in the removal of a normal appendix with a small risk of morbidity [11].
In our study, the maximum numbers of patients with appendicitis were in the age group of <30 years (54.9%). Similar findings were also reported by Murata A et al., [12]. In our study although the total leucocyte count was increased in maximum of the cases yet in 19.7% of the cases it remained normal, and although the clinical interpretation can give a strong indication in the diagnosis as well as in deciding whether to manage the patient conservatively or to go for surgery, yet it alone cannot be relied upon safely. We also found that most of the patients have a variety of symptoms and the severity by clinical judgment alone can lead to a poor or fatal outcome as it will depend on the patient’s tolerance.
In our study it was observed that 15 (18.3%) patients out of the 82 patients who underwent appendectomy had a normal appendix on histopathological examination. Thus the rate of negative appendectomy in our study was 18.3% which is on the higher side as compared to other studies [13]. However, the negative appendectomy rate varies in different studies [14]. The higher negative appendectomy rate in our study as compared to others could be due to lesser implementation of CT scan or due to inadequate diagnostic work up prior to surgery, and in all these patients the serum fibrinogen level was found to be normal. Had the serum fibrinogen value been taken into consideration prior to the decision to go for surgery, the possibility of the issue of high negative appendectomy could have been averted and the rate of negative appendectomy rate would have reduced further. The Mean±SD of serum fibrinogen in mg/dl in our study in those patient proved to be having acute appendicitis by histopathology was 436.6±40.6 while those with normal appendix was 391.91±66.54. Based on our study the area under the curve is 0.697 i.e., it has an accuracy of around 70% and this is statistically significant (p=0.018). If the cut off level of fibrinogen level is reduced to 397 then it increases the sensitivity to 82% with a specificity of 60% and if the level is reduced further to 375 it gives a sensitivity of 88% and specificity of 55%. Similar findings were also reported in other studies where they found that the serum fibrinogen level when taken into consideration along with other diagnostic tools for acute appendicitis helps in reducing the negative appendectomy rate [8–10]. The diagnostic factor is found more significant in a complicated appendicitis [15].
Our results suggest that the use of fibrinogen blood level may be a new diagnostic acute-phase reactant in the diagnosis of acute appendicitis that may be helpful in deciding whether to operate or to manage non-operatively.
Limitation
However, the sample size is less, further larger series studies are needed to confirm our finding, and also, an ideal cut off level of serum fibrinogen needs to be ascertained.
Conclusion
Acute appendicitis still remain the most common surgical condition which requires immediate intervention and early diagnosis plays a vital role in preventing simple appendicitis from complicating. But as the dilemma in decision-making still persists, the surgeon must take every possible additional information, so as to come out with the best possible result. As our study suggests, the serum fibrinogen level may be used as a new inflammatory marker in the diagnosis and more importantly in decision making of management of acute appendicitis.
HPE-Histopathological examination