Introduction
Periodontitis is a major cause of tooth loss and has been suggested as a risk factor for several systemic conditions [1]. Periodontitis is classified into several types of which the aggressive and chronic forms are the two main types. Although both forms have similar pathophysiology, aggressive periodontitis is more destructive in nature with higher progression rate, distinctive clinical characteristics and its aetiology may be different [2]. The rate of destruction in aggressive periodontitis was estimated to be 3-4 times more than the chronic form. Aggressive periodontitis tends to have a familial aggregation and comprised of what was previously known as rapidly progressive and juvenile periodontitis [3].
Aggressive periodontitis patients are likely to loose multiple teeth due to the progression and destructive nature of the disease, which may impact future dental implant rehabilitation. Even though dental implant is not contraindicated in patients affected with aggressive periodontitis, a greater bone loss rate has been reported [4,5]. It is possible that bone density is different in aggressive periodontitis patients. This assumption was based on the reported data that showed an association between periodontitis and osteoporosis where reduced bone density in osteoporotic patients was suggested to create vulnerable sites at which the effect of periodontal pathogens and host immune response is enhanced resulting in rapid progression of periodontal tissue destruction [6]. Furthermore, a recent systematic review showed that osteoporotic subjects had lower dental implant survival rate [7], which could suggest that the quality of recipient bone site might be an important factor.
Studies on early detection of aggressive periodontitis cases would be invaluable in order to provide proper treatment and subsequently prevent the substantial periodontal tissues breakdown associated with delayed discovery. Although much of the information required to diagnose periodontitis can be obtained through clinical examination alone, the information on bone levels and density provided by radiographs has a significant impact on risk assessment, diagnosis as well as treatment outcomes. However, bone density and the precise form of periodontal defects including furcation involvements, hemiseptum and intrabony defects cannot be determined easily from conventional two-dimensional radiographs [8,9]. CBCT could be utilized to overcome these limitations. CBCT can be used to assess the mineral density of craniofacial bone structures and has been utilized to predict osteoporosis [10–14]. CBCT has also been used to assess bone density for dental implant treatment planning and placement [15–17]. Isoda K et al., showed that the quality of evaluated bone using CBCT had a significant correlation with the primary implants stability suggesting that CBCT estimated bone density might predict implant stability [16]. Similarly, Tatli U et al., reported the possibility to use preoperative CBCT to predict the stability of immediately loaded implants [17]. Hasan I et al., reported that CBCT gray values can be used to monitor bone density changes at different periods after insertion of dental implants [15]. However, utilization of gray scale to assess bone density is criticized by some researchers when used as an absolute value [18,19]. Thus, the scanning device and image-acquisition settings and positioning influence the intensity values of CBCT images and should be controlled for in order to reduce CBCT-related variability in mineral density [20].
Understanding the changes in bone density of periodontitis patients might be useful in its early detection and proper treatment planning. Although estimation of bone density could be useful in the prediction of aggressive periodontitis patients, thus far, CBCT has not been previously utilized to address this issue. Therefore, the purpose of this study was to measure alveolar bone density in aggressive periodontitis patients and compare it with periodontally healthy individuals using CBCT.
Materials and Methods
This cross-sectional study was carried out at the Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia and included 40 individuals using purposive sampling, between the ages of 18 to 40 years. Twenty patients with a confirmed diagnosis of aggressive periodontitis (both localized and generalized) and 20 periodontally healthy patients attending the dental clinics for implant placement or extraction of impacted third molars and required CBCT for their procedure were included in the study. The diagnosis of aggressive periodontitis was made in the postgraduate periodontic clinics based on the case history, clinical and radiographic findings as outlined in 1999 International Workshop for the Classification of Periodontal Diseases and Conditions [21]. The research was conducted in accordance with the principles of the Helsinki Declaration and was approved by the Research Ethics Committee of the Faculty of Dentistry at King Abdulaziz University. An informed consent was obtained from participants prior to their enrollment.
The exclusion criteria included; patients who received medications such as steroids, non-steroidal anti-inflammatory drugs, bisphosphonates or any similar drug that might affect bone density, within the previous six months. Also, patients who received any periodontal treatment in the previous 12 months, patients with known systemic disease according to the Cornell Medical Index [22,23], pregnant females, smokers, osteoporotic patients and patients with any form of periodontitis other than aggressive were excluded.
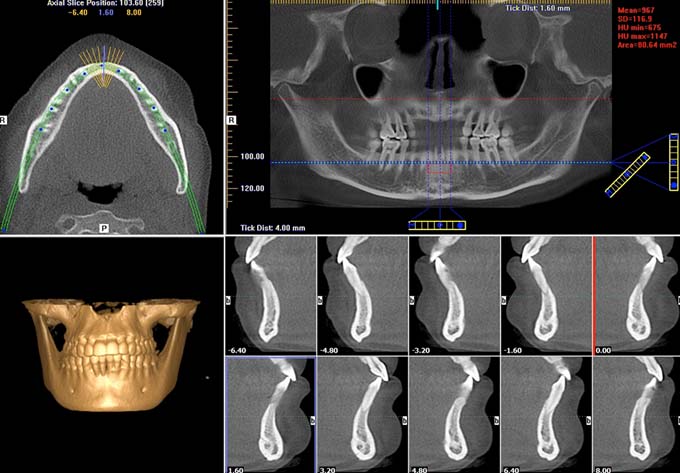
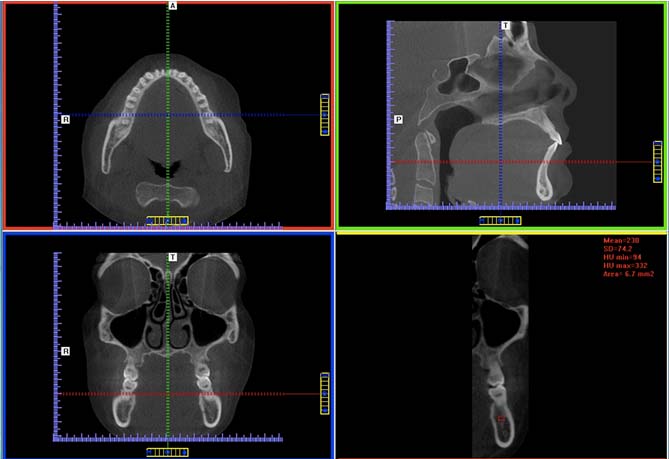
Patients were scanned using i-CAT Next Generation CBCT unit (Imaging Sciences International, LLC, Hatfield, PA, USA). All the selected images were acquired with the same machine and scan settings. Scans were taken with 0.4 mm voxel resolution, 16 cm field of view diameter and 13 cm field of view height with 8.9 seconds scan time. Scans were processed and interpreted using i-CAT vision software. A calibrated Oral and Maxillofacial Radiologist interpreted all images. By using the software density measurement tool (gray scale value), alveolar bone density was recorded on selected locations and slices. The measurements of the anterior area of the mandible were taken apical to the anterior teeth on the reconstructed panoramic view. The slice thickness for the reconstructed panoramic view was adjusted to 3 mm for all images. This was undertaken to limit bone density measurement to the trabecular bone. The measured area size was adjusted to be equal in all cases and it was 80.6 mm2 as shown in [Table/Fig-1]. In the posterior area of the mandible, measurements were performed on the multi planar view at the apical area between mandibular first and second molars bilaterally. Cross-sectional slice on each side was generated perpendicular to mandibular buccal surface. Slice thickness and measured area size were standardized in all cases [Table/Fig-2].
The measurements of the anterior area of the mandible were taken | apical to the anterior teeth on the reconstructed panoramic view and the slice I thickness for the reconstructed panoramic view was adjusted to 3 mm and adjusting I the measured area size to be equal to 80.6 mm2.
The measurements at the apical area between mandibular first and second molars were performed on the multi planar view and a cross sectional slice was generated perpendicular to mandibular buccal surface.
Statistical Analysis
Data analysis was carried out using the Statistical Package for Social Science (SPSS for Windows, version 20, IBM Corp, Armonk, NY, USA). The data are presented as mean±Standard Deviation (SD). Normality was tested using the Kolmogorov–Smirnov, and thus parametric tests were performed. Independent sample t-tests were used to compare aggressive periodontitis with controls for age and bone density of the anterior and posterior regions. Multivariable linear regression models were also performed and statistical significance was set at p<0.05.
Results
A total of 40 individuals were included in this study, 20 diagnosed with aggressive periodontitis and 20 periodontally healthy controls. The total sample consisted of 24 females and 16 males with no difference in gender distribution between groups, p = 0.55.
The results of the bivariate analysis are shown in [Table/Fig-3]. The mean age of the total study sample was 30.1 (±6.1) years with no significant difference between groups, mean age of aggressive periodontitis was 32 (±4.6) years and 29.4 (±6.5) years for the control group, p= 0.43. The mean bone density for the total sample in the anterior region was 882.4 (±238.2) and 259.1 (±96.1) in the posterior region. In aggressive periodontitis, the mean bone density in the anterior region was 822.1 (±225.7) and was 955.5 (±240.2) for the control group with no statistically significant difference, p = 0.12. In the posterior region the mean bone density for the aggressive periodontitis and the control groups were 284.2 (±92.5) and 230.7 (±95.2), respectively with no significant difference between them, p = 0.12.
Descriptive and bivariate statistics of the study sample.
| Total sample | Aggressive Periodontitis Means (±Standard Deviation) | Control Means (±Standard Deviation) | p-value |
|---|
| Age | 30.1 (6.1) | 32 (4.6) | 29.4 (6.5) | 0.43 |
| Bone density: |
| Anterior region | 882.4 (238.2) | 822.1 (225.7) | 955.5 (240.2) | 0.12 |
| Posterior region | 259.1 (96.1) | 284.2 (92.5) | 230.7 (95.2) | 0.12 |
The results of the multivariable regression models are shown in [Table/Fig-4,5]. In the anterior region, no significant association was found between bone density and groups. However, patient’s age was significantly associated with bone density. A one-year increase in age was found to be associated with 21.5 unit increase in bone density independent of gender and group. In the posterior region, bone density was not associated with study groups, age or gender.
The multivariable linear regression model of the anterior bone density.
| Model | Unstandardized Coefficients | Standardized Coefficients | t | p-value |
|---|
| B | Std. Error | Beta |
|---|
| Age | 21.5 | 7.6 | 0.63 | 2.81 | 0.01 |
| Gender | 53.3 | 99.6 | 0.12 | 0.54 | 0.60 |
| Group | -105.3 | 100.5 | -0.23 | -1.05 | 0.31 |
The multivariable linear regression model of the posterior bone I density.
| Model | Unstandardized Coefficients | Standardized Coefficients | t | p-value |
|---|
| B | Std. Error | Beta |
|---|
| Age | 6.4 | 3.9 | 0.38 | 1.60 | 0.13 |
| Gender | -24.4 | 52.3 | -0.11 | -0.47 | 0.65 |
| Group | 49.7 | 52.7 | 0.22 | 0.94 | 0.36 |
Discussion
This study used the CBCT to measure the alveolar bone density in aggressive periodontitis patients and healthy controls. The results of the present study showed no difference between the two groups. It was not possible to compare the results of this study to others as no previous studies have examined alveolar bone density in patients affected with aggressive periodontitis. Numerous studies on chronic periodontitis are available in relation to osteoporosis or low bone mineral density; but their results were inconclusive. Some investigators showed that the prevalence of chronic periodontitis is higher in osteoporotic subjects [24–26]. In a recent study, treatment of osteoporosis by bisphosphonate therapy as an adjunct to nonsurgical periodontal treatment resulted in significant improvement in periodontal condition [27]. Also, a recent systematic review found a positive relationship between osteoporosis and periodontal disease [28]. In contrast, others found no association between periodontitis and osteoporosis or low bone mineral density [29–31].
CBCT is an excellent tool for viewing anatomy in three dimensions. Its application in clinical dental practice provides a number of merits when compared to conventional CT and it has become commonly used for oral and maxillofacial imaging, providing great threedimensional resolution, gray density range and contrast, and good pixel/noise ratio [32].
Several investigators demonstrated a significant correlation between CBCT and CT when measuring bone density [33–35]. Still, the use of gray scale value of CBCT to assess bone density was not recommended by some investigators when used as an absolute value [18,19]. A study showed that CBCT was not beneficial when CBCT values are taken as absolute values for the assessment of bone density of jaws and established that although CBCT has a low radiation dose, however it does not provide precise estimation of bone density [18]. This was attributed to the fact that CBCT lacks the ability to provide Hounsfield Unit (HU) measurements [36–38]. However, several investigators have argued that CBCT grayscale values could be similar to HU [33,39–45]. Valiyaparambil JV et al., evaluated the correlation between dental CBCT gray scale values and HU and whether CBCT gray values correlate with clinical bone quality assessed subjectively during dental implant placement [34]. Their results showed that the dimensional accuracy of CBCT was comparable with CT although the gray density values of the CBCT images (voxel value) were not absolute.
In the present study voxel values of standardized CBCT images were compared between the aggressive periodontitis group and their control, which eliminated the need for having absolute values [34]. Moreover, Campos MJ et al., in a study to assess the degree of mineral density of the apical third of the roots of maxillary central incisors and of the periapical bone [46], through CBCT images, comparing orthodontically treated and untreated subjects, they stated that mineral density determination is the best indicator for the quality of mineralized tissues, and CBCT has been proposed as a low radiation dose method for achieving such a purpose.
Periodontitis is a multifactorial disease that develops as an interaction between bacteria and the host response. The genetic predisposition in cases of aggressive periodontitis in particular is recognized as an important factor. Even though the prevalence of aggressive periodontitis is low, the destructive nature of this disease makes its early detection and proper understanding of the soft and hard tissue conditions essential, for planning comprehensive treatment [3]. The successful treatment of aggressive periodontitis relies on early diagnosis and treatment targeted against the causative microorganisms to provide optimum environment, free of infection to aid healing. The detection of aggressive periodontitis is complex and involves a great amount of skill. A corner stone of periodontal examination is periodontal probing of six sites per tooth, which is laborious and time consuming. This is the classical screening and monitoring method that has to be repeated periodically and thus far, no alternative screening tools with proven utility are available [47].
Conventional radiographs are valuable adjunct to clinical examination as it provides essential information regarding the extent and pattern of alveolar bone status. The use of these radiographs greatly aids the diagnosis of periodontal disease, as they can be useful in assessing the effect of treatment as well as disease progress and prognosis. However, conventional radiographs have major limitations such as they provide two-dimensional views of three-dimensional structures and underestimate alveolar bone destruction [9]. These limitations can be overcome by CBCT which provide greater information, but thus far CBCT is not considered a routine imaging modality. The CBCT radiation dose is equivalent to conventional full mouth series and about 3 to 7 times panoramic radiograph dose [9,48,49].
Limitation
One limitation to the current study was its small sample size due to the stringent inclusion criteria; thus, studies with larger sample size are recommended. Furthermore, future studies to compare the assessment of bone density using CBCT, CT-Scanning and Dual-Energy X-Ray Absorptiometry (DXA) in aggressive and other forms of periodontitis are suggested.
Conclusion
Within the limitations of the study, the results showed no difference in alveolar bone density between aggressive periodontitis patients and periodontally healthy controls.
[1]. Kim J, Amar S, Periodontal disease and systemic conditions: A bidirectional relationshipOdontology 2006 94:10-21. [Google Scholar]
[2]. Albandar JM, Aggressive and acute periodontal diseasesPeriodontol 2000 2014 65:7-12. [Google Scholar]
[3]. Armitage GC, Cullinan MP, Comparison of the clinical features of chronic and aggressive periodontitisPeriodontol 2000 2010 53:12-27. [Google Scholar]
[4]. Al-Zahrani MS, Implant therapy in aggressive periodontitis patients: A systematic review and clinical implicationsQuintessence Int 2008 39:211-15. [Google Scholar]
[5]. Kim KK, Sung HM, Outcomes of dental implant treatment in patients with generalized aggressive periodontitis: A systematic reviewJ Adv Prosthodont 2012 4:210-17. [Google Scholar]
[6]. Reddy MS, Morgan SL, Decreased bone mineral density and periodontal managementPeriodontol 2000 2013 61:195-218. [Google Scholar]
[7]. Giro G, Chambrone L, Goldstein A, Rodrigues JA, Zenobio E, Feres M, Impact of osteoporosis in dental implants: A systematic reviewWorld J Orthop 2015 6:311-15. [Google Scholar]
[8]. Park CH, Abramson ZR, Taba M, JrJin Q, Chang J, Kreider JM, Threedimensional micro-computed tomographic imaging of alveolar bone in experimental bone loss or repairJ Periodontol 2007 78:273-81. [Google Scholar]
[9]. de Faria Vasconcelos K, Evangelista KM, Rodrigues CD, Estrela C, de Sousa TO, Silva MA, Detection of periodontal bone loss using cone beam CT and intraoral radiographyDentomaxillofac Radiol 2012 41:64-69. [Google Scholar]
[10]. Benavides E, Rios HF, Ganz SD, An CH, Resnik R, Reardon GT, Use of cone beam computed tomography in implant dentistry: The International Congress of Oral Implantologists consensus reportImplant Dent 2012 21:78-86. [Google Scholar]
[11]. Abbassy MA, Sabban HM, Hassan AH, Zawawi KH, Evaluation of mini-implant sites in the posterior maxilla using traditional radiographs and cone-beam computed tomographySaudi Med J 2015 36:1336-41. [Google Scholar]
[12]. Kapila SD, Nervina JM, CBCT in orthodontics: Assessment of treatment outcomes and indications for its useDentomaxillofac Radiol 2015 44:20140282 [Google Scholar]
[13]. Barngkgei I, Joury E, Jawad A, An innovative approach in osteoporosis opportunistic screening by the dental practitioner: The use of cervical vertebrae and cone beam computed tomography with its viewer programOral Surg Oral Med Oral Pathol Oral Radiol 2015 120:651-59. [Google Scholar]
[14]. Barngkgei I, Al Haffar I, Khattab R, Osteoporosis prediction from the mandible using cone-beam computed tomographyImaging Sci Dent 2014 44:263-71. [Google Scholar]
[15]. Hasan I, Dominiak M, Blaszczyszyn A, Bourauel C, Gedrange T, Heinemann F, Radiographic evaluation of bone density around immediately loaded implantsAnn Anat 2015 199:52-57. [Google Scholar]
[16]. Isoda K, Ayukawa Y, Tsukiyama Y, Sogo M, Matsushita Y, Koyano K, Relationship between the bone density estimated by cone-beam computed tomography and the primary stability of dental implantsClin Oral Implants Res 2012 23:832-36. [Google Scholar]
[17]. Tatli U, Salimov F, Kurkcu M, Akoglan M, Kurtoglu C, Does cone beam computed tomography-derived bone density give predictable data about stability changes of immediately loaded implants?: A 1-year resonance frequency follow-up studyJ Craniofac Surg 2014 25:e293-99. [Google Scholar]
[18]. Cassetta M, Stefanelli LV, Pacifici A, Pacifici L, Barbato E, How accurate is CBCT in measuring bone density? A comparative CBCT-CT in vitro studyClin Implant Dent Relat Res 2014 16:471-78. [Google Scholar]
[19]. Pauwels R, Jacobs R, Singer SR, Mupparapu M, CBCT-based bone quality assessment: Are Hounsfield units applicable?Dentomaxillofac Radiol 2015 44:20140238 [Google Scholar]
[20]. Hsu JT, Chang HW, Huang HL, Yu JH, Li YF, Tu MG, Bone density changes around teeth during orthodontic treatmentClin Oral Investig 2011 15:511-19. [Google Scholar]
[21]. Armitage GC, Development of a classification system for periodontal diseases and conditionsAnn Periodontol 1999 4:1-6. [Google Scholar]
[22]. Abramson JH, The cornell medical index as an epidemiological toolAm J Public Health Nations Health 1966 56:287-98. [Google Scholar]
[23]. Ng N, Kaye EK, Garcia RI, Coffee consumption and periodontal disease in malesJ Periodontol 2014 85:1042-49. [Google Scholar]
[24]. Lohana M, Suragimath G, Abbayya K, Varma S, Zope S, Kale V, A study to assess and correlate osteoporosis and periodontitis in selected population of MaharashtraJ Clin Diagn Res 2015 9:ZC46-50. [Google Scholar]
[25]. Chang WP, Chang WC, Wu MS, Pai JT, Guo YC, Chen KC, Population-based 5-year follow up study in Taiwan of osteoporosis and risk of periodontitisJ Periodontol 2014 85:e24-30. [Google Scholar]
[26]. Passos JS, Vianna MI, Gomes-Filho IS, Cruz SS, Barreto ML, Adan L, Osteoporosis/osteopenia as an independent factor associated with periodontitis in postmenopausal women: A case-control studyOsteoporos Int 2013 24:1275-83. [Google Scholar]
[27]. Bhavsar NV, Trivedi SR, Dulani K, Brahmbhatt N, Shah S, Chaudhri D, Clinical and radiographic evaluation of effect of risedronate 5 mg as an adjunct to treatment of chronic periodontitis in postmenopausal women (12-month study)Osteoporos Int 2016 27:2611-19. [Google Scholar]
[28]. Dodd DZ, Rowe DJ, The relationship between postmenopausal osteoporosis and periodontal diseaseJ Dent Hyg 2013 87:336-44. [Google Scholar]
[29]. Hernandez-Vigueras S, Martinez-Garriga B, Sanchez MC, Sanz M, Estrugo-Devesa A, Vinuesa T, Oral microbiota, periodontal status, and osteoporosis in postmenopausal femalesJ Periodontol 2016 87:124-33. [Google Scholar]
[30]. Alves RC, Felix SA, Rodriguez-Archilla A, Oliveira P, Brito J, Dos Santos JM, Relationship between menopause and periodontal disease: A cross-sectional study in a Portuguese populationInt J Clin Exp Med 2015 8:11412-19. [Google Scholar]
[31]. Moeintaghavi A, Pourjavad M, Dadgar S, Tabbakh NS, Evaluation of the association between periodontal parameters, osteoporosis and osteopenia in post menopausal womenJ Dent (Tehran) 2013 10:443-48. [Google Scholar]
[32]. Kamburoglu K, Use of dentomaxillofacial cone beam computed tomography in dentistryWorld J Radiol 2015 7:128-30. [Google Scholar]
[33]. Parsa A, Ibrahim N, Hassan B, van der Stelt P, Wismeijer D, Bone quality evaluation at dental implant site using multislice CT, micro-CT, and cone beam CTClin Oral Implants Res 2015 26:e1-7. [Google Scholar]
[34]. Valiyaparambil JV, Yamany I, Ortiz D, Shafer DM, Pendrys D, Freilich M, Bone quality evaluation: Comparison of cone beam computed tomography and subjective surgical assessmentInt J Oral Maxillofac Implants 2012 27:1271-77. [Google Scholar]
[35]. Gonzalez-Garcia R, Monje F, The reliability of cone-beam computed tomography to assess bone density at dental implant recipient sites: A histomorphometric analysis by micro-CTClin Oral Implants Res 2013 24:871-79. [Google Scholar]
[36]. Swennen GR, Schutyser F, Three-dimensional cephalometry: Spiral multislice vs cone-beam computed tomographyAm J Orthod Dentofacial Orthop 2006 130:410-16. [Google Scholar]
[37]. Katsumata A, Hirukawa A, Noujeim M, Okumura S, Naitoh M, Fujishita M, Image artifact in dental cone-beam CTOral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 101:652-57. [Google Scholar]
[38]. Katsumata A, Hirukawa A, Okumura S, Naitoh M, Fujishita M, Ariji E, Effects of image artifacts on gray-value density in limited-volume cone-beam computerized tomographyOral Surg Oral Med Oral Pathol Oral Radiol Endod 2007 104:829-36. [Google Scholar]
[39]. Cha JY, Kil JK, Yoon TM, Hwang CJ, Miniscrew stability evaluated with computerized tomography scanningAm J Orthod Dentofacial Orthop 2010 137:73-79. [Google Scholar]
[40]. Mah P, Reeves TE, McDavid WD, Deriving Hounsfield units using grey levels in cone beam computed tomographyDentomaxillofac Radiol 2010 39:323-35. [Google Scholar]
[41]. Naitoh M, Aimiya H, Hirukawa A, Ariji E, Morphometric analysis of mandibular trabecular bone using cone beam computed tomography: An in vitro studyInt J Oral Maxillofac Implants 2010 25:1093-98. [Google Scholar]
[42]. Naitoh M, Hirukawa A, Katsumata A, Ariji E, Evaluation of voxel values in mandibular cancellous bone: Relationship between cone-beam computed tomography and multislice helical computed tomographyClin Oral Implants Res 2009 20:503-06. [Google Scholar]
[43]. Parsa A, Ibrahim N, Hassan B, Motroni A, van der Stelt P, Wismeijer D, Reliability of voxel gray values in cone beam computed tomography for preoperative implant planning assessmentInt J Oral Maxillofac Implants 2012 27:1438-42. [Google Scholar]
[44]. Pittman JW, Navalgund A, Byun SH, Huang H, Kim AH, Kim DG, Primary migration of a mini-implant under a functional orthodontic loadingClin Oral Investig 2014 18:721-28. [Google Scholar]
[45]. Reeves TE, Mah P, McDavid WD, Deriving Hounsfield units using grey levels in cone beam CT: A clinical applicationDentomaxillofac Radiol 2012 41:500-08. [Google Scholar]
[46]. Campos MJ, de Albuquerque EG, Pinto BC, Hungaro HM, Gravina MA, Fraga MR, The role of orthodontic tooth movement in bone and root mineral density: A study of patients submitted and not submitted to orthodontic treatmentMed Sci Monit 2012 18:CR752-57. [Google Scholar]
[47]. Preshaw PM, Detection and diagnosis of periodontal conditions amenable to preventionBMC Oral Health 2015 15(Suppl 1):S5 [Google Scholar]
[48]. Feijo CV, Lucena JG, Kurita LM, Pereira SL, Evaluation of cone beam computed tomography in the detection of horizontal periodontal bone defects: An in vivo studyInt J Periodontics Restorative Dent 2012 32:e162-68. [Google Scholar]
[49]. Signorelli L, Patcas R, Peltomaki T, Schatzle M, Radiation dose of cone-beam computed tomography compared to conventional radiographs in orthodonticsJ Orofac Orthop 2016 77:9-15. [Google Scholar]