Difficult airway management is one of the most challenging and exciting tasks for anaesthesiologist. FB has been used very effectively for securing airway in patients with both anticipated and unanticipated difficult airways. Establishment of secure airway in patients with difficult airway is routinely done while the patient is awake after providing adequate anxiolysis while maintaining a patent airway to ensure adequate ventilation. So, fiberoptic intubation in awake state has become a gold standard for difficult airways [1]. The role of awake fiberoptic intubation has been recognized in guidelines by various societies for management of both anticipated and unanticipated difficult airways [2,3]. Intubation in awake state is associated with many discomforts as anxiety, airway obstruction, oxygen desaturation, tachycardia, and hypertension [1,4–6]. To overcome these problems, patients should be intubated while they were fully unconscious. Laryngeal Mask Airway (LMA) was used to facilitate TI in patients with difficult airway. LMA improves ventilation and facilitates fiberoptic intubation in patients which are difficult to intubate but the success rate was less [7]. In 1997 new, modified laryngeal mask, the intubating laryngeal mask airway was introduced [8]. This modified LMA has an epiglottis elevator bar at the mask aperture and a curved shaft to guide placement of an endotracheal tube into the trachea [4]. Present study was carried out to assess feasibility of FLMA to manage difficult airway as a conduit for intubation as well as for ventilation and to compare it with fiberoptic bronchoscope regarding patient’s satisfaction and comfort.
Materials and Methods
After ethical approval from the institutional ethic committee and informed consent, 60 patients with difficult airway or history of prior difficult intubation were enrolled in the study. The sample size, a power analysis of α=0.05 and β=0.80, showed that 30 patients per study group were needed.
Formula n=2 (α+β)2 σ2/(μ1−μ2)2; n=the sample size in each of the groups; μ1 = population mean in treatment Group 1; μ2 = population mean in treatment Group 2; μ1−μ2 = the difference the investigator wishes to detect; σ2 = population variance (SD); α = Type I error (0.05); β = Type II error (0.80).
A thorough pre anaesthetics check up and all necessary investigations were done in all patients. Patient with Mallampati Grade (MPG) ≥3, thyromental distance ≤6 cm, limited spine movement with normal blood pressure, pulse rate and oxygen saturation were included in the study. Patients with mouth opening <2 finger (as required for FLMA insertion), and with history of difficult ventilation were excluded from the study. Patients with anticipated difficult airway were randomly divided into two groups (n=30 of each group) using random number table. Group1: FB Group and Group 2: FLMA Group.
All the patients were monitored with pulse oximeter (SpO2), capnogram (ETCO2), Electrocardiogram (ECG), Noninvasive Blood Pressure (NIBP). The haemodynamic variables and SpO2 were recorded at baseline, induction, airway insertion, immediately post-insertion and thereafter at five minutes interval for 30 minutes. During intervention of cases a difficult airway cart which included bougies, trachlight, multiple laryngeal mask airways and combitubes was present.
In FB Group, patients were given 0.2 mg glycopyrrolate IV as an antisialagogue and sedated with midazolam (2 mg) and/or fentanyl (1μg/kg). Oropharynx and nasopharynx were anaesthetized topically with combinations of 4% lidocaine gargle and 10% lidocaine spray. For larynx and trachea superior laryngeal nerve block (1.5 ml of 2% lidocaine with adrenaline on each side) and transtracheal injection of 3 ml of 2% xylocard was given. TI was done by using 7.5 mm endotracheal tube (silicone) and fiberoptic bronchoscope of standard size. General anaesthesia was induced by propofol after confirmation of TI by end tidal CO2 (ETCO2) detection. After the failure of each attempt, patients were oxygenated and repositioned before next attempts (total three attempts) within 20 minutes. In FLMA Group, patients were pre oxygenated with 100% oxygen for three to five minutes. Induction was done by using fentanyl (1-2 μg/kg) and propofol (1-2 mg/kg). After induction, in all patients FLMA of size 4.0 was inserted and assessed for mechanical ventilation. Trial was considered as failure if more than two adjustments of FLMA were required for adequate ventilation, and patient was awakened for FB intubation. After achieving adequate ventilation, succinylcholine (1.5 mg/kg) was administered to paralyze the patient. First attempt was made blindly by inserting 7.5 mm (silicone) Endotracheal Tube (ETT) through FLMA. If TI was unsuccessful, the ETT was removed and further attempt was made with FB guidance via FLMA. Manual Positive Pressure Ventilation (PPV) with 100% oxygen was provided intermittently during TI attempts. If TI was unsuccessful after total three attempts including blind TI or total 20 minutes consumed, the trial was considered as failure and patient was awaken for FB intubation. If TI was successful, the FLMA was removed with use of ETT stabilizer. Induction Time (IT) in FB Group was from initiation of airway topicalization to introduce fiberoptic bronchoscope and TI time from the initiation of introducing of FB to ETCO2 detection from the ETT. In FLMA Group, initiation of induction with propofol to introduce FLMA was considered as IT and thereafter till ETCO2 detection from ETT was considered as TI time. Primary anaesthesiologist was the resident who has done TI under supervision of senior consultant. The initial experience was limited but equal in both FB and FLMA. Anaesthesiologist’s comfort was assessed by using a 10 point VAS. Patient’s satisfaction and morbidity was assessed on postoperative day 1 by using 10 point VAS score.
Statistical Analysis
Statistical analysis was performed by using SPSS (16.0 version) software and online graph pad calculator. Data were presented as mean (±SD), median and percentage. Patients’ demographics, haemodynamic variables and time to TI were compared using unpaired Student’s t-tests. Non-parametric variables including oxygen saturation and all VAS scores were analyzed using Mann-Whitney U-test. A p-value of <0.05 was considered significant.
Results
Demographic distribution and inclusion: The mean age and sex distribution between the two groups was statistically similar. Number of patients with anatomical abnormality, that is patients with MPG III and IV, thyromental distance <6.5 cm, limited cervical spine movement, retrognathia were 59.99% in FB Group and 63.32% in FLMA Group. Number of patients with difficulty in laryngoscopy 19.99% and history of failed laryngoscopy (more than two attempts) 19.99% in FB Group and 19.99% and 16.66% in FLMA Group, respectively. The study was comparable and difference was not statistically significant (p≥0.05) as shown in [Table/Fig-1].
| Variables | FB Groupn=30 | FLMA Groupn=30 | p-value |
|---|
| Age (mean±SD) Years | 41.07±7.041 | 40.03±6.269 | >0.05* |
| SexMaleFemale | 15 (50%)15 (50%) | 16 (53%)14 (47%) | >0.05* |
| Airway status | |
| Anatomical abnormality | 18 (59.99%) | 19 (63.32%) | >0.05* |
| Difficult laryngoscopy (>2 attempts) | 6 (19.99%) | 6 (19.99%) | >0.05* |
| History of failed laryngoscopy | 6 (19.99%) | 5 (16.66%) | >0.05* |
* Student’s t-tests
Intubation and ventilation parameters: The TI time and success of technique were almost similar between the two groups. IT in FB Group was significantly higher than FLMA Group (p<0.001). The difference between the TI time in both the groups was statistically not significant (p=0.11). In FLMA Group, 25 (83%) patients successfully ventilated in first attempt, three (10%) patients in second attempt and two (7%) in third attempt. In FLMA Group, 15 (50%) patients were blindly intubated only with FLMA. Further 8 (26.66%) were intubated with FB guidance without manipulating FLMA. Next five (16.66%) patients were intubated with FB guidance after reinsertion of FLMA whereas two (6.66%) patients could not be intubated within time. In FB Group 13 (43.29%) patients in first attempt, 10 (33.33%) in second attempt and five (16.66%) in third attempt were intubated successfully. The attempts success rate were not significantly differ in FLMA Group as compared to FB Group. The overall success rate was similar i.e., 28 (93.33%) patients were successfully intubated in both the groups [Table/Fig-2].
Comparison of intubation and ventilation indices.
| Variables | FB Group | FLMA Group | p-value |
|---|
| Induction time(min) | 11.43±1.478 | 9.8±2.355 | 0.0022*† |
| Tracheal Intubation time(min) | 2.786±0.787 | 2.448±0.827 | 0.110† |
| No. of attempts successful ventilation |
| First attempt | - | 25 | - |
| Second attempt | - | 3 | - |
| Third attempt | - | 2 | - |
| Attempts for intubation |
| First attempt (Blind intubation through FLMA) | 13(43.29%) | 15(50%) | <0.001**† |
| Second attempt (FB Guidance) | 10(33.33%) | 8(26.66%) | 0.5807† |
| Third attempt (FB Guidance) | 5(16.66%) | 5(16.66%) | - |
| Failed (number) | 2(6.66%) | 2(6.66%) | - |
* Significant (p<0.05) and ** Highly significant (p<0.001), † Student’s t-tests
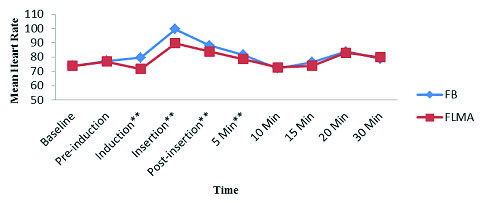
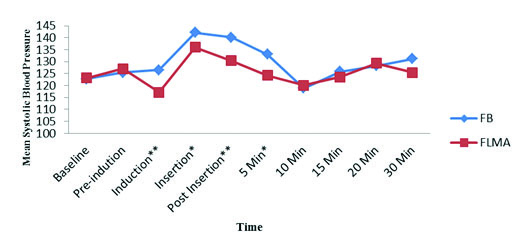
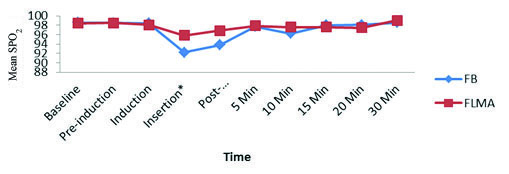
Haemodynamic variables: Statistically baseline heart rate was similar but it rose very fast during intubation. On comparison, it was significantly higher in FB Group than that in FLMA Group during induction, insertion, post-insertion and at five minutes post-insertion (p<0.001) [Table/Fig-3]. Mean systolic blood pressure increases in both the groups but on comparison, it was very significantly higher in FB Group during induction and post insertion (p<0.001) but only significantly higher (p<0.05) during insertion and five minutes post-insertion [Table/Fig-4]. Mean oxygen saturation decreases in both the group but it was rapidly decreased in FB Group. On comparison, the SpO2 was significantly lower (p<0.05) in FB Group during insertion and post insertion [Table/Fig-5]. Thus, haemodynamically patients were more stable in FLMA Group than that in FB Group.
Mean heart rate.
* Significant (p=<0.05) and ** Highly significant (p<0.001)
Comparison of mean systolic blood pressure.
* Significant (p=<0.05) and ** Highly significant (p<0.001)
Comparison of mean oxygen saturation.
* Significant (p=<0.05) and ** Highly significant (p<0.001)
Postoperative patient complications: Sore throat was similar i.e., one in both the FB Group and in FLMA Group. VAS score was 3 for hoarseness was significantly higher i.e., more incidence of hoarseness in FB Group than that in FLMA Group (p<0.001). Patient’s satisfaction score was 9 in FLMA Group versus 5 in FB Group. Statistically this difference was very significant (p<0.001). Recall of TI was significantly higher in FB Group 27% versus 0% in FLMA Group (p<0.01). The median VAS score for anaesthesiologist’s comfort with method of TI in FB Group was statistically lowered (p <0.001) compared to in FLMA Group [Table/Fig-6].
Comparison of patient’s complications and anaesthesiologist’s comfort.
| VAS Score for Different Variables | FB Groupmedian(min-max) | FLMA Group median(min-max) | p-value |
|---|
| Sore Throat(VAS 0–10, 10 worst) | 1 (0-3) | 1 (0-3) | 0.649† |
| Hoarseness(VAS 0–10, 10 worst) | 3 (0-4) | 1 (0-3) | <0.001**† |
| Satisfaction(VAS 0–10, 10 best) | 5 (2-9) | 9 (3-10) | <0.001**† |
| Anaesthesiologists Comfort(VAS 0–10, 10 best) | 7 (3-9) | 9 (4-10) | <0.001**† |
| Recall of TIFrequency (%) | 8 (26.67%) | 0 (0.00%) | <0.01*‡ |
* Significant (p=<0.05) and ** Highly significant (p<0.001), † Mann-Whitney U-test, ‡ Student’s t-tests
Discussion
In our study, in FLMA Group successful ventilation was achieved in all the patients with first attempt success rate of 83.30%. Successful intubation was achieved in 28 patients (93.33%) in both the groups. Similarly, Brain AI et al., reported the efficacy of Intubation Laryngeal Mask Airway (ILMA) and found that successful ventilation was achieved in all (100%) patients while 99.3% patients intubated successfully with first attempt success rate of 50% and fewer adjustments required for TI of patients with difficult airway [9]. Another study was conducted in patients with difficult airway to show efficacy of ILMA that showed that the insertion rate of ILMA was 96.90% and TI rate was 93% to support the results of our study [10]. Langenstien H et al., compared FLMA with Simple LMA (SLMA), and concluded that ILMA had maintained ventilation as SLMA but intubation rate was doubled [11]. The higher success rate was possible because of its unique anatomical structure which causes easy insertion into the oral cavity without any manipulation of head and neck and establishes proper alignment with airway axis. Another study showed even higher success rate of TI in which 100% patients were intubated but they had used lighted stylet through ILMA to guide TI [12]. In our study, success rate of TI in both FLMA Group and FB Group was 93.33%. In this regard the result of our study slightly differed from previous studies conducted by Watson et al. (1999), who reported that the success rate of TI in FLMA was slightly greater than FB [13]. They concluded that the intubating LMA may have slightly higher success rate and facilitate blind TI when fiberoptic intubation is unsuccessful. Similarly, Langeron O et al., and Joo HS et al., reported that the success of TI guided by intubating LMA and fiberoptic bronchoscope respectively to manage patients with difficult airway [14,15]. In this study, the IT was significantly lower in FLMA Group but TI time was similar in both FB and FLMA groups. Our study was supported by Joo HS et al., and Joo HS and Rose DK, who reported that the IT was more in FB Group due to more time taken in airway topicalization; in superior laryngeal nerve block and transtracheal block, as compared to simply induction of general anaesthesia in FLMA Group [15,16]. In our study, changes in haemodynamic variables and oxygen saturation during procedure were significantly more in FB Group than those in FLMA Group. On comparing the groups, these haemodynamic parameters were significantly higher and oxygen saturation was significantly lower in FB Group versus FLMA Group during induction, insertion, and five minutes post insertion, thereafter they settle down in both the groups. This difference was possible because of limited experience, only partial sedation, more manipulation and more time required in FB Group than in FLMA Group. A study comparing ILMA with laryngoscopic guided intubation found the similar results. He stated that the haemodynamic stress response to blind and fiberoptic guided intubation with the ILMA was less than for laryngoscope guided intubation [14]. Another study compared intubation guided by ILMA versus FB and showed that haemodynamic response was not differ but oxygen saturation was significantly lower in FB Group [16]. While another study compared TI through ILMA to the conventional direct laryngoscopy and concluded that haemodynamic response was less pronounced in patients with ILMA Group [17]. In our study, the incidence of sore throat was similar in both the groups as shown by the few previous studies [14–16]. Hoarseness was significantly lower in FLMA Group in comparison to FB Group and this finding is slightly differed from the previous study [15,16]. Lower incidence of hoarseness in FLMA Group was possible because of rapid and easy intubation due to its better anatomic design and alignment. Patient’s satisfaction VAS score in FB Group was significantly lower while recall of TI was significantly higher than FLMA Group. Similarly, Joo HS et al., and Joo HS and Rose DK, reported that recall of TI was significantly higher than FLMA [15,16]. This was because, in FLMA Group patients were completely unconscious while in FB Group they were only partially sedated before TI was done. So patients were more satisfied and lesser recall of TI in FLMA Group than in FB Group. Anaesthesiologist’s comfort with the method of TI was statistically more in the FLMA groups. This result of our study slightly differed from previous studies. Anaesthesiologist was more comfortable with fiberoptic bronchoscope [14,16]. Reason for this may be that here anaesthesiologist was the resident who has limited experience. Thus, the results of our study showed that both FB and FLMA are associated with a high degree of success. There was less adverse event or morbidity in FLMA Group. Recall of TI, patient’s and anaesthesiologist’s satisfaction was more favourable for FLMA than FB. Haemodynamic responses to TI were significantly lower in FLMA Group.
Limitation
Study limitation is the sample size. All eligible patients in a one-year period were approached. Multicentered study with larger sample size would be required for better results. The anaesthesiologists had inadequate exposure with both FLMA and FB involved in TI.
Conclusion
The present study showed that the FLMA is a useful device for managing patients with difficult airways with lower complications as compared to FB. Moreover, the patients were more satisfied and anaesthesiologist was more comfortable in FLMA Group as compared to FB Group.
* Student’s t-tests
* Significant (p<0.05) and ** Highly significant (p<0.001), † Student’s t-tests
* Significant (p=<0.05) and ** Highly significant (p<0.001), † Mann-Whitney U-test, ‡ Student’s t-tests