Co-infection of Candidaparapsilosis in a Patient of Pulmonary Actinomycosis-A Rare Case Report
Purbasha Ghosh1, Indrajit Gupta2, Mousumi Kar3, Poulami Nandi4, Prosenjit Naskar5
1 Assistant Professor, Department of Microbiology, Burdwan Medical College, Burdwan, West Bengal, India.
2 Post Graduate Trainee, Department of Microbiology, Burdwan Medical College, Burdwan, West Bengal, India.
3 Demonstrator, Department of Pathology, Burdwan Medical College, Burdwan, West Bengal, India.
4 Assistant Professor, Department of Microbiology, NRS Medical College, Kolkata, West Bengal, India.
5 Post Graduate Trainee, Department of Community Medicine, Burdwan Medical College, Burdwan, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Indrajit Gupta, 128/1 G.T. Road, Baidyabati, Kajipara, District Hooghly, Baidyabati-712222, West Bengal, India.
E-mail: indrajitgupta.mail@gmail.com
The diagnosis of pulmonary actinomycosis is difficult and less than 10% of cases are diagnosed at the initial presentation. Actinomycosis is always poly-microbial flora infection in human. On the other hand, Candida parapsilosis is an emerging fungal pathogen especially in immuno-compromised patients. Combined bacterial-fungal infection increases frequency and severity of the disease. This report is a case of a Candida parapsilosis co-infection in a 23-year-old male patient having pulmonary actinomycosis. This thereby could guide the clinicians towards an appropriate therapy.
Appropiate therapy, Immunosuppression, Poly-microbial flora
Case Report
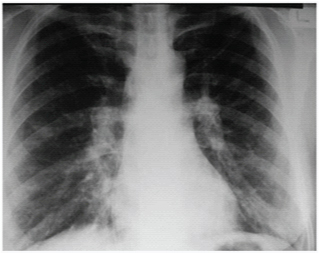
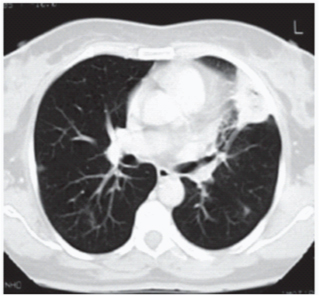
A 23-year-old male patient was brought in medicine Outpatient Department (OPD) for unconsciousness with high fever. He had a past history of nasal infection 7-8 days back accompanied with headache. Patient’s accompanied persons reported that he was smoker and alcoholic. On examination, blood pressure was 62 mm Hg/48 mm Hg; no neck stiffness; right hemi-paresis. The ECG was normal. Echocardiography showed mitral valve prolapsed with moderate mitral regurgitation. Chest X-ray showed a heterogeneous hypolucent area, with loss of substance in its centre, in the middle of the left lung field [Table/Fig-1] A Computed Tomography (CT) scan of the chest revealed a 3.8 cm mass with heterogeneous content and pleural extension to the level of the lingual [Table/Fig-2]. MRI of brain showed sub-acute haemorrhagic infarct in left basal ganglia extending to left inferior frontal region. Blood investigations showed: TLC=11800/mm3, CRP=110 mg/L, Blood glucose FBS=150 mg/dL, PPBS=259 mg/dL, Na+=133 mmol/L, K+=3.30 mmol/L. Blood culture, urine culture, and CSF culture showed no growth. Sputum for Ziehl-Neelsan (ZN) stain did not reveal acid-fast bacilli. The serum immunological study, the viral marker analysis showed no significant alterations. Colonoscopy, transabdominal pelvic ultrasound reports were normal. Bronchoscope was performed to exclude malignancy and pleural effusion was revealed. Pleural fluid was sent for microbiological analysis.
Chest X-ray showing pleural effusion.
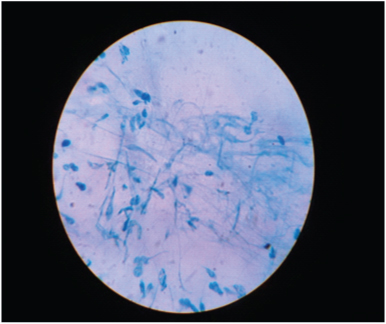
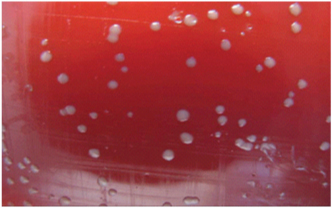
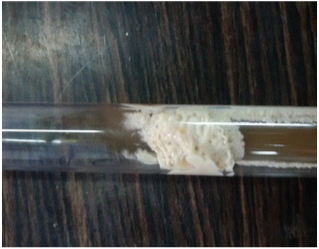
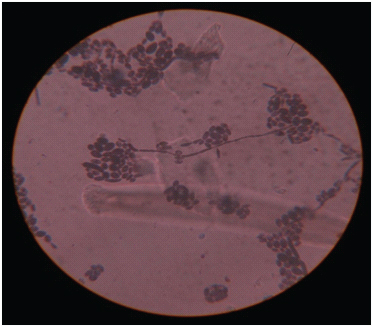
Gram-staining was done which showed non-spore forming gram-positive branching, filamentous rods. ZN showed non acid-fast bacteria [Table/Fig-3]. Then pleural fluid was cultured on nutrient agar, blood agar and Sabouraud’s Dextrose Agar (SDA) and incubated for 72 hours in both aerobic and anaerobic condition. After incubation, blood agar shows typically white-coloured rough, ‘molar tooth’ colony [Table/Fig-4]. Clinical presentation and colony morphology was suggestive of actinomyces species. On SDA media there was white, creamy, shiny and smooth growth [Table/Fig-5]. CHROM-agar Candida showed white colonies [Table/Fig-6]. Then subsequent carbohydrate assimilation and fermentation tests, germ-tube test proved that it was a fungal growth of Candida parapsilosis [1]. Gram-stain showed budding yeast cells [Table/Fig-7]. Both organisms were isolated in a pure form. Antimicrobial drug susceptibility test was performed according to CLSI guidelines [2]. The patient was gradually responding to the treatment with intravenous penicillin G 15 million units, with oral fluconazole 200 mg/day for 3 weeks.
ZN stain (pleural fluid) showing non acid fast branching filamentous bacteria with plenty of pus cells. (left to right)
Showing Molar-tooth colonies on blood agar.
Showing creamy growth of Candida on SDA slant.
CHROM-AGAR showing the white coloured confluent growth of Candida parapsilosis.

Showing budding yeast cells of Candida. (left to right)
Discussion
Actinomycosis is a non-contagious, chronic bacterial infection that occasionally occurs in human. It is caused by a facultative anaerobe, gram-positive bacterium, of the genus Actinomyces within the family Actinomycetaceae, which is filamentous and slow-growing [3]. Pulmonary actinomycosis is usually caused by aspiration of oropharyngeal secretions. The disease is typically suppurative and granulomatous [4]. On the other hand, Candida parapsilosis is an emerging fungal pathogen specially in immuno compromised situations [5]. The case report on the isolation of Candida parapsilosis along with Actinomyces species from the pleural fluid of a 23-years-old male patient further focus on this trend. The study was approved by the Institutional Human Ethical Committee and informed written consent was taken from the patients before collection of sample. The patient was a known smoker and alcoholic. He was diagnosed to have diabetes mellitus, but he had not since taken the anti-diabetic treatment regularly. Beside these, He had underlying cardiac and cerebral pathology. For unconsciousness intubation was done. It may further enrich the pulmonary actinomycosis. As a smoker he had a poor dental hygiene. These could be a reason for actinomycosis. A higher incidence of pulmonary actinomycosis has also been reported in patients with underlying respiratory disorders, such as emphysema, chronic bronchitis and bronchiectasis, and in alcoholics [6,7]. Our case presented different clinical features of conventional pulmonary actinomycosis. It is more or less asymptomatic for lung pathology. The young diabetic patient is immuno compromised due to several underlying disease factors. This facilitated the growth of C.parapsilosis. Actinomycosis is always poly-microbial flora infection [8]. C. parapsilosis is a part of the mixed infection [1]. Combined bacterial-fungal infection increases frequency and severity of the disease. This may be due to the formation of biofilm which can give resistance to both host clearance pathway and antimicrobial agents [9]. Pulmonary actinomycosis resembles several diseases like tuberculosis, nocardiosis, bronchogenic carcinoma. On X-rays, the infiltrates are dense and well circumscribed [8]. Pleural effusion is commonly found as in our case [10]. To the best of our knowledge, our present report on the isolation of C. parapsilosis as a co-pathogen with Actinomyces species in an uncontrolled diabetic patient with cardiac and cerebral pathology is the first from India.
Conclusion
Every physician should be familiar with this important though rare differential in a patient with long-standing pulmonary infiltrates to prevent unnecessary morbidity or even unwarranted surgery. Bacterial cultures and associated pathology is the mainstay of diagnosis. An antibiotic therapy was insufficient and this, in combination with an antifungal therapy resulted in a successful outcome in our case. To the best of our knowledge, this is a rare case report from India.
[1]. Chander Jagadish, Textbook of Medical Mycology 2010 3New Delhi, IndiaMeheta Publishers:266-70. [Google Scholar]
[2]. Methods for the antimicrobial dilution and the disk susceptibility testing of infrequently isolated or fastidious bacteria. Approved standard M45-A. Wayne, PA: CLSI. 2014;26:18-21 [Google Scholar]
[3]. Mabeza G, Macfarlane J, Series “unusual pulmonary infections”Eur Respir J 2003 21:545-51. [Google Scholar]
[4]. Farrokh D, Rezaitalab F, Bakhshoudeh B, Pulmonary actinomycosis with endobronchial involvement: A case report and literature reviewTanaffos 2014 13(1):52-56. [Google Scholar]
[5]. Trofa D, Gácser A, Nosanchuk JD, Candida parapsilosis, an emerging fungal pathogenClin Microbiol Rev 2008 21(4):606-25. [Google Scholar]
[6]. MabezaG F, Macfarlane J, Pulmonary actinomycosisEuropean Respiratory Journal 2003 21:545-551. [Google Scholar]
[7]. Kim SR, Jung LY, Oh IJ, Kim YC, Shin KC, Lee MK, Pulmonary actinomycosis during the first decade of 21st century: Cases of 94 patientsBMC Infectious Diseases 2013 13:216 [Google Scholar]
[8]. Valour F, Sénéchal A, Dupieux C, Karsenty J, Lustig S, Breton P, Actinomycosis: Etiology, clinical features, diagnosis, treatment, and managementInfect Drug Resist 2014 7:183-97. [Google Scholar]
[9]. Morales DK, Hogan DA, Candida albicans Interactions with Bacteria in the Context of Human Health and DiseasePLoSPathog 2010 Apr 6(4):e1000886 [Google Scholar]
[10]. Nagaoka K, Izumikawa K, Yamamoto Y, Yanagihara K, Ohkusu K, Kohno S, Multiple lung abscesses caused by actinomyces graevenitzii mimicking acute pulmonary coccidioidomycosisJournal of Clinical Microbiology 2012 50:3125-28. [Google Scholar]