Dangerous Headache: A Case of Dural Venous Sinus Thrombosis with Protein S Deficiency
M Hari Kumar1, D Angeline Deepthi2, Deepak Ningombam Singh3, Banu Virupakshappa4, R Rahul5
1 Senior Lecturer, Department of Oral Medicine and Radiology, Saveetha Dental College & Hospital, Saveetha University, Chennai, Tamil Nadu, India.
2 Reader, Department of Oral Medicine and Radiology, Rajas Dental College, Tirunelvelli, Tamil Nadu, India.
3 Assistant Professor, Department of Oral Medicine and Radiology, Dental College, Regional Institute of Medical Sciences, Manipur University, Imphal, Manipur, India.
4 Reader, Department of Oral Medicine and Radiology, Educare Institute of Dental Science, Malappuram, Kerala, India.
5 Senior Lecturer, Department of Oral Medicine and Radiology, Azeezia College of Dental Sciences and Research, Kollam, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. M Hari Kumar, Senior Lecturer, Department of Oral Medicine and Radiology, Saveetha Dental College & Hospital, Saveetha University, 162, Masilamani Nagar, Seneerkuppam Bypass Road, Poonamallee-600077, Chennai, Tamil Nadu, India.
E-mail: drhari.omrd@gmail.com
Dural Venous Sinus Thrombosis (DVST) is a sporadic cause of headache. DVST is a recherché complication of maxillary sinus infection. Maxillary sinusitis infection may spread directly to orbit via lamina papyracea and it is expedited by the presence veins of breschet. The authors present a clinical case of dural sinus thrombosis with protein S deficiency and also describe an effective management approach for DVST.
Arteriovenous, Magnetic resonance venography, Visual analogue scale
Case Report
A 23-year-old male presented to dental clinic with three months history of bifrontal pulsatile headache which was associated with nasal congestion, right facial numbness. Subsequently, he complained of photophobia and pulsatile tinnitus in both the ears for past two weeks. The pain intensity was 4 on the Visual Analogue Scale (VAS) lasting five hours and gradually progressed over the next five days to a score of 6 on VAS.
There was no previous history of trauma and no family history of headache, migraines. There was no prior history of thrombosis and thrombophilic predisposition. His past medical history was remarkable for maxillary sinusitis for which he had been on self medication acetaminophen 650 mg (Dolo 650) three times a day as required for past one month. On physical examination he was conscious, oriented, and haemodynamically stable with normal visual acuity but grade III papilloedema on fundus examination. Rests of the cranial examinations were normal and there was no motor or sensory deficit or incoordination. Signs of meningeal irritation were present with positive kernig’s sign.
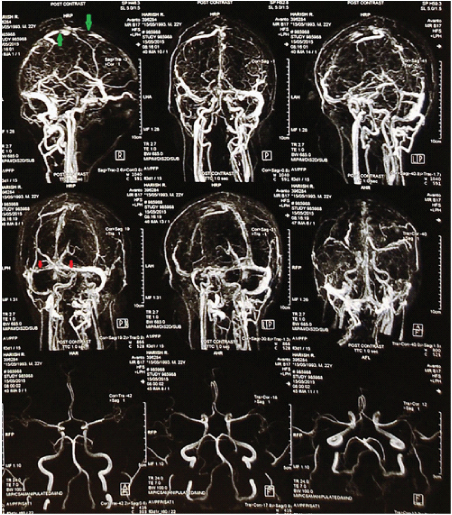
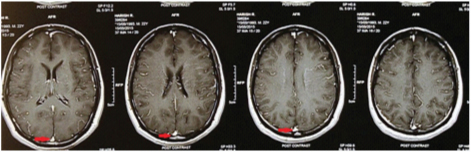
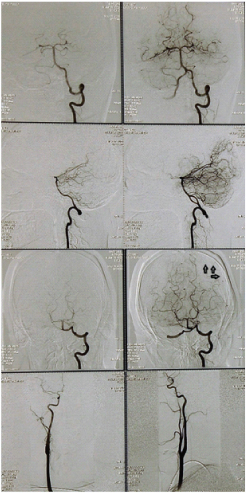
Preliminary laboratory investigations including a complete haemogram, routine urine test were normal. The Cerebrospinal Fluid (CSF) culture for bacteria (including mycobacteria) and fungi were negative. An emergency Computerized Tomography (CT) scan of brain and paranasal sinus without contrast was carried and it showed mucosal thickening with small retention cyst in the right maxillary sinus – highly suggestive of right maxillary sinusitis [Table/Fig-1]. Magnetic Resonance Imaging (MRI) with Magnetic Resonance Venography (MRV) brain revealed features of dural venous thrombosis involving superior sagittal sinus, straight sinus and bilateral transverse sinus without any evidence of haemorrhagic venous infarct [Table/Fig-2]. MRI with contrast revealed ill defined hyper attenuation of super sagittal sinus associated with hyperdense foci. [Table/Fig-3]. Digital subtraction angiography revealed no evidence of Arteriovenous (AV) fistula, Arteriovenous Malformation (AVM) or aneurysm of intracranial vessels. Non opacification of left transverse sinus, medial part of right transverse sinus, straight sinus and most of superior saggital sinus suggestive of thrombosis [Table/Fig-4]. Prothrombotic work up done prior to starting anticoagulant revealed protein S deficiency. His visual acuity and visual field charting was normal.
Emergency CT scan of brain and paranasal sinus without contrast showing mucosal thickening with small retention cyst in the right maxillary sinus. The white arrows indicate mucosal thickening with small retention cyst in the right maxillary sinus.

Magnetic resonance imaging (MRI) with Magnetic resonance venography (MRV) brain revealed features of dural venous sinus thrombosis involving superior sagittal sinus, straight sinus and bilateral transverse sinus without any evidence of haemorrhagic venous infarct. The green arrows indicate narrowing of superior sagittal sinus and red arrows indicate narrowing of bilateral transverse sinus suggestive of venous sinus thrombosis.
MRI with contrast revealed ill defined hyper attenuation of super sagittal sinus associated with hyperdense foci. The red arrows indicate delta sign in superior sagittal sinus.
Digital subtraction angiography revealed no evidence of AV fistula, AVM or aneurysm of intracranial vessels. Non opacification of left transverse sinus, medial part of right transverse sinus, straight sinus and most of superior sagittal sinus. The black arrows indicate non opacified superior sagittal sinus suggestive of extensive thrombosed superior sagittal sinus.
The patient was referred to private stroke clinic and he was treated with anticoagulant 4 mg Warf (warfarin) tablet twice daily for 10 days. Since the patient developed severe headache, he was started with Diamox (acetazolamide) 250 thrice daily with Dolo (paracetamol) 650 twice daily for ten days. His headache subsided with complete bed rest and good rehydration. The patient was advised to continue anticoagulant 5 mg Warf (warfarin) tablet once daily for six months.
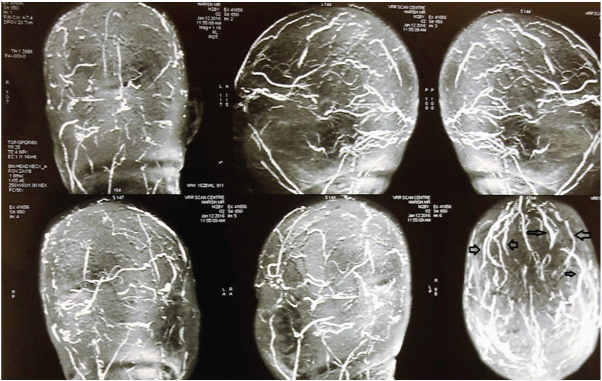
After the six month follow up, there was no signs of meningeal irritation and papilloedema. The follow up MRI with MRV was normal [Table/Fig-5]. The warfarin was stopped and he was advised to have regular recall visit to stroke clinic, for every three months.
At six month follow up, MRI with MRV showing complete recanalization of the previously thrombosed sinuses. The black arrows indicate recanalization of the previously thrombosed sinuses.
Discussion
DVST is a sporadic disease with an unreliable prognosis. Diverse aetiologies play major role in the development of dural sinus thrombosis like infections from paranasal sinusitis, intracranial abscess, otitis, mastoiditis and meningitis have also been reported [1].
The trabeculated cavernous sinus acts as sieves, filtering bacteria, thrombi from the maxillary sinus, medial third of face and teeth. Due to lack of one-way valves infected thrombi or blood clot from deep facial vein or inferior ophthalmic vein communicate to cavernous sinus via pterygoid plexus [2].
Clinical presentations are various in DVST and headache is the most common presenting symptom. Sensory deficits, dysphagia, seizures occurs in 75% of cases. MRI combined with MRV remains gold standard imaging technique in diagnosing DVST [3].
The accurate prevalence of protein S deficiency is unknown. Approximately protein S deficiency is present in 0.2% of general population. Hereditary protein S deficiency is caused by PROS1 gene mutation [4].
Protein S is a vitamin K-dependent cofactor and it is produced by endothelial cells, megakaryocytes, osteoblasts and hepatocytes. Acquired protein S deficiency is associated with liver disease, pregnancy, HIV infection, systemic lupus erythematous, disseminated intravascular coagulation, warfarin and oral contraceptive therapies. Patients with acquired protein S deficiency have an increased risk of developing thrombotic disease [5,6]. Our case report propounds that protein S deficiency may be an additional peril factor. Level of protein S should be assessed as part of the coagulation test in all patients with dural venous sinus thrombosis and deep vein thrombosis.
The corner stone of DVST treatment is administration of anticoagulants such as low molecular weight heparin and warfarin [7].
Conclusion
Dentist often accidently diagnose maxillary sinusitis during routine radiographic examination like intraoral periapical radiograph and panoramic tomogram. Most of maxillary sinusitis patient present with pain originating from orofacial region. Severe headache, papilloedema with signs like kernig’s sign tends to preponderate in most cases of DVST. Early aggressive treatment of infection involving maxillary sinus can prevent the development of DVST.
[1]. Kim BS, Do HM, Marks MP, Diagnosis and management of cerebral venous and sinus thrombosisSeminars in Cerebrovascular Diseases and Stroke 2004 4:205-16. [Google Scholar]
[2]. Ebright JR, Pace MT, Niazi AF, Septic thrombosis of the cavernous sinusesArchives of Internal medicine 2001 161(22):2671-76. [Google Scholar]
[3]. Khandelwal S, Miller CD, Distinguishing dural sinus thrombosis from benign intracranial hypertensionEmergency Medicine Journal 2004 21(2):245-47. [Google Scholar]
[4]. Waqas M, Baig MA, Waheed S, Khursheed M, Cerebral venous sinus thrombosis with tentorial haemorrhagic infarctions in combined proteins deficiency and hyperhomocysteinemia treated with anticoagulation-limited evidence with good results: A case reportEmergency Medicine: Open Access 2016 6:1 [Google Scholar]
[5]. Chen PY, Hu HH, Chang FC, Chern CM, Protein S deficiency associated with progressive loss of vision and intracranial venous sinus thrombosisJ Chin Med Assoc 2004 67:521-26. [Google Scholar]
[6]. Iranzo A, Domingo P, Cadafalch J, Sambeat MA, Intracranial venous and dural sinus thrombosis due to protein S deficiency in a patient with AIDSJournal of Neurology, Neurosurgery, and Psychiatry 1998 64(5):688 [Google Scholar]
[7]. Shah M, Agarwal N, Gala NB, Prestigiacomo CJ, Gandhi CD, Management of dural venous sinus thrombosis in pregnancyEJVES Extra 2014 27(5):e41-42. [Google Scholar]