Pseudoexfoliation (PEX) syndrome is an age-related disorder characterized by the production and progressive accumulation of fibrillar-granular extracellular material in many ocular tissues [1]. Although it has been known since the beginning of the 20th century, the exact aetiopathogenesis of this condition still remains elusive. In the ocular tissues, PEX is characterized clinically by whitish flaky deposits, most commonly on the pupillary margin and the anterior lens capsule. However, it is also deposited on the corneal endothelium, trabecular meshwork, ciliary body, ciliary zonules and even the anterior vitreous [1]. Pigment loss from the iris sphincter region and its deposition on anterior chamber structures support the diagnosis [2].
Patients with PEX syndrome have a significantly higher risk of a variety of complications during cataract surgery owing to the omnipresence of PEX material in the anterior segment. These include intra-operative problems such as corneal endotheliopathy, small pupil, zonular weakness, posterior capsule dehiscence, vitreous loss, etc. In addition, post-operative spectrum of complications includes post-operative Intra-ocular Pressure (IOP) spike, corneal oedema, posterior capsular opacification, anterior capsular phimosis, macular oedema, etc. [3]. In developing countries like India, both Phacoemulsification (PHACO) and manual Small Incision Cataract Surgery (SICS) are among the most common procedures performed for cataract extraction. In the setting of PEX syndrome, both these procedures are fraught with risks. Meticulous pre-operative planning and modification of intra-operative techniques can help reduce the incidence of complications.
So much said and done, dilemma exists regarding multiple facets of this entity. Existing techniques for cataract surgery in the presence of PEX continue to be modified and newer techniques continue to be devised. However, no single surgical technique has been conclusively proven to be safe for cataract extraction in presence of PEX syndrome. Ours being a major tertiary care government ophthalmological institute in India, a fairly large number of cataract patients with PEX syndrome are encountered on a daily basis. Many studies [4–16] have analyzed the efficacy of SICS, Extracapsular Cataract Extraction (ECCE) and PHACO in PEX syndrome. However, to our knowledge, no study has directly compared SICS to PHACO with regards to safety and visual outcome. Hence, we decided to conduct a comparative pilot study analysing the visual outcome of PHACO versus SICS in the combined setting of cataract and PEX syndrome.
Materials and Methods
A prospective, observational pilot study was conducted in the ophthalmology department of a tertiary care government ophthalmological institute in India over a period of six months from July 2014 to December 2014. Prior permission to conduct the study was obtained from the Institutional Clinical Ethics Committee. A total of 200 eyes of 100 conveniently sampled patients aged 40 years and above, of either sex, clinically diagnosed (on the basis of slit-lamp biomicroscopy before and after pupillary mydriasis) to have senile cataract and PEX syndrome were enrolled in the study. Written, informed consent was obtained from all enrolled subjects.
Exclusion criteria were as follows:
Patients below the age of 40 years
Patients with any other form of lens opacity except senile cataract.
Patients with any other ocular pathology except senile uncomplicated cataract and PEX syndrome. Thus, patients with pre-existing PXS induced complications such as subluxated/dislocated cataract, zonular dialysis and PEX glaucoma were excluded.
Patient with any other known ocular, systemic medical/ surgical/ psychiatric diseases that were likely to confound visual outcome.
Patients with a history of previous ocular medications, surgery or trauma.
Patients not willing to give voluntary written consent.
The enrolled subjects were matched for age and sex and randomly divided into two groups. Patients in Group-1 underwent temporal limbal incision based PHACO while those in Group-2 underwent manual SICS – henceforth referred to as PHACO group and SICS groups respectively. No patient was lost to follow-up. The primary outcome measure was safety of the two procedures defined by the incidence of intra-operative and post-operative complications.
Pre-operative evaluation: Best Corrected Visual Acuity (BCVA) for distance was recorded at presentation using the Snellen’s distance chart. All patients underwent a slit-lamp bio-microscopic examination before and after pupillary mydriasis. Special emphasis was laid on recording the distribution of PEX material. Intra-Ocular Pressure (IOP) was recorded using Goldmann Applanation Tonometry (GAT). All patients underwent retinal evaluation by indirect ophthalmoscopy. Those found to have any optic disc or retinal pathology that was likely to confound post-operative visual outcome were excluded from the study. B scan ultrasonography was performed in patients in whom fundus was not visible (for e.g., mature cataracts). Other procedures included lacrimal sac syringing, manual keratometry, contact A-scan biometry with the Sanders-Retzlaff-Kraff – II (SRK – II formula). Routine systemic investigations (complete blood count, random blood sugar, renal function tests and electrocardiogram) were performed in all patients to determine fitness for surgery.
Dilatation was started one hour before surgery carried out using a combination of tropicamide 8 mg and phenylephrine 50 mg drops, with flurbiprofen 3 mg for sustaining the same. Peribulbar anaesthesia was administered in all cases. The anaesthetic solution used was a mixture of lignocaine 2% (as lignocaine hydrochloride 21.3 mg), Adrenaline (as adrenaline bitartrate 0.009 mg) with hyaluronidase (1500IU). Almost 1 ml of hyaluronidase enzyme solution was dissolved in 30 ml of Lignocaine and adrenaline solution.
Intra-operative procedures: Surgery was performed by two experienced surgeons well-versed with both PHACO and SICS. Bimanual PHACO was done via a temporal 3.2 mm limbal incision using the stop and chop technique. SICS was performed via a superior trapezoid 5.5 mm incision. The preferred mode of nucleus delivery in SICS was by Blumenthal technique. In-the-bag implantation of Posterior Chamber Intra-Ocular Lens (PCIOL) was attempted in all cases. Hydrophobic acrylic foldable one-piece IOLs were used in PHACO group and rigid Polymethyl Methacrylate (PMMA) lenses in SICS group. Patients who had to be left aphakic during primary cataract surgery underwent secondary IOL implantation at a later date. Anterior Chamber Intra-Ocular Lenses (ACIOLs) were not used in this study. Operated eyes were padded after surgery.
Post-operative management: Eye pad was removed on first post-operative day and the following parameters were recorded: Uncorrected Visual Acuity (UCVA), IOP, slit lamp biomicroscopy and indirect ophthalmoscopy (in cases where fundus was not visible preoperatively). In uncomplicated cases, patients were then discharged.
Topical antibiotic-steroid combination drops (Ciprofloxacin-dexamethasone) were prescribed in a weekly frequency of 8,6,4,3 and 2 times per day, tapered every week for a period of five weeks.
Patients were asked to follow up thrice after discharge: on Post-operative Day (POD) 7, POD 14 and POD 35. At each follow up, slit-lamp biomicroscopy, IOP measurement and indirect ophthalmoscopy were performed. Refraction was performed on POD 35 and BCVA recorded.
Statistical Analysis
Data obtained was meticulously recorded and analysed using the online Graph Pad QuickCalcs software version 2015. Statistical significance was set at 95% confidence intervals, i.e., at a p-value of <0.05. Parametric data was analysed using the chi-square test. To depict the pre-operative and post-operative visual acuities, grouped vertical bar diagrams were used.
Results
The study sample consisted of 76 males (152 eyes) and 24 females (48 eyes). The mean age of the sample was 67.95±6.77 years, with majority of patients in their seventh decade of life (n=52). PEX was clinically evident bilaterally in 83% cases. Pupillary margin was the most common site of deposition of PEX material (n=78), followed by anterior lens capsule (n=68). Mean intra-ocular pressure was 17.63±2.66 mm of Hg. As many as 63 patients had a poorly dilating pupil (diameter <5 mm after mydriasis). The mean axial length was 22.53±1.02 mm. [Table/Fig-1] outlines the demographic characteristics and ocular profiles in the study sample.
Demographic and ocular profile of the study groups.
| Parameter | Group 1 (PHACO) | Group 2 (SICS) | Total |
|---|
| Age in years (no. of patients) |
| 41-50 | 1 | 1 | 2 |
| 51-60 | 7 | 7 | 14 |
| 61-70 | 26 | 26 | 52 |
| 71-80 | 14 | 14 | 28 |
| > 80 | 2 | 2 | 4 |
| Sex |
| Males | 38 | 38 | 76 |
| Females | 12 | 12 | 24 |
| Distribution of PEX material (no. of eyes) |
| Corneal endothelium | 6 | 7 | 13 |
| Pupillary margin | 34 | 44 | 78 |
| Iris | 17 | 19 | 36 |
| Lens | 33 | 35 | 68 |
| Anterior chamber depth (van Herick grading – no. of eyes) |
| Grade 1 | 2 | 0 | 2 |
| Grade 2 | 7 | 4 | 11 |
| Grade 3 | 28 | 29 | 57 |
| Grade 4 | 12 | 18 | 30 |
| Pupillary dilatation (no. of eyes) |
| < 5mm (poor) | 5 | 8 | 13 |
| 5-7 mm (fair) | 34 | 33 | 67 |
| > 7mm (good) | 11 | 9 | 20 |
| Intra-ocular pressure (IOP) in mm Hg (no. of eyes) |
| < 14 | 4 | 6 | 10 |
| 14-21 | 46 | 44 | 90 |
Only the eyes scheduled for surgery have been included in the table
In the primary sitting, in-the-bag PCIOL implantation was possible in 96 cases. Four patients had to be left aphakic in primary sitting due to intra-operative complications. Two of these belonged to the PHACO and SICS group each. One aphakic patient was not willing for a second surgery and hence, eventually 99 cases were pseudophakic.
The intra-operative complication rates have been demonstrated in [Table/Fig-2]. As seen, the differences in the rates of intra-operative complications between the two groups were not statistically significant.
Intra-operative complication profile between PHACO and SICS groups.
| Parameter | Group 1 (PHACO) | Group 2 (SICS) | p-value* | Statistical significance |
|---|
| Difficulty/ Entension in capsulorhexis | 7 (14%) | 11 (22%) | 0.43 | none |
| Posterior capsular rupture (PCR) | 1 (2%) | 3 (6%) | 0.60 | none |
| Zonular Dialysis (ZD) | 2 (4%) | 3 (6%) | 0.64 | none |
| Nucleus drop | 1 (2%) | 0 | 0.31 | none |
| Iridodialysis | 0 | 1 (2%) | 0.31 | none |
| Overall | 13 (26%) | 21(42%) | 0.13 | none |
Figures denote the number of eyes: Bracketed figures are percentage calculated for individual groups
*Chi-square test used
Intra-operative Technique Modifications:
PHACO group: A Capsular Tension Ring (CTR) was used in 2% (n=1) case to stretch the capsular bag in intra-operative zonular dialysis. A controlled sphincterotomy was done in 2% (n=1) case to facilitate phacoemulsification through a poorly dilating pupil.
SICS group: A CTR was used in 10% (n=5) cases and a controlled sphincterotomy was done in 16% (n=8) cases. As evident from [Table/Fig-3], controlled sphincterotomy had to be done in a statistically significant higher number cases in SICS group compared to PHACO group.
Comparison of intra-operative technique modifications.
| Parameter | Group 1 (PHACO) | Group 2 (SICS) | p-value* | Statistical significance |
|---|
| Controlled sphincterotomy | 1 (2%) | 8 (16%) | p = 0.03 | statistically significant |
| Capsular Tension Ring (CTR) used | 1 (2%) | 5 (10%) | p = 0.2 | none |
Figures denote the number of eyes: Bracketed figures are percentage calculated for individual groups
*Chi-square test used
Immediate post-operative complications (as observed on first post-operative day) were also recorded and compared between the two groups. The results have been illustrated in [Table/Fig-4]. As observed, though the incidence of post-operative complications were on the higher side in SICS group in terms of numbers, there was no statistically significant difference among the two groups.
Comparison of post-operative complications on first post-operative day.
| Complication | Group 1(PHACO) | Group 2(SICS) | p-value* | Statisticalsignificance |
|---|
| Striate Keratopathy | 1 (2%) | 3 (6%) | 0.61 | none |
| Corneal oedema | 2 (4%) | 4 (8%) | 0.67 | none |
| Hyphema | 0 | 1 (2%) | 0.31 | none |
| Inflammation* | 1 (2%) | 1 (2%) | 1.0 | none |
| Increased IOP (>21mm Hg) | 1 (2%) | 1 (2%) | 1.0 | none |
| Overall | 5 (10%) | 10 (20%) | 0.26 | none |
Figures denote the number of eyes: Bracketed figures are percentage calculated for individual groups
*Chi-square test used
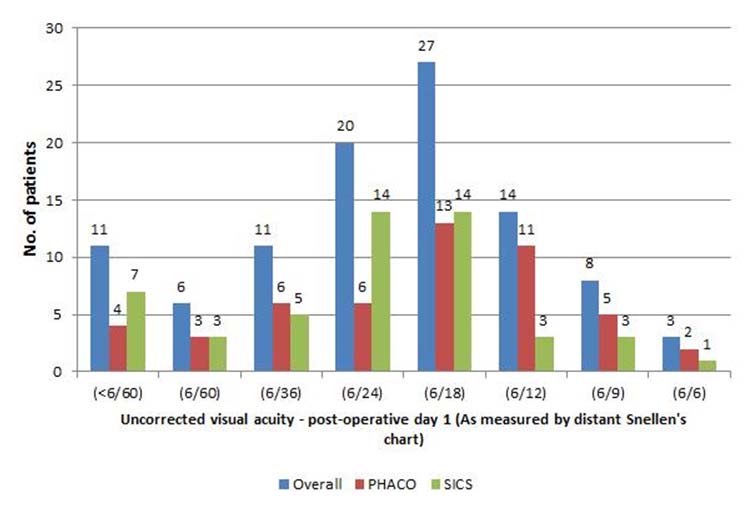
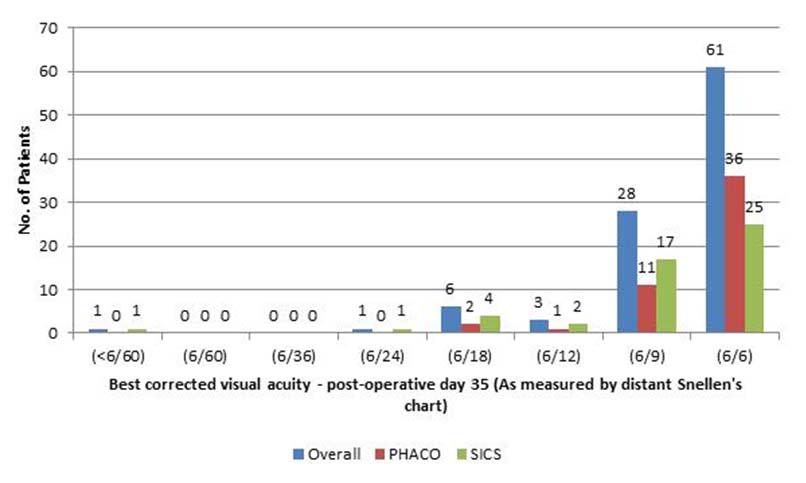
A comparison of the post-operative visual acuities on first post-operative day and at the time of third follow-up (35th post-operative day) is illustrated in [Table/Fig-5,6] respectively. As evident, 89% of the patients achieved an UCVA of 6/9 or better on 35th post-operative day.
UCVA on first post-operative day.
UCVA on 35th post-operative day.
Discussion
This study reiterated certain known facts and unearthed certain new findings during its conduct. An extensive literature search failed to find any similar study that has directly compared the visual outcome of PHACO with SICS in PEX syndrome. However, there have been numerous studies [4–16] that have compared the visual outcome of individual surgical technique, viz., Extracapsular Cataract Extraction (ECCE), SICS and PHACO in patients with and without PEX syndrome.
Intra-operative complications: Studies [4,5,11,12,14,15] have reported PCR rates ranging from 9% to 15.6% in the setting of PEX syndrome when ECCE/SICS was performed. Studies involving PHACO [11,12,14] have reported lower rates ranging from 0.3% to 7.7%. In this study, the PCR rates in both SICS (6%) and PHACO (2%) were comparable to studies [4,5,11,12,14,15] conducted worldwide. Though the incidence of PCR was lower in the PHACO group, statistically significant difference was not observed when the rates between the two techniques were compared.
Intra-operative zonular dehiscence/ dialysis/ break ranged from 4% to 15.6% [5,15] in studies evaluating ECCE/SICS and from 2.9% to 10% with phacoemulsification in PEX syndrome. In this study, the rates of zonular dehiscence were comparable to these studies and did not significantly differ between SICS (6%) and PHACO (4%) groups.
In this study, nucleus drop and iridodialysis occurred in one case (2%) of PHACO and SICS group respectively. Pranathi K et al., (with SICS and PHACO combined) reported an iridodialysis incidence of 1.9% and Jawad M et al., (with ECCE) reported an incidence of 1% [5,15]. These incidences are comparable to our study.
Two important intra-operative technique modifications were employed in this study. First, in a significantly higher number of SICS cases a controlled sphincterotomy had to be done compared to the PHACO group, which has not been previously reported. However, this apparently significant difference in the rates of sphincterotomy may be because of the basic difference in the process of nucleus management in PHACO and SICS. In PHACO, an in-the-bag nucleus division and aspiration was attempted, with only one case requiring a supracapsular management due to a rigid pupil. Hence, a sphincterotomy was done in this sole case only. However, in SICS, as the nucleus has to be luxated out in all cases, the problem of small and rigid pupil has to be dealt with in higher instances.
Post-operative complications: Striate Keratopathy was the most common post-operative complication encountered in this study. Sufi AR et al., with PHACO, had a 22% incidence in their study [14]. In this study the incidence of SK in PHACO group was lower than SICS group but the difference was not statistically significant.
The incidence of corneal oedema was higher in the SICS group compared to PHACO group, but this difference was not statistically significant. Mohan P et al., found a significantly higher rate of post-operative corneal oedema in SICS group compared to PHACO group [16]. Other studies have reported varying rates [4,11]. Minimal damage to the corneal endothelium is of utmost importance during cataract surgery. Various factors that govern this are the operative time, endothelial handling during manipulation of instruments in the anterior chamber, grade of cataract, etc. Minimal operative time and generous use of ocular viscoelastic devices is helpful to minimize endothelial damage and hence prevent corneal oedema.
The rates of post-operative hyphema have been reported from 1% to 9.4% in ECCE/SICS-based studies [4,5,15], while Sufi AR et al., had a 0% incidence with PHACO [14]. In current study, hyphema was observed in just one case in the SICS group, which resolved with non-surgical intervention.
Post-operative inflammation can manifest as aqueous cells/flare, iritis or a pupillary membrane. Sufi AR et al., noted a significantly higher incidence of post-operative inflammation in PEX group (42%) compared to control group (4%) [14]. On the contrary, Shingleton BJ et al., reported no statistically significant difference in the two groups (1.4% in non-PEX group compared to 1.7% in the PEX group) [11]. In this study, inflammation was seen in 2% cases, one in SICS and other in PHACO group. A variety of factors are responsible for post-operative inflammation. Interplay of these factors might be the reason for variance in the reported incidence in different studies.
Reported rates of IOL decentration vary from 3.1% to 5.8% in ECCE/SICS-based studies [4,5,15] and 0.3% reported by Shingleton BJ et al., with PHACO [11]. This study had comparable incidence rates to the above studies. The difference in the PHACO and SICS group was statistically non-significant.
Post-operative visual acuity: On the immediate post-operative day, the uncorrected visual acuities varied widely from less than 6/60 to 6/6. By the time of third follow up, 89% patients had a BCVA of 6/9 or better. Sufi AR et al., noted a visual acuity of equal to or better than 6/9 in 72% of their PEX group patients [14]. Pranathi K et al., [5] reported a visual acuity between 6/12 – 6/6 in 23.1% of their patients. Some studies (e.g., Shingleton et al., [11]) have used logmar charts for acuity recording and have observed slightly better acuity in non-PEX group, but this was not statistically significant. Standardization of recording the visual acuity is needed to compare the results between different studies.
Limitation
This study had certain limitations which can serve as avenues for future research. Most significantly, the study lacked a control group without PEX syndrome that could have led to comparison of visual outcome of both SICS and PHACO with normal population. The sample size was conveniently derived and was too small to extrapolate the study findings to the general population. There was no long term follow up in either group. Post operative complications and visual acuity were evaluated only till a maximum period of five weeks. Most other studies have followed up for upto six months or so. Long-term follow-up could reveal late complications as well as any change in the course of visual outcome. Owing to small sample size which lowers the statistical power, the reliability of the findings can be questioned. However, this being a pilot study can serve as a frame work for randomized major studies in future.
Conclusion
Deposition of PEX material onto ocular structures leads to changes that can pose challenges and cause complications during cataract surgery. Poor pupillary dilatation forms the basis for majority of difficulties in cataract surgery, right from limitation in size of capsulorhexis to nucleus delivery/phacoemulsification. Inherent zonular weakness can lead to dialysis intraoperatively, which predisposes to variety of complications such as posterior capsular rent, subluxation, etc. In our study, we did encounter numerous intraoperative complications, both during SICS and PHACO. However, the rate of complications did not significantly differ between the two categories. This held true for both intra and post operative complications. This proves that apparently both small incision cataract surgery and PHACO are apparently safe operative procedures in PEX syndrome. Use of capsule stretching devices, pupil stretching devices, controlled sphincterotomy, etc., need to be contemplated and tailored according to merit of each individual case. Surgeon expertise is also a factor. However, considering the limitations of this pilot study, further research needs to be done to reveal any new insights into eventual visual outcome.
Only the eyes scheduled for surgery have been included in the table
Figures denote the number of eyes: Bracketed figures are percentage calculated for individual groups
*Chi-square test used