Introduction
The emergence and spread of Multi-Drug Resistant (MDR) Non-Fermenting Gram-Negative Bacilli (NFGNB) in Intensive Care Units (ICU) and their genetic potential to transmit diverse antibiotic resistance regardless of their ability to ferment glucose poses a major threat in hospitals. The complex interplay of clonal spread, persistence, transmission of resistance elements and cell-cell interaction leads to the difficulty in controlling infections caused by these multi drug-resistant strains. Among non-fermenting Gram-negative rods, the most clinically significant species Pseudomonas aeruginosa, Acinetobacter baumannii and Stenotrophomonas maltophilia are increasingly acquiring resistant to carbapenems. Carbapenems once considered as a backbone of treatment of life threatening infections appears to be broken as the resistance to carbapenems is on rise.
Aim
To document the prevalence of carbapenem resistance in non-fermenting Gram-negative bacilli isolated from patients with respiratory tract infections in the ICU of Himalayan Institute of Medical Sciences, Dehradun.
Materials and Methods
This is a cross-sectional study conducted in ICU patients between October 2015 to March 2016. A total of 366 lower respiratory tract samples were collected from 356 patients with clinical evidence of lower respiratory tract infections in form of Endotracheal (ET) aspirate, Tracheal Tube (TT) aspirate and Bronchoalveolar Lavage (BAL) specimen. Organism identification and the susceptibility testing was done by using an automated system VITEK 2.
Results
Out of 366 samples received 99 NFGNB were isolated and most common sample was ET aspirate sample 256 (64.5%). Acinetobacter baumannii was the most common NFGNB isolated 63 (63.63%) followed by Pseudomonas aeruginosa 25 (25.25%), Elizabethkingia meningoseptica seven (7.07%) and Strenotrophomonas maltophilia four (4.04%). We observed that 90.5% Acinetobacter baumannii were resistant to imipenem and 95.2% resistant to meropenem, Pseudomonas aeruginosa came out to be 52% resistant to imipenem and 56% resistant to meropenem while Stenotrophomonas maltophilia and Elizabethkingia meningoseptica were 100% resistant to carbapenems as they are intrinsically resistant to carbapenems.
Conclusion
The resistance rate of carbapenems for NFGNB infections is very high in our study and variable in different regions. Overall carbapenem resistance is on rise. So, the infection control team and microbiologist needs to work together to determine the risk carried by multi drug resistant non-fermenting gram-negative infections and the resistance surveillance programs are mandatory to control these bacteria in ICU settings.
Acinetobacter, Imipenem, Meropenem, VITEK 2
Introduction
NFGNB are aerobic, Gram-negative, non-motile, non-lactose fermenting, oxidase-negative, catalase-positive coccobacilli which are developing as a major threat to critically ill patients [1]. NFGNB which are often neglected are increasingly acquiring resistance to carbapenems [2]. These organisms have potential to cause, difficult to treat life threatening infections, often in immunosuppressed patients with multiple co-morbidities [3]. They are intrinsically resistant to multiple antibiotics and carbapenems are frequently used for these treatment.
The rate of carbapenem resistance in NFGNB is gradually increasing worldwide and vary geographically [4,5]. Mechanism of carbapenem resistance in non-fermenting Gram-negative bacilli occurs by various mechanisms including carbapenemase production, decrease permeability due to loss of porin channels, overexpression of efflux pump and changes in penicillin binding proteins [6]. The prevalence of Carbapenem Resistant Acinetobacter (CRA) has increased alarmingly up to 85% in the ICUs after the first reported case in 1991 from the United States [7–9]. Unfortunately, there is paucity of data on the prevalence of carbapenem resistant NFGNB infections in the Indian literature [10]. Here, we document the microbiological aspects of the prevalence of carbapenem resistance in NFGNB, isolated from patients with respiratory tract infections in the ICU.
Materials and Methods
This is a cross-sectional study conducted in ICU of a multi-speciality hospital of Uttarakhand, India, after taking approval from Research and Ethical Committee of our institute. A total of 366 samples were collected from 356 patients of all age groups and both sex with clinical evidence of lower respiratory tract infections, admitted to ICU during October 2015 to March 2016. The samples were collected from those patients who develop new onset of fever with rise in Total Leukocyte Count (TLC), change in amount and consistency of lower respiratory tract secretions and new onset developing infiltrates in chest X-ray. Ten patients had prolonged ICU stay that developed multiple times lower respiratory tract infection, so repeated samples were send for those patients. Specimens were collected before antibiotic administration. Samples like endotracheal aspirates or tracheal tube aspirates from patients on ventilators and BAL samples were collected in sterile universal containers. Endotracheal aspirates were collected by using sterile 12 gauge endotracheal suction catheter tube connected to suction pump passed through endotracheal tube. Samples were transported immediately within 15 minutes to microbiology laboratory and processed. Samples that were not representative of lower respiratory tract were excluded from the study.
Microbiological Processing:
The ET secretion, BAL and TT secretion specimens received in the microbiology section was assessed for composite quality score by making a Gram-stain smear [11]. After confirming the sample to be representative of lower respiratory tract secretion the samples were plated on Sheep Blood Agar (SBA), Chocolate Agar (CA), and Mac-Conkey Agar (MA) by using 4 mm nichrome wire loop (Hi-media, Mumbai, India), which holds 0.01 ml of sample. All plates were incubated overnight at 37°C and chocolate agar plates at 37°C in 5% CO2 incubator. Plates were incubated for 18-24 hours at 37°C. Threshold for quantitative cultures was considered as 105 CFU/ml. Growth of any organism below the threshold was assumed as colonization or contamination. Organisms identification and antimicrobial susceptibility tests was carried out by using an automated system VITEK 2 for amikacin, amoxicillin-clavulanic acid, aztreonam, cefepime, cefotaxime, ceftazidime, ceftriaxone, ciprofloxacin, ertapenem, gentamycin, imipenem, levofloxacin, meropenem, piperacillin-tazobactam, trimethoprim-sulfamethoxazole and colistin. Pseudomonas aeruginosa (ATCC-27853) was used as quality control strain. The result of susceptibility testing was interpreted as per Clinical and Laboratory Standards Institute (CLSI 2014) guidelines [12].
The interpretation and analysis of the data obtained were done by using Microsoft Excel and SPSS version 22.0. The quantitative data was expressed as frequency, percentages and graphical representation.
Results
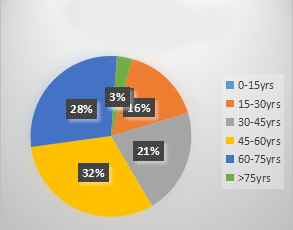
In our study out of 236 ET aspirates, 64 TT secretions and 66 BAL samples received, 99 came out to be positive for NFGNB infections. A total of 156 samples were positive for other organisms and 111 samples were negative for any growth of bacteria. Lower respiratory infections with NFGNB was more in males (77%) as compared to females (23%) and more common in elderly age group in range of 45-75 years as shown in [Table/Fig-1]. These infections were more common in medical patients with co-morbid illness. Out of NFGNB infections Acinetobacter baumannii was most common bacteria isolated 63 (63.63%) which was followed by Pseudomonas aeruginosa 25 (25.25%), Elizabethkingia meningoseptica 7 (7.07%) and Stenotrophomonas maltophilia 4 (4.04%) as shown in [Table/Fig-2].
Age wise distribution of patients.
0 to 15 years - percentage is zero as there were no paediatric patients
Percentages of NFGNB isolated.
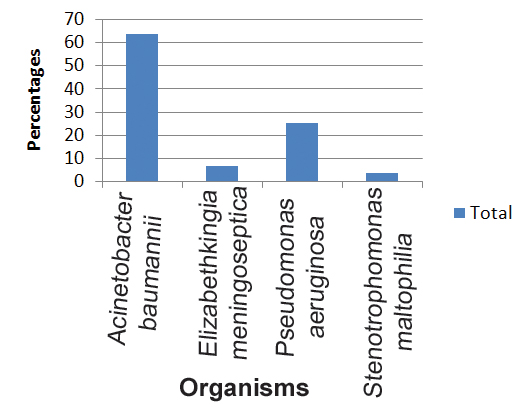
The most alarming was the carbapenem resistance, which is considered as last choice in life threatening infection. We observed an overall of 81.8% resistance to imipenem and 85.8% to meropenem exhibited by our NFGNB isolates. Resistances for carbapenems by different NFGNBs are shown in [Table/Fig-3]. The antibiotic susceptibility pattern for NFGNBs showed that all the isolates were uniformly sensitive to colistin (100%) except Elizabethkingia meningoseptica. However, high rates of resistance was observed for other antibiotics like amikacin 69 (69.69%), gentamycin 82 (82.82%), amoxicillin-clavulanic acid 90(90.9%), aztreonam 94 (94.94%), cefepime 84 (84.84%), cefotaxime 95(95.95%), ceftazidime 86(86.86%), ceftriaxone 99 (100%), ciprofloxacin 99 (100%), levofloxacin 92 (92.92%), piperacillin-tazobactam 82 (82.82%) and trimethoprim-sulfamethoxazole 89 (89.89%).
Percentage of carbapenem resistance in nonfermenting Gram-negative organisms.
| Micro-organism | Imipenem | Meropenem | Ertapenem |
|---|
| Acinetobacter baumannii | 90.54% | 95.2% | NA |
| Pseudomonas aeruginosa | 52% | 56% | NA |
| Elizabethkingia meningoseptica | 100% | 100% | 100% |
| Stenotrophomonas maltophilia | 100% | 100% | 100% |
Discussion
Carbapenems since they were first introduced in 1980’s were considered as backbone antibiotic therapy in case of life threatening serious infections in ICU settings [13]. Gradually resistance to carbapenems started coming up after it was first reported in 1991 in USA which is now a serious problem in ICUs [1]. NFGNB are saprophytes but have potential to cause opportunistic life threatening serious infections, often in immunocompromised and critically ill patients [14]. These non fermenters are often multidrug resistant with limited therapeutic options and the resistance pattern is increasing over last two decades [15]. They can also transfer the resistance to susceptible organism by gene transfer [16]. Documentation of carbapenem resistance in NFGNB is important as they can cause outbreaks in ICU settings which adds on to morbidity and mortality in patients with underlying diseases. Regular monitoring and documentation of carbapenem resistance help us to judiciously use antibiotics and developing strategies to control infections.
Acinetobacter baumannii and Pseudomonas aeruginosa are well established health care associated pathogens due to their ability to develop resistance to various antibiotics including carbapenems by various mechanisms [17]. Isolation of Acinetobacter baumannii and Pseudomonas aeruginosa as the most common NFGNB has been increasingly reported in the literature [17–19]. In our study also, the most common NFGNB isolated was Acinetobacter baumannii 63 (63.63%) followed by Pseudomonas aeruginosa 25 (25.25%).
The antimicrobial resistance pattern of the NFGNBs varies widely from hospital to hospital in different geographical region. Imipenem being a commonly used carbapenem in ICU settings, resistance exhibited by various NFGNBs against this carbapenem has been reported by many Indian authors which is shown in [Table/Fig-4] [18–25]. In our study, we observed a high resistance to imipenem by Acinetobacter isolates (90.54%), while 52% of Pseudomonas aeruginosa isolates were imipenem resistant. Frequent use of imipenem might attribute to the high resistant against imipenem in our NFGNB isolates. Nosocomial infections with carbapenem resistant strains is favoured by selection pressure of previously used antibiotics and also related to duration of ICU stay [26]. Baumgart AMK et al., reported that carbapenem resistance of Acinetobacter is on rise and 77% and 80% of Acinetobacter isolates were resistant against imipenem and meropenem respectively [27]. However, Memish ZA, et al., showed very low (5.4%) imipenem resistance Acinetobacter which is probably due to selection of all the samples of NFGNB and most of the patients they received were mostly directly from community [28].
Data of carbapenem (imipenem) resistance from different regions of India [18–25].
| Author | Region | Year | Imipenem resistant A. baumannii | Imipenem resistant P. aeruginosa | Imipenem resistant S. maltophilia |
|---|
| Rit Ket al., [19] | Eastern India | 2013 | 55% | 8.2% | 100% |
| Gurjar M et al., [20] | Lucknow | 2013 | 75% | - | - |
| Benachinmardi, KK., [21] | Bengaluru | 2014 | 59% | 20% | - |
| Sharma Det al., [22] | Jaipur | 2014 | 81% | 80% | 62% |
| Kombade Set al., [23] | Nagpur | 2015 | 60% | 90% | 20% |
| Devi PV et al., [18] | Nellore, AP | 2015 | 28% | 42% | - |
| Ashwani Jet al., [24] | Raigarh, CH | 2015 | 3.5% | 10.3% | - |
| Ahmed NHet al., [25] | Central India | 2015 | 53% | 29% | - |
| Present study | Dehradun | 2015/ 2016 | 90.54% | 52% | 100% |
Stenotrophomonas maltophilia is an emerging multidrug-resistant opportunistic pathogen [29]. The increasing incidence of nosocomial and community-acquired S. maltophilia infections is of concern to the clinicians especially in case of immunocompromised individuals, as this pathogen is associated with a significant mortality. S. maltophilia was first isolated in 1943 as Bacterium bookeri and then named Pseudomonas maltophilia [30]. Data from the SENTRY Antimicrobial Surveillance Program during 1997 to 2008 showed that 3.1% of S. maltophilia were recovered from hospitalized patients with pneumonia from 2004 to 2008, with regional recovery rates of 3.3% for the United States, 3.2% for Europe, and 2.3% for Latin America [31]. S. maltophilia can form biofilms on lung cells [32]. In our study Stenotrophomonas was isolated in 4.04% cases. There has been an increase in antimicrobial resistance of S. maltophilia over recent years, notably to Trimethoprim-Sulfamethoxazole (TMX), once a preferred treatment for S. maltophilia infections [33]. In a 2012 study of S. maltophilia recovered from cystic fibrosis patients, 24.2% of the patients had TMX resistant isolates [34]. They are intrinsically resistant to imipenem and overuse of carbapenems has led to the emergence of Stenotrophomonas infections in hospital environment because of selection pressure [35]. In our study they were 100% resistant to carbapenems.
Elizabethkingia meningoseptica has been considered as a potentially important threat to patients in critical care areas because of its multidrug-resistant pattern and its ability to adapt to various environments [36]. Elizabethkingia meningoseptica possess two different types of beta-lactamases, namely class A Extended-Spectrum β-Lactamases (ESBL) and class B Metallo β-Lactamases (MBLs); the latter confer resistance to carbapenems, which are widely used to treat life threatening Gram-negative infections. They are intrinsically resistant to multiple antibiotic classes and have unusual resistance patterns and mechanisms [37]. Colistin overuse has acted as a selective factor that allowed E. meningoseptica to emerge in the hospital. In our study Elizabethkingia meningoseptica is 100% resistant to carbapenems.
Limitation
Limitation of our study was that we could not confirm the mechanism of carbapenem resistance in our isolates by molecular methods which would have helped in developing novel therapeutic strategies for combating these infections.
Conclusion
Our study highlights the high prevalence of carbapenem resistance NFGNB among the clinical isolates of our ICU. In view of this high carbapenem resistance amongst the isolates, there is a need to emphasize on strict adherence to the concept of “reserve drugs” and antibiotic therapy should be advocated or modified following culture and sensitivity. This would not only help in the proper treatment of the patient but also would discourage the indiscriminate use of available antibiotics and curtail the spread of drug resistance bacteria. Moreover, considering the prevalence of carbapenem resistant bacteria, it is necessary to carry out regular monitoring of drug resistance and molecular characteristics of carbapenem resistant isolates in this region.
[1]. Kim UJ, Kim HK, An JH, Cho SK, Park KH, Jang HC, Update on the epidemiology, treatment, and outcomes of carbapenem-resistant acinetobacter infectionsChonnam Med J 2014 50(2):37-44. [Google Scholar]
[2]. Gniadek TJ, Carroll KC, Simner PJ, Carbapenem-resistant non-glucose-fermenting Gram-negative bacilli: The missing piece to the puzzleJ Clin Microbiol 2016 54(7):1700-10. [Google Scholar]
[3]. Rampal R, Infections due to the Pseudomonas species and related organisms. Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL editorsIn: Harrison’s principles of Internal Medicine 2008 17th edUSAMcGraw-Hill Medical:949-56. [Google Scholar]
[4]. Center for Disease Control and Prevention 2013. Antibiotic resistance threats in the United States, 2013. Centres for disease control and prevention Atlanta, GA [Google Scholar]
[5]. Kim YJ, Kim SI, Hong KW, Kim YR, Park YJ, Kang MW, Risk factors for mortality in patients with carbapenem-resistant Acinetobacter baumannii bacteremia: Impact of appropriate antimicrobial therapyJ Korean Med Sci 2012 27(5):471-75. [Google Scholar]
[6]. Meletis G, Exindari M, Vavatsi N, sofianou D, Diza E, Mechanism responsible for the development of resistance in Pseudomonas aeruginosaHippocrata 2012 16:303-07. [Google Scholar]
[7]. Dizbay M, Tunccan OG, Sezer BE, Hizel K, Nosocomial imipenem resistant Acinetobacter baumannii infections: Epidemiology and risk factorsScand J Infect Dis 2010 42:741-46. [Google Scholar]
[8]. Manchanda V, Sinha S, Singh NP, Multidrug resistant AcinetobacterJ Global Infect Dis 2010 2:291-304. [Google Scholar]
[9]. Mera RM, Miller LA, Amrine MH, Sahm DF, Acinetobacter baumannii 2002-2008: Increase of carbapenem associated multiclass resistance in the United StatesMicrob Drug Resist 2010 16:209-15. [Google Scholar]
[10]. Porwal R, Gopalakrishnan R, Rajesh NJ, Ramasubramanian V, Carbapenem resistant gram-negative bacteremia in an Indian intensive care unit: A review of the clinical profile and treatment outcome of 50 patientsIndian J Crit Care Med 2014 18(11):750-53. [Google Scholar]
[11]. Forbes BA, Sahm DF, Weissfeld AS, Infections of the lower respiratory tract. In: Forbes BA, Sahm DF, Weissfeld AS, editorsBailey and Scott’s Diagnostic Microbiology 2007 12th edNew YorkMosby Elevier:798-807. [Google Scholar]
[12]. Clinical Laboratory Standard Institute. Performance standards for antimicrobial susceptibility testing: Twenty-fourth informational supplement. CLSI document M100–S24. Clinical Laboratory Standards Institute, Wayne, PA 19087, USA. 2014 [Google Scholar]
[13]. Go ES, Urban C, Burns J, Kreiswirth B, Eisner W, Clinical and molecular epidemiology of Acinetobacter infections sensitive only to polymyxin B and sulbactamLancet 1994 344:1329-32. [Google Scholar]
[14]. Perween N, Sehgal S, Prakash SK, Geographical patterns in antimicrobial resistance of acinetobacter in clinical isolatesJ Clin Diagn Res 2014 8(4):DC10-DC12. [Google Scholar]
[15]. Tripathi PC, Gajbhiye SR, Agrawal GN, Clinical and antimicrobial profile of Acinetobacter spp: An emerging nosocomial superbugAdv Biomed Res 2014 9(3):13 [Google Scholar]
[16]. Wendel AF, Brodner AH, Wydra S, Ressina S, Henrich B, Pfeffer K, Genetic charecterization and the emergence of metallo -beta-lactamase GIM 1 in Pseudomonas species and enterobacteriaceae during a long- term outbreakAntimicrobial Agent Chemother 2013 57:5162-65. [Google Scholar]
[17]. Malini A, Deepa EK, Gokul BN, Prasad SR, Nonfermenting gram-negative bacilli infections in a tertiary care hospital in Kolar, KarnatakaJ Lab Physicians 2009 1(2):62-66. [Google Scholar]
[18]. Devi PV, Reddy PS, John MS, Incidence of carbapenem resistant nonfermenting gram-negative bacilli from patients with respiratory tract infections among intensive care unitsInt J Res Med Sci 2015 3(6):1368-71. [Google Scholar]
[19]. Rit K, Nag F, Raj HK, Maity PK, Prevalence and susceptibility profiles of nonfermentative gram-negative bacilli infection in a tertiary care hospital of Eastern IndiaIndian Journal of Clinical Practice 2013 24(5):451-55. [Google Scholar]
[20]. Gurjar M, Saigal S, Baronia AK, Rao BP, Azim A, Poddar B, Carbapenem resistant Acinetobacter ventilator associated pneumonia: Clinical characteristics and outcomeIndian Journal of Critical Care Medicine 2013 17(3):129-34. [Google Scholar]
[21]. Benachinmardi KK, Padmavathy M, Malini J, Naveneeth BV, Prevalence of NFGNB and their in vitro susceptibility pattern at a tertiary care teaching hospitalJournal of the Scientific Society 2014 41(3):162-66. [Google Scholar]
[22]. Sharma D, Vyas N, Sinha P, Mathur A, NFGNB as a nosocomial pathogen: Identification and antibiotic sensitivity in clinical samples of indoor patientsNepal Journal of Medical Sciences 2014 3(2):101-05. [Google Scholar]
[23]. Kombade S, Agrawal GN, Study of multidrug resistant nonfermenting gram-negative bacilli in intensive care unit, NagpurIndian J Microbiol Res 2015 2(2):120-25. [Google Scholar]
[24]. Aswani J, Pattanayak M, Sao S, Panda PK, Incidence of carbapenem resistant Pseudomonas aeruginosa isolated from patients with lower respiratory tract infection in intesive care unitsInternational Journal of Scientific Research And Management 2015 3(7):289-92. [Google Scholar]
[25]. Ahmed NH, Hussain T, Biswal I, Antimicrobial resistance of bacterial isolates from respiratory secretions of ventilated patients in a multi-speciality hospitalAvicenna J Med 2015 5(3):74-78. [Google Scholar]
[26]. Baran G, Erbay A, Bodur H, Ongürü P, Akinci E, Balaban N, Risk factors for nosocomial imipenem resistant Acinetobacter baumannii infectionsInt J Infect Dis 2008 12:16-21. [Google Scholar]
[27]. Baumgart AMK, Molinari MA, Silveira AC, Prevalence of carbapenem resistant Pseudomonas aeruginosa and Acinetobacter baumannii in high complexity hospitalBraz J Infect Dis 2010 14(5):433-36. [Google Scholar]
[28]. Memish ZA, Shibl AT, Kambal AM, Ohaly YA, Ishaq A, Livermore DM, Antimicrobial resistance among non-fermenting gram-negative bacteria in Saudi ArabiaJournal of Antimicrobial Chemotherapy 2012 67(7):1701-05. [Google Scholar]
[29]. Brooke JS, Stenotrophomonas maltophilia: An emerging global opportunistic pathogenClin Microbiol Rev 2012 25(1):2-41. [Google Scholar]
[30]. Hugh R, Leifson E, A description of the type strain of Pseudomonas maltophiliaInt Bull Bacteriol Nomencl Taxon 1963 13:133-38. [Google Scholar]
[31]. Jones RN, Microbial etiologies of hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumoniaClin Infect Dis 2010 51:S81-87. [Google Scholar]
[32]. Pompilio A, Crocetta V, Confalone P, Nicoletti M, Petrucca A, Guarnieri S, Adhesion to and biofilm formation on IB3-1 bronchial cells by Stenotrophomonas maltophilia isolates from cystic fibrosis patientsBMC Microbiol 2010 7(10):102 [Google Scholar]
[33]. Goldberg E, Bishara J, Contemporary unconventional clinical use of co-trimoxazoleClin Microbiol Infect 2012 18(1):8-17. [Google Scholar]
[34]. Milne KEN, Gould IM, Combination antimicrobial susceptibility testing of multidrug-resistant Stenotrophomonas maltophilia from cystic fibrosis patientsAntimicrob Agents Chemother 2012 56(8):4071-77. [Google Scholar]
[35]. Sanyal SC, Mokaddas EM, The increase in carbapenem use and emergence of Stenotrophomonas maltophilia as an important nosocomial pathogenJournal of Chemotherapy 1999 11(1):28-33. [Google Scholar]
[36]. Jean SS, Lee WS, Chen FL, Ou TY, Hsueh PR, Elizabethkingia meningoseptica: An important emerging pathogen causing healthcare-associated infectionsJ Hosp Infect 2014 86(4):244-49. [Google Scholar]
[37]. González LJ, Vila AJ, Carbapenem resistance in Elizabethkingia meningoseptica is mediated by metallo-β-lactamase BlaBAntimicrob Agents Chemother 2012 56(4):1686-92. [Google Scholar]