Prinzmetals Angina Masquerading as Acute Pericarditis
Ashwal Adamane Jayaram1, Mugula Sudhakar Rao2, R Padmakumar3, UK Abdul Razak4
1 Assistant Professor, Department of Cardiology, KMC Manipal, Manipal, Karnataka, India.
2 Resident, Department of Cardiology, KMC Manipal, Manipal, Karnataka, India.
3 Professor, Department of Cardiology, KMC Manipal, Manipal, Karnataka, India.
4 Assistant Professor, Department of Cardiology, KMC Manipal, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Abdul Razak U.K., Assistant Professor, Department of Cardiology, KMC Manipal, Manipal-576104, Karnataka, India.
E-mail: razakkaup@gmail.com
Coronary artery spasm is an intense vasoconstriction of the coronary arteries and may be responsible for the myocardial ischemia, myocardial infarction as well as sudden deaths. Coronary angiography is generally needed to identify the cause. Coronary artery spasm is a multifactorial disease with underlying mechanism still poorly understood. Here, we present case of a 48-year-old male with no significant past history who presented with acute episodic onset chest pain. Clinical, Electrocardiography (ECG) and echocardiographic findings suggested pericarditis but a diagnostic coronary angiography revealed significant coronary vasospasm. Patient’s symptoms significantly improved with calcium channel blockers and Nitroglycerine (NTG).
Coronary vasospasm, Nitroglycerine, Recurrent angina
Case Report
A 48-year-old male presented to the emergency department with acute onset chest pain. There was no history of hypertension, diabetes, Ischaemic Heart Disease (IHD) or family history of coronary artery disease. Also, there was no history of any addictions.
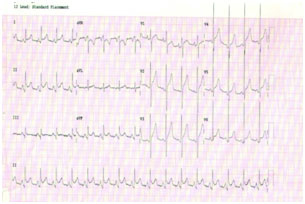
The patient reported to have multiple episodes of chest pain over the last two to three days associated with dyspnoea and low grade fever. The chest pain was atypical in nature, episodic, left sided, diffuse and non-radiating associated with no sweating or relation with position or respiration. However, admission electrocardiogram demonstrated ST-segment elevation in all the anterior and inferior leads with ST segment depression in aVR lead and presence of PR segment depression on leads I,II, aVF, V1 [Table/Fig-1]. Troponin-T was mildly elevated.
Admission ECG demonstrated ST-segment elevation in all the anterior and also inferior leads with ST segment depression in aVR lead and presence of PR segment depression on leads I,II, aVF, V1.
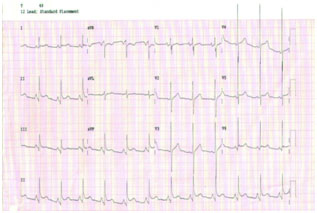
Repeat electrocardiogram after 10 hours showed resolution of ST changes in anterior chest leads with some residual ST elevations on leads V4-V6 [Table/Fig-2]. Two dimensional echocardiogram showed normal ventricular function with no regional wall motion abnormalities.
Repeat ECG after 10 hours showed resolution of ST changes in anterior chest leads with some residual ST elevations on leads V4-V6.
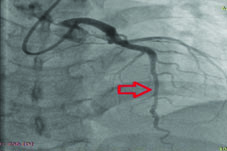
On the basis of clinical and investigational results, the diagnosis of pericarditis was made. However, as patient was unresponsive to analgesics, was taken up for diagnostic coronary angiography. Coronary angiogram revealed a Type 3 Left Anterior Descending (LAD) artery showing a long segment more than 40 mm, tubular 80% stenosis in mid part [Table/Fig-3]. After NTG we found that the stenotic segment significantly dilated [Table/Fig-4]. So, a diagnosis of vasospastic angina was made. Patient was treated with calcium channel blockers and nitroglycerine after which his symptoms significantly improved.
On angiography in PA cranial view showing LAD artery which is a type 3 vessel with an arrow depicting long segment more than 40 mm, tubular 80-85% stenosis in mid part.

On angiography in PA cranial view showing LAD artery after 200 micrograms of nitroglycerin with arrow depicting relief of vasospasm.
Discussion
Prinzmetal angina was first described in 1959 by Prinzmetal M [1]. Several factors trigger Prinzmetal angina like illicit use of cocaine, amphetamine or marijuana chemotherapy drugs, over-the-counter medication and different antibiotics [2]. Vasospastic angina can also occur without any triggering factor [3]. The classical symptom is recurrent angina at rest with spontaneous remission, preferentially occurring in the early morning hours [4]. Therapeutic management consists of calcium- channel blockers and long-term nitrates due to their vasodilatory effects [4].
Acute myopericarditis usually presents as diffuse ST segment elevation and may also be accompanied with a rise of cardiac biomarkers sometimes [5]. Some of the studies have also given examples of patients being thrombolyzed which later found out to be pericarditis [6,7]. Significant proportion of the patients presumed to be evolving myocardial infarction might indeed have pericarditis with a normal coronary angiogram [8]. As in our case, sometimes non ischemic causes of ST segment elevation present a challenge to clinicians.
Our patient presented with a history suggestive of acute pericarditis in the form of atypical anginal pain which was episodic. History of fever, normal echocardiogram along with the ECG changes supported underlying acute pericarditis. Patient was treated with analgesics and the follow up electrocardiogram showed some resolution of the changes. However, as the patient was unresponsive to the analgesics, he was taken up for the coronary angiography which revealed the diffuse tubular stenosis of mid LAD, which could be either coronary spasm (if present in both systole and diastole) or bridging due to intramyocardial course (if present at systole only). However, as it was present during both systole and diastole along with response to intracoronary nitroglycerine, the diagnosis of coronary vasospasm was made. The patient was treated with a calcium-channel blocker and nitroglycerin was continued.
Characteristics favouring coronary angiography in a patient with acute pericarditis are typical angina pain, ST segment elevation, and previous history of coronary artery disease, elevated troponin, diaphoresis and male sex [9]. Studies have revealed mild to moderate coronary artery disease (up to 35%) in patients with acute pericarditis [9]. First time a link between coronary vasospasm and inflammation has been described by Lewis JR et al., in 1978 which reported the death of the patient due to cardiogenic shock, variant angina and localized pericarditis [10].
Conclusion
The diagnosis of the coronary artery spasm has an important clinical implication as the calcium channel blockers are the preferred drugs rather than beta blockers and thrombolysis with prognosis considered benign. Our case revisits a known but rare association between the variants angina and pericarditis and stresses the importance of diagnostic milieu.
[1]. Prinzmetal M, Kennamer R, Merliss R, Wada T, Bor N, Angina pectoris. I. A variant form of angina pectoris; Preliminary reportAm J Med 1959 27:375-88. [Google Scholar]
[2]. Hung MJ, Hu P, Hung MY, Coronary artery spasm: Review and updateInt J Med Sci 2014 11(11):1161-71. [Google Scholar]
[3]. Stern S, Bayes de Luna A, Coronary artery spasm: A 2009 updateCirculation 2009 119:2531-34. [Google Scholar]
[4]. Ruisi M, Ruisi P, Rosero H, Schweitzer P, A series of unfortunate events: prinzmetal angina culminating in transmural infarction in the setting of acute gastrointestinal hemorrhageCase Reports in Cardiology 2013 2013:641348 [Google Scholar]
[5]. Nozari Y, Tajdini M, Mehrani M, Ghaderpanah R, Focal myopericarditis as a rare but important differential diagnosis of myocardial infarction; A case seriesEmergency 2016 4(3):159-62. [Google Scholar]
[6]. Smith KJ, Theal M, Mulji A, Pericarditis presenting and treated as an acute anteroseptal myocardial infarctionCan J Cardiol 2001 17(7):815-17. [Google Scholar]
[7]. Millaire A, de Groote P, Decoulx E, Leroy O, Ducloux G, Outcome after thrombolytic therapy of nine cases of myopericarditis misdiagnosed as myocardial infarctionEur Heart J 1995 16(3):333-38. [Google Scholar]
[8]. Larson DM, Menssen KM, Sharkey SW, Duval S, Schwartz RS, Harris J, “False-positive” cardiac catheterization laboratory activation among patients with suspected ST-segment elevation myocardial infarctionJAMA 2007 298(23):27:54-60. [Google Scholar]
[9]. Salisbury AC, Olalla-Gómez C, Rihal CS, Bell MR, Ting HH, Casaclang-Verzosa G, Frequency and predictors of urgent coronary angiography in patients with acute pericarditisMayo Clinic Proceedings 2009 84(1):11-15. [Google Scholar]
[10]. Lewis JR, Kisilevsky R, Armstrong PW, Prinzmetal’s angina, normal coronary arteries and pericarditisCan Med Assoc J 1978 119:36-39. [Google Scholar]