Successful Management of the Masochistic Habit in a Child with Santovuori-Haltia-Hagberg Disease (Infantile Neuronal Ceriod Lipofuscinoses)
Laresh N Mistry1, Shivayogi M Hugar2, Vidyavathi H Patil3, Punit Patel4
1 Senior Lecturer, Department of Paedodontics and Preventive Dentistry, MGM College of Dentistry, Navi Mumbai, Maharashtra, India.
2 Professor and Head, Department of Paedodontics and Preventive Dentistry, KLE VK Institute of Dental Sciences, KLE University, Belagavi, Karnataka, India.
3 Lecturer, Department of Paedodontics and Preventive Dentistry, KLE VK Institute of Dental Sciences, KLE University, Belagavi, Karnataka, India.
4 Postgraduate Student, Department of Paedodontics and Preventive Dentistry, KLE VK Institute of Dental Sciences, KLE University, Belagavi, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vidyavathi H Patil, Department of Paedodontics and Preventive Dentistry, KLE VK Institute of Dental Sciences, JNMC Campus, Nehru Nagar, Belagavi-590010, Karnataka, India.
E-mail: nisarga_vhp@yahoo.com
Self-injurious behaviours are usually related to paediatric patients with mental retardation. The management of such patients is quiet challenging to the paediatric dentists because of the difficulty to communicate with such patients regarding their feelings verbally. Here, we present a case report of successful management of self-injurious behaviour in a child with Infantile Neuronal Ceriod Lipofuscinoses (INCL).
Communication, Factitious injury, Fingernail, Mouth guard
Case Report
A one and half year-old-female toddler was referred to the Department of Paedodontics and Preventive dentistry by a Paediatric neurologist for management of orofacial Self Injurious Behaviour (SIB) of the child then diagnosed a case of INCL.
On evaluation of history, the parents revealed that the patient started with SIB when she was 10 months old. Further history revealed that at birth there was delay in cry, the patient suffered from asphyxia and convulsions and was hospitalized for the same. When the patient was 10 months old she suffered from fever and febrile seizures. The parents also reported that from past eight months the child was losing weight and the speech had still not developed. The patient had frequent seizures for which she was under medication. There were delayed developmental mile stones with motor in-coordination. The investigations of brain plain Magnetic Resonance Imaging (MRI) revealed marked bilateral symmetrical cerebral cortical atrophy with paucity of white matter and thinning of splenium of corpus callosum of brain parenchyma, moderate dilation of third and lateral ventricals which is the major feature of INCL.
On general examination the patient could not sit, stand or walk when reported to the department. There were multiple wounds on the temple and occipital region as well as on the thumb of both the hands. On oro-facial examination the patient showed large ulcer on the lower lip due to lip biting habit measuring approximately 3×2 cm2 [Table/Fig-1]. The deciduous anterior teeth showed severe attrition along with hypoplasia [Table/Fig-2]. A modified conventional mouth guard was planned for management of SIB.
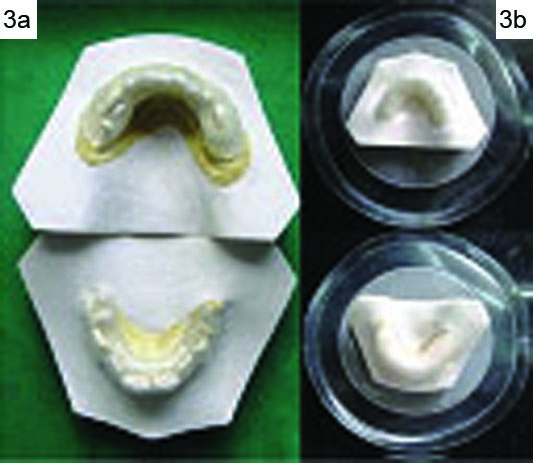
Primary impressions of maxillary and mandibular arch were made using elastomeric impression material and diagnostic casts were poured, on these casts custom stock tray were fabricated using acrylic resin material and final impressions were made using elastomeric impression material for the fabrication of conventional mouth guard. The mouth guard was fabricated initially with 2 mm thickness thermoplastic sheet (3A Medes Easy – Vac Gasket, Korea) on the maxillary cast and was delivered to the patient [Table/Fig-3a]. Due to continuous movement of the tongue the retention and stability of the mouth guard was not adequate hence to enhance stability the mouth guard was modified by adapting cold cure acrylic over it and once again a thermoplastic sheet was adopted over it. Vents were made bucco-palatally on the acrylic for the retention of the thermoplastic sheet over it [Table/Fig-3b]. A floss of 12 inches was attached to the mouth guard to prevent it’s aspiration [Table/Fig-4]. The patient was recalled every 15 days to check the healing of wounds of the thumb and oral mucosa.
Follow Up: The parents reported that there was decrease in the tendency of SIB, the ulcer on the lower lip showed signs of healing with marked reduction in size with complete healing at the end of two months. Even the thumb showed complete healing [Table/Fig-5]. The patient had also regained weight [Table/Fig-6], over a period of six months. Since then patient is kept under periodic recall.
Preoperative photographs showing trauma to the lip and thumb.

Decidious maxillary and mandibular teeth showing attrition and hypoplasia.

a) Initial Mouth guard fabrication; b) Modified Mouth guard.
Modified conventional mouth guard placed on maxillary arch.

Two months follow up showing postoperative healing of lesions. (Images left to right)

Showing the pre op and post op weight gain after 6 months.

Discussion
SIB is defined as deliberate harm to one’s body without suicidal intent [1]. They are also referred to as self-mutilating injuries, masochistic habits and factitious injury [2]. It usually manifests as hitting or banging of the head, finger and lip biting, skin cutting, oral, ocular and genital self mutilation [1]. Seventy five percent of the factitial injuries are located in the head and neck region. The oral structures commonly affected by such acts including gingiva, teeth, tooth supporting structures, lips and oral mucosa. Injury is mainly by putting foreign objects or fingernails into the oral cavity or tissue biting. These injuries may manifest as factitial ulcers, factitial gingivitis, factitial periodontitis and self extraction [3]. The prevalence of SIB in general population is estimated to be around 750 in 1,00,000 whereas, in individuals with mental retardation it is seen in nearly 81% of individuals [4].
INCL also known as Santovuori-Haltia-Hagberg disease was first described by Santovuori et al., in 1974. The most outstanding feature of this ailment is the speed with which it destroys the neurons [5]. The term Neuronal Ceriod Lipofuscinoses (NCL) was coined by Zeman and colleagues. It represents a group of inherited, neurodegenerative disorders characterized by the accumulation of auto fluorescent material in the neuronal lysosomes and other tissues [6]. Clinically this disease is characterized by microcephaly, seizures, visual failure, motor and mental deterioration leading to a vegetative state [7]. Based on the clinico-pathology and age of onset they are classified as: 1) infantile; 2) late infantile; 3) early juvenile; 4) juvenile; 5) adult; and 6) Finnish variant of late infantile form [8]. There is mutation in the CLN1 gene located on chromosome 1p32 leading to deficiency of an enzyme palmitoyl-protein thioesterase in the lysosomes in INCL [5]. The onset is between six to 12 months of life and by the end of three years the patient becomes completely unresponsive and most children die by 10 years of age [6].
SIB is commonly seen in individuals with psychotic problems, character disorder, mental retardation, coma and genetic syndromes [1]. Stewart and Kernohan have broadly classified factitial oral lesions into three types. Type: A- lesions superimposed upon pre-existing lesion, Type: B- lesions secondary to recognized habits, Type: C- those arising due to complex or unknown aetiology [9]. Common therapies used in management of SIB include behavioural modification, pharmacological management and physical restraints [3]. Although pharmacological management is feasible but it requires chronic use and the ones that are used place the patient in a chronic state of unconsciousness hence they cannot be advocated. Physical restrains are the reliable means of preventing such injuries [10]. Various oral restrains have been used in literature for SIB, these include; removable or fixed acrylic horse shoe appliance, buccal or lingual shields, soft mouth guards, thermoplastic appliances in combination of extraoral and intraoral elastics along with accessories like chin cup, special belts or clothing, facemasks and lip separators. In severe cases full mouth teeth extraction have also been done [3]. In the present case patient falls in Type: C according to Stewart and Kernohan classification, hence behavioural modification is not recommended and pharmacological management is not feasible. Hence a modified conventional mouth guard was planned for the management of SIB.
Conclusion
The severity of SIB depends on the underlying pathology and there is no definitive treatment for INCL. Treatment is purely supportive. It mainly centres on control of seizures, hyperactivity, insomnia, behaviour problems, and malnutrition and gastroesophageal reflex. Treatment has to be designed based on these circumstances and is a challenge for the paediatric dentist as the management of SIB is complicated and there are no standard techniques or treatment for such injuries. Appropriate preventive procedures have to be tailored for each of such patients based on practical consideration.
This case report is of the first kind to discuss the successful management of SIB in patients with INCL. A modified conventional mouth guard was planned for this patient based on the medical and clinical findings. This appliance has advantages like, since it is a removable appliance oral hygiene can be facilitated, the materials used in its fabrication are biocompatible and as this appliance covers only the maxillary arch side effects like dermatitis and drooling of saliva are prevented. However, it has some limitations as it requires the compliance of the patients for periodic examination, and periodic fabrication to accommodate the jaw growth.
[1]. Liang-Ru C, Jeng-Fen L, Successful treatment of self inflicted oral mutilation using an acrylic splint retained by a head gearPaediatr Dent 1996 18(5):408-10. [Google Scholar]
[2]. Subbaiah R, Thomas B, Maithreyi VP, Self-inflicted traumatic injuries of gingival-A case seriesJ Int Oral Health 2010 2(2):43-49. [Google Scholar]
[3]. Medina AC, Sogbe R, Gómez-Rey AM, Mata M, Factitial oral lesions in an autistic paediatric patientInt J Paediatr Dent 2003 13:130-37. [Google Scholar]
[4]. Silva DR, Da Foncica MA, Self injurious behaviour as a challenge for the dental practice: A case reportPaediatr Dent 2003 25(1):62-66. [Google Scholar]
[5]. Santovuori P, Neuronal ceroid-lipofuscinoses in childhoodBrain Dev 1988 10:80-83. [Google Scholar]
[6]. Zeman W, Donanne S, Dyken P, Green J, The NCL (Batten-Vogt syndrome)In: Handbook of Neurology. 10. Eds. P.J. Vinken and G.W Bruyn) 1970 AmsterdamNorth Holland Publishers:588-679. [Google Scholar]
[7]. Jalanko A, Braulke T, Neuronal ceriod lipofuscinosesBiochim Biophys Acta 2009 :697-709. [Google Scholar]
[8]. Sinha S, Satishchandra P, Santosh V, Gayatri N, Shankar SK, Neuronal ceroid lipofuscinois: A clinicopathological studySeizure 2004 13:235-40. [Google Scholar]
[9]. Stewart DJ, Kernohan DC, Self-inflicted gingival injuries: gingivitis artefacta, factitial gingivitisDent Pract Dent Rec 1972 22:418-426. [Google Scholar]
[10]. John JB, Prabhurajan V, Stalin A, Krishnan M, Masochistic habits in a child patient: A case report and its managementInt J Crit Illn Inj Sci 2013 3(3):211-13. [Google Scholar]