The Interstitial Lung Disease (ILD) is characterized by varying degrees of fibrosis and inflammation of the lung parenchyma or interstitium and are classified together because of similar clinical, radiographic, physiologic, or pathologic features [1,2]. It includes a wide variety of conditions, individually relatively rare, but collectively found in approximately 50 per 100,000 population [3]. In India, the incidence of ILDs is not known. PH has been defined as an increase in mean Pulmonary Arterial Pressure (PAP)≥25mmHg at rest as assessed by Right Heart Catheterization (RHC) [4]. Diseases like Chronic Obstructive Pulmonary Disease (COPD) as well as bronchiectasis commonly lead to the development of Pulmonary Hypertension (PH). Hypoxic vasoconstriction plays an important role in development of pulmonary hypertension in ILD [5]. However, the effect of different pulmonary functions, arterial blood gases, saturation and various other parameters in ILDs on PH is not known. So, the correlation of spirometry and 6MWT with PH in patients with ILDs in a tertiary care hospital is studied. Therefore the present study aimed to study the correlation of following parameters of spirometry and 6MWT with PH in patients with ILD:
Materials and Methods
The study was carried out from January 2013 to September 2014 in a tertiary healthcare centre at Lokmanya Tilak Municipal Medical College and General Hospital in Mumbai, Maharashtra, India.
Study Design: It was a prospective observational clinical study.
Patient Recruitment: The patients diagnosed to have ILD above 18 years of age were selected from the outpatient as well as the inpatient department of pulmonary medicine of the same institute. The diagnosis of ILDs was made on the basis of clinical history and examination along with High Resolution Computed Tomography (HRCT) findings. Regarding sampling different types of ILD, it was difficult as adequate histopathological confirmation and various serological markers could not be done due to economic issues. So, all the ILDs with interstitial thickening (intralobular +interlobular thickening with honeycombing and in some cases GGOs) were taken.
Besides PH as per the recent European Respiratory Society (ERS) guidelines is described only at rest and not on exercise. RHC is needed to confirm the pulmonary hypertension. However, the facility was not available. Besides as per the recent ERS Guidelines, 2-D echo can be used to make probable diagnosis of PH if Pulmonary Artery Systolic Pressure (PASP) is ≥36 mmHg.
All those who were pregnant or had rheumatic or congenital heart disease as well as valvular heart disease were excluded.
The 6MWT was performed as per the American Thoracic Society (ATS) guidelines [6]. It was performed indoors, along a 24 m long, flat, straight, enclosed corridor with a hard surface. The patient was asked to sit at rest for at least 10minutes before the test starts. Pulse and blood pressure were checked. Later, at rest and post-exercise arterial blood gases were collected from the radial artery under all aseptic precautions. Patients who had oxygen saturation (SpO2) less than 90% were not allowed for the exercise test due to non-availability of portable oxygen therapy. Those having Raynaud’s phenomenon were not subjected to arterial blood gas analyses. Pulse oximetry was used to measure arterial saturation non-invasively at rest and post exercise in all the patients.
Those who had unstable angina or myocardial infarction during the previous month, resting heart rate of more than 120, a systolic blood pressure of more than 180mmHg, and a diastolic blood pressure of more than 100mmHg were not subjected to the test. During the 6MWT patients were made to walk as far as possible for 6minutes. The distance walked was measured in meters as well as percent predicted 6MWD was calculated using Enright et al., formula and for the Indian population [7,8].
Using Enright et al., formula the predicted 6MWD was calculated as:
For men, 6MWD = (7.57 x height in cm) - (5.02 x age) - (1.76 x weight in kg) - 309m, and for women, 6MWD = (2.11 x height in cm) - (2.29 x weight in kg) - (5.78 x age) + 667m [8].
Percent predicted 6MWD is calculated as: actual 6MWD/predicted 6MWD x 100
Similarily, predicted 6MWD was calculated for the Indian population:
Indian males: 561.022 - (2.507 × age [years]) + (1.505 × weight [kg]) - (0.055 × height [cm]) [8].
For Indian females: 30.325 - (0.809 × age [years]) - (2.074 × weight [kg]) + (4.235 × height [cm]) [8].
Percent predicted 6MWD was calculated as: actual 6MWD/predicted 6MWD x 100.
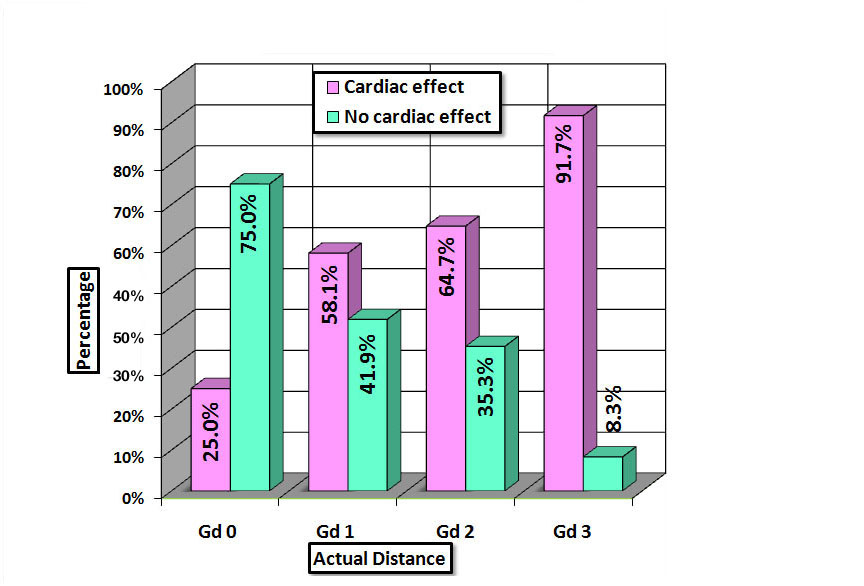
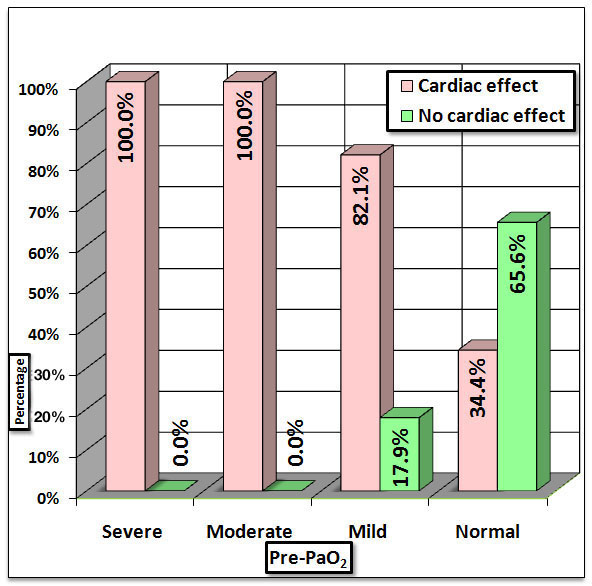
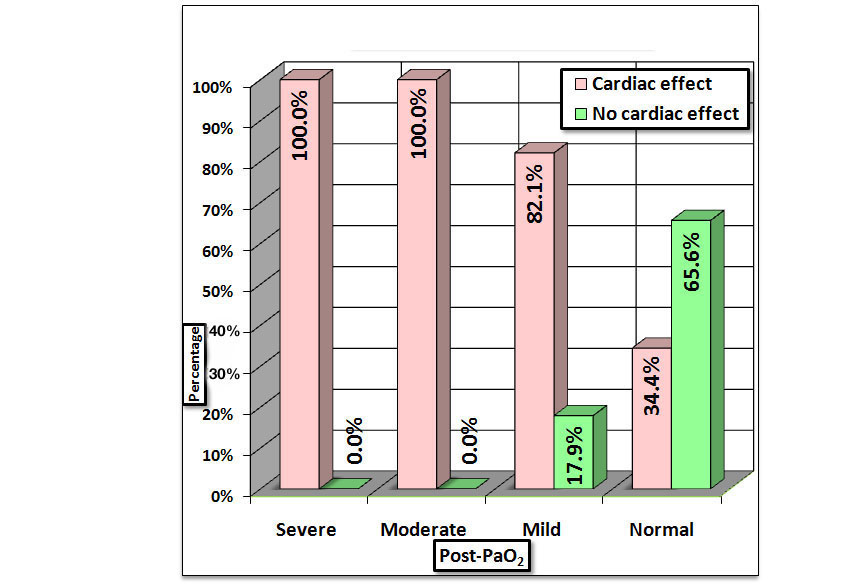
The arterial PaO2 was normal if more than or equal to 80mmHg and hypoxemia was graded as mild (60 to 79mmHg), moderate (40 to 59mmHg) and severe (40mmHg) [9]. The actual 6MWD was classified as Grade 0 (≥350m), Grade 1 (250m to 349m), Grade 2 (150m to 249m) and Grade 3 (<150m) [10].
Spirometry: The spirometry was performed and adequate spirograms which met the criteria as per the ATS guidelines 1994 were selected [11].
The FEV1% and FVC% predicted as per the joint statements on lung function testing for the ATS and the ERS were classified as normal (≥80%), mildly reduced (70-79%), moderately reduced (60-69%), moderately severe (50-59%), severe (35-49), very severe (<35) [12,13]. Cardiac effect of ILD was studied in terms of PH which was diagnosed measuring Pulmonary Artery Systolic Pressure (PASP). It was estimated using 2-D echo. PH is unlikely if PASP <36mmHg in the absence of other echocardiographic findings suggestive of PH [14]. So, in this study probable diagnosis of PH was made if PASP was ≥36mmHg. Association between qualitative variables was assessed by Chi-Square test with Continuity Correction for all 2x2 tables and Fisher’s exact test for all 2 X 2 tables where p-value of Chi-Square test was not valid due to small counts. Analysis of quantitative data (actual and %predicted 6MWD, pre- and post- exercise PaO2, desaturation, FEV1 and FVC) between the two groups (those with PH and those without PH) was done using unpaired t-test if data passes ‘Normality test’ and by Mann-Whitney Test if data fails ‘Normality test’. SPSS Version 17 was used for analysis. This study was conducted in accordance with the amended Declaration of Helsinki. The institutional ethics committees approved the protocol, and written informed consent was obtained from all patients.
Committee: Institutional Ethics Committee-Human Research
Approval No: IEC/DISS/41/12
Results
A total of 80 patients with diagnosed ILD were taken out of which 5 patients were lost to follow-up. So, 75 patients were studied. Most of the cases belonged to the age group 44 to 63 with the mean age being 50 years. Majority (59%) were female.
Out of 75 patients, only 65 could perform the exercise capacity. However arterial blood gases were taken of only 62 patients as 3 patients had Raynaud’s phenomenon. The average actual (6MWD) was 235.88 m. The mean percent predicted 6MWD using Enright et al., formula was 32.92% while that as per the Indian reference equation it was 46.17%. Approximately 31 patients could cover actual 6MWD between 250 m to 350 m. The average pre- and post- exercise PaO2 were 81.6 mmHg and 74.05 mmHg respectively. Only 2% had pre-exercise moderate hypoxemia while 27% had post-exercise moderate hypoxemia. The average difference in pre- and post-exercise PaO2 was 6.32 mmHg. The average desaturation was 2.13%. The mean FEV1 and FVC were 67.81 and 62.81 respectively. About 30% had normal FEV1 while 35% of them had mildly reduced FVC. PH correlated to 6MWT and spirometry.
A 66.66 % had PH on 2-D echo, 4% of these patients with PH also had pericardial effusion. The mean PASP of patients with PAH was 45.7 mmHg while that of patients without PAH was 28.04 mmHg. All of those who were unable to perform the test had PH. The mean actual distance in patients with PH was 235.88 m while it was 291.82 m in those without PH and so statistically significant association found (p=0.010) [Table/Fig-1]. The mean percent predicted 6MWD as per the Indian reference equation was 46.17% in those with PH and 55.67% in those without cardiac involvement and so had a significant association with PH (p=0.022). However, the percent predicted 6 minute walk distance as per the Enright et al., formula did not correlate significantly. The mean pre- and post- exercise PaO2 in those without cardiac involvement were 89.09 mmHg and 82.86 mmHg respectively while in those with cardiac involvement they were 76.19 mmHg and 67.69 mmHg respectively. So, the correlation of pre- and post-exercise PaO2 with PH was statistically significant (p=0.0002 and 0.0009 respectively) [Table/Fig-2,3]. Besides the desaturation also had a very significant association with PH (p=0.003).
Cardiac effect by actual distance.
Cardiac effect by pre-PaO2.
Cardiac effect by post-PaO2.
The mean FEV1 and FVC were 66.33% and 62.22% respectively in those with cardiac effect while they were 70.62% and 63.92% respectively in those without cardiac effect. Though the mean FEV1 and FVC were less in patients with PH, the difference was statistically not significant.
Discussion
In our study the mean age was 50 years and majority were in the age group ranged from 44 years to 63 years. About 59% were female. In another Indian study the mean age of the patients was 48 years [15]. In that same Indian study the male:female ratio was 1:2 [15]. The ILD Indian Registry started in 2011 and showed that ILDs occur at a younger age compared to the western countries, and females are affected more [16]. Only 65 out of 75 were able to perform exercise capacity because the remaining 10 were already on long term oxygen therapy and there was lack of portable oxygen therapy to perform the test. All who could not perform exercise capacity were having PH. In the 6MWT that we studied, the average actual distance was 235.88 m. Almost 51% had oxygen more than 80 mmHg while 45% had PaO2 between 60-79 mmHg. However, post exercise the percent of patients having moderate hypoxemia (40 to 60 mmHg) increased from 2 to 27%. This can be explained by the fact that there is a reduced ventilatory reserve and ventilatory limitation to exercise often seen in ILD, thus reflecting deranged pulmonary mechanics in ILD [17,18]. At rest, patients with ILD will usually have either normal or various levels of reduced PaO2. During exercise, in most patients with ILD, impressive arterial desaturation occurs. So, the post exercise PaO2 drops significantly [17]. However there is no published data which studies the average the pre- and post- exercise PaO2 in patients with ILD. As far as pulmonary functions are considered about 35% of patients had mildly reduced and about 30% had normal FEV1 there was restrictive pattern. ILD is known to have restrictive ventilatory defect in which the static expiratory Pressure-Volume (P-V) curve of the lung is shifted downward and to the right compared with normal subjects due to a reduced distensibility of the lung parenchyma [19]. It merely reflects fewer functioning alveolar units because of obliteration by the disease process and filling of the alveoli with exudate, oedema, or inflammatory material [19]. On the other hand airway function is generally well preserved and so the ratio (FEV1/FVC) is usually normal. Combining data from several large series, Gottlieb and Snider reported that the mean FVC was reduced to 63% predicted normal [19,20]. However, in our study the mean FVC was 62.81. The physiologic data from selected series of patients with idiopathic interstitial pneumonia revealed that FVC ranged from 59 to 83%.
The 6MWT is a sub-maximal exercise test used to assess functional capacity in chronic pulmonary diseases and congestive heart failure. It is also useful for evaluating patients with PH for the following reasons: (1) The ease of reproducibility; (2) The good correlation with maximal exercise testing and (3) The fact that most patients reach the endpoint of the test [21]. In our study all who were unable to perform the test had cardiac involvement. The actual 6MWD as well as % predicted 6MWD as per the Indian reference equation had a significant correlation with PH (p=0.010 and 0.022 respectively). This meant that those having PH were more likely to cover less distance in six minutes. The confounding factors like age, height and weight were removed by calculating the percent predicted 6MWD as per Indian reference equation and it was observed that % predicted 6MWD (for Indian population) was also lower in patients with PH. However % predicted 6MWD (as per Enright et al., formula) did not correlate significantly with PH. In 2004, Leuchte et al., studied 39 patients with ILD and divided them into those with echocardiographic-Estimated PASP at rest less than 35mmHg and more than 35 mmHg [22]. There was a significant reduction in exercise capacity as measured by the 6MWT in the group with elevated pulmonary artery pressures (185 meters), compared with patients who had lower pressures (304 meters) [22]. Pre- and post-exercise arterial PaO2 had a very significant association with PH (p=0.0002 and 0.0009 respectively). This meant that patients of ILD with hypoxemia are more likely to have PH. In our study, the desaturation also had a very significant association with PH (p=0.003) which meant that those with PH were likely to have higher desaturation. Hypoxic pulmonary vasoconstriction may contribute to the development of PH. But as the disease progresses and arterial hypoxemia intensifies, the level of PH also increases, and cor pulmonale begins to evolve. Exercise-induced hypoxemia is seen in both ILD and the pulmonary vascular diseases. However cardiopulmonary exercise testing revealed increased dead space ventilation and failure of the dead space ventilation to decrease with exercise when PH is present in the setting of ILD [22]. The pulmonary function tests did not distinguish those with or without PH. Although most of the patients with very severe reduction in FVC and FEV1 were observed to have PH, the association was not statistically significant. In one of the study by Leuchte et al., the FVC was somewhat higher (54%) in the group with PH as compared to that (42%) in patients with ILD having no or mild pulmonary hypertension [22]. There are few more studies which have studied FVC in selected ILD cohorts and presence of PH. For instance, in a study by Nadrous et al., 88 patients having Idiopathic Pulmonary Fibrosis (IPF) were studied and it was seen that the % predicted FVC ranged from 63.5% to72.3% [23]. In that same study about 84% of those patients had resting estimated sPAP>35mmHg while about 30.7% of them had resting estimated sPAP>50mmHg diagnosed using echocardiography [23]. In a study by Lettieri et al., which included 79 patients, PH was present in 31.6% of patients [24]. In that same study the mean % predicted FVC was 49.3% in patients having IPF with PH (resting mPAP>25mmHg using RHC) [24]. In another study by Nathan et al., which included 118 patients, PH was present in 40.7% of patients [25]. In that same study, the mean % predicted FVC was 54.6% in patients having IPF with PH (resting mPAP>25mmHg using RHC) [25].
It is a known fact that patients with PH desaturate on exercise. This study does not prove this fact. However, this study shows significant correlation of PASP with the 6MWD and the oxygen saturation. So, 6MWT is a simple and inexpensive way of monitoring the progression of PH in ILD patients.
Limitation
The major limitation of the study was that it could not categorize different types of ILDs and the sample size was small.
Conclusion
Pulmonary hypertension in ILD correlated significantly with the actual as well as the % predicted 6MWD (as per the Indian reference formula). Besides it also significantly correlated with pre- and post-exercise PaO2 as well as desaturation. However, it did not correlate with spirometry variables.