Radiological Outcomes of Distal Radius Fractures Managed with 2.7mm Volar Locking Plate Fixation-A Retrospective Analysis
Prem Kotian1, Srikanth Mudiganty2, Rajendra Annappa3, Jose Austine4
1 Professor, Department of Orthopaedic Surgery, Kasturba Medical College, Manipal University, Mangalore, Karnataka, India.
2 Senior Resident, Department of Orthopaedic Surgery, Kasturba Medical College, Manipal University, Mangalore, Karnataka, India.
3 Assistant Professor, Department of Orthopaedic Surgery, Kasturba Medical College, Manipal University, Mangalore, Karnataka, India.
4 Postgraduate Resident, Department of Orthopaedic Surgery, Kasturba Medical College, Manipal University, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Jose Austine, T1 Attavar Park Apartments, 6th Cross, Near KMC Hospital Attavar, Mangalore-575001, Karnataka, India.
E-mail: joseaustine10@gmail.com
Introduction
Distal radius fractures accounts for around 15% of all fractures diagnosed and treated in the emergency rooms. These fractures usually result secondary to high velocity injury such as a motor vehicle accident or fall on an out stretched hand. In the elderly, it is a common fragility fracture. Volar Locking Compression Plates (LCP) is effective devices for fixation of the distal radius fractures. There is a lacuna with regard to literature on the 2.7 mm volar LCP and the current study retrospectively assesses the postoperative radiological outcomes.
Aim
To measure the radiological outcomes in patients with displaced distal radius fractures managed with 2.7 mm volar LCP fixation using Sarmiento’s Modification of Lindstorm Criteria.
Materials and Methods
A retrospective study was conducted in the Department of Orthopaedic Surgery at Kasturba Medical College Allied Hospitals, Mangalore from May 2014 to July 2016. All displaced distal radius fractures of skeletally mature patients who underwent volar locking plate fixation between May 2014 to July 2016 and follow up with X-rays at six weeks and three months were included as part of the study. The study comprised of 20 patients and fractures were classified using the AO and Melone’s classification systems. The radiological outcome was scored based on Sarmiento’s Modification of Lindstorm Criteria.
Results
Post operative check X-rays were analysed at immediate post operative, six weeks and three months. The mean immediate post operative radial shortening, decrease in radial deviation and loss of palmar tilt were 4.08±2.23, 5.91±4.01and 4.11±3.29 respectively. The corresponding values at last follow up were 4.71±2.31, 7.9±5.13 and 4.91±3.32 respectively. No statistically significant difference (p=0.930;874;716) in radial shortening, decrease in palmar angulation and loss of radial deviation was seen till the final follow up. Sarmiento’s Modification of Lindstorm Criteria showed a good radiological outcome in 60% followed by fair in 25% and excellent in 15%.
Conclusion
Use of 2.7 mm volar LCP showed good to excellent post operative radiological outcomes in majority of the cases. The fracture reduction achieved in the immediate post operative period is maintained throughout the follow up duration.
Closed Manipulative Reduction, Locking compression plate, Sarmiento’s modification of lindstorm criteria
Introduction
Fractures of the distal end of the radius accounts to around 15% of all fractures diagnosed and treated in the emergency rooms. In the words of Dr. Abraham Colles “this fracture takes place about an inch and a half above the carpal extremity of the radius and there is a 17% lifetime probability for distal radius fractures”. The majority of these injuries are ‘closed’, with no evidence of breach of the surrounding skin [1].
A bimodal age distribution is seen, with differing trends in males and females. In females, the probability of these fractures rises with age, especially from the age of 40 years and onwards [2]; in people below the age of 40 years, the incidence is more in males [3]. In young people, these fractures usually result secondary to high velocity injury such as a motor vehicle accident or fall on an out stretched hand. While in the elderly, the fracture commonly occurs from low-energy or moderate trauma, like a fall from standing height. This is due to the fragile bone in older adults as a result of osteoporosis [4].
Management for distal radius fractures has evolved significantly over the years. Closed Manipulative Reduction (CMR) and below elbow cast application has been the main treatment [5]. However, the outcomes are often less than satisfactory with loss of reduction, limitation of function and disabilities. Several studies have shown that after a distal radius fracture, patients function more effectively when the anatomy is restored [6]. Despite this fracture being very common, we lack evidence to support a single reparative technique as against the use of others. It is difficult to compare “fractures of the distal radius” because of the many different specific patterns of lesions [7]. In addition, different plates are used for fixation, different outcome tools are used and the fractures also vary in their complexity [8].
Though we have yet to reach a consensus regarding a gold standard for surgical treatment [8], recent bio-mechanical studies have shown volar LCPs have much more rigidity and stability in comparison to traditional volar or dorsal plates [9].
Ever since volar LCP have been in use, numerous case series have demonstrated their efficacy in the fixation of distal radius fractures especially in elderly patients. While osteoporosis and poor bone quality hamper fracture stabilization, LCPs provide enhanced stability and axial loading force as compared to conventional plates [10–12]. Studies have also demonstrated good functional results (95% satisfactory) with the use of LCP in intra-articular distal radius fractures [13].
There has been an exponential increase in the use of LCP’s with more than 30 different volar plating systems in use. Studies have been done on the 2.4 mm and the 3.5 mm LCP but there is a lacuna with regard to literature on the 2.7 mm volar LCP [13–18]. The current study is being undertaken to retrospectively assess the postoperative radiological outcomes in a 2.7 mm volar LCP system used for internal stabilisation of distal radius fractures.
Materials and Methods
A descriptive study was conducted in a tertiary care hospital located in South India. Study methods were reviewed and approved by the Institutional Ethics Committee (Ref No. IEC KMC MLR 03-16/45).
The sample comprised of 20 patients. The convenience method of sampling was adopted. All displaced distal radius fractures of skeletally mature patients who were managed with volar locking plate fixation between May 2014 to July 2016 and follow up with X-Rays at six weeks and three months were included as part of the study. Distal radius AO classification type A1, Melone’s Type 1 and poly-trauma patients with an Injury Severity Score of more than 16 were excluded [19].
After approaching and priming participants regarding the study, each provided their written informed consent. Participants were assured privacy and confidentiality. Patients were counselled that participation was voluntary and they could discontinue at any time without prejudice. No honorarium was paid and data was kept confidential with restricted access. A proforma was used to collect data pertaining to patient demographics, procedure details, mode of injury, type of fracture, duration and type of immobilisation, and complications.
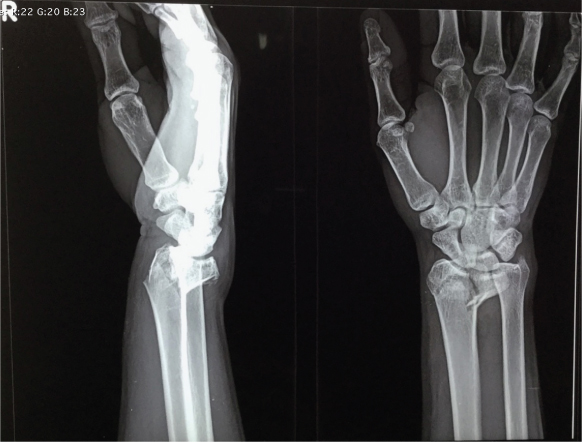
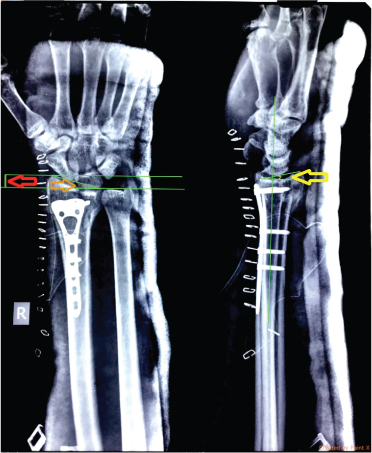
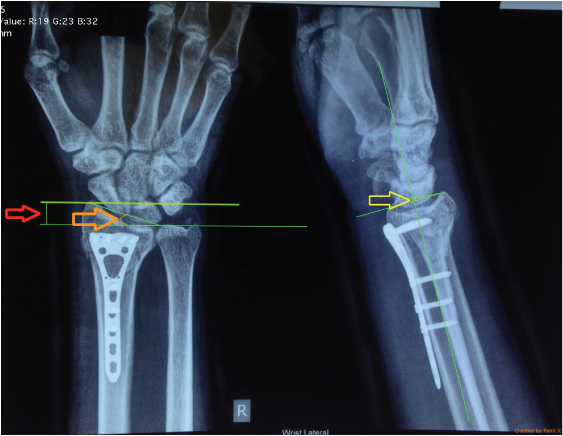
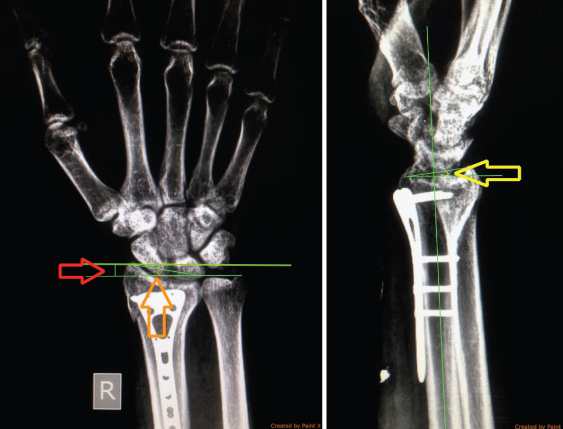
X-rays of the wrist in the anteroposterior and true lateral views, taken pre operatively [Table/Fig-1], immediate post operative [Table/Fig-2], six weeks [Table/Fig-3] and three months [Table/Fig-4] were assessed. The radiological outcome was scored based on the Sarmiento’s Modification of Lindstorm Criteria [20] which comprised of recording and grading palmar tilt, radial angulation, articular congruency and radial length.
Preoperative X-ray in anteroposterior and true lateral views showing distal radius fracture.
Immediate postoperative X-ray in antero-posterior and true lateral views after open reduction and internal fixation with 2.7 mm Volar LCP with measurements of radial length (red), radial deviation (orange) and palmar angulation (yellow).
Six weeks follow up X-ray in antero-posterior and true lateral views after open reduction and internal fixation with 2.7 mm Volar LCP with measurements of radial length (red), radial deviation (orange) and palmar angulation (yellow).
Three months follow up X-ray in antero-posterior and true lateral views after open reduction and internal fixation with 2.7 mm Volar LCP with measurements of radial length (red), radial deviation (orange) and palmar angulation (yellow).
Analysis was done using descriptive statistics. Difference between data of follow up intervals was estimated by Student’s paired t-test. A statistical package SPSS version 17.0 and MS Excel was used to do the analysis. A p-value < 0.05 was considered as significant.
Results
All patients underwent the surgical procedure under regional anaesthesia and within a week after the injury. The Modified Henry’s approach was used and all surgeries were performed by the same surgeon. The limb was immobilised in a short arm plaster splint until suture removal on the tenth post operative day. Active finger movements were initiated early followed by wrist mobilisation after three to four weeks, check X-rays of the wrist in the anter-oposterior and true lateral views were taken in the immediate post operative, six weeks and three months.
The patient demographics are elaborated in [Table/Fig-5]. The study comprised of nine (45%) females and 11 males (55%). The mean age was 46.95±13.93 with range being 24-74 years. Fall (65%) either on an outstretched arm or from height was the most common mode of injury. High energy trauma as a cause for distal radius fractures showed greater incidence in individuals <60 years. AO Type A2 was the most common fracture type encountered during this study.
Summary of patient demographics, mode of injury and fracture classification (n=20).
| Patient | Age(years) | Gender | Mode of Injury | AO Type | Melone’s Type |
|---|
| 1 | 50 | Female | Fall on outstretched arm | A2 | Type II |
| 2 | 57 | Female | Fall on outstretched arm | B1 | Type II |
| 3 | 34 | Male | Fall from Height | A2 | Type II |
| 4 | 56 | Male | Fall from height | C1 | Type III |
| 5 | 47 | Female | Fall on outstretched arm | A2 | Type II |
| 6 | 56 | Female | Motor Vehicle Accident | C3 | Type III |
| 7 | 34 | Male | Fall from height | B1 | Type II |
| 8 | 26 | Male | Motor Vehicle Accident | A3 | Type II |
| 9 | 24 | Male | Motor Vehicle Accident | C1 | Type III |
| 10 | 42 | Female | Fall on outstretched arm | B1 | Type II |
| 11 | 70 | Female | Fall on outstretched arm | A3 | Type II |
| 12 | 42 | Male | Motor Vehicle accident | A2 | Type II |
| 13 | 34 | Male | Motor Vehicle Accident | B2 | Type II |
| 14 | 39 | Male | Fall on outstretched arm | C1 | Type II |
| 15 | 74 | Female | Motor Vehicle Accident | C1 | Type III |
| 16 | 60 | Female | Fall on outstretched arm | A2 | Type II |
| 17 | 61 | Male | Fall on outstretched arm | A2 | Type II |
| 18 | 53 | Female | Fall on outstretched arm | A2 | Type II |
| 19 | 46 | Male | Motor Vehicle Accident | C3 | Type V |
| 20 | 34 | Male | Fall on outstretched arm | C1 | Type III |
Post operative check X-rays were analysed at immediate post operative, six weeks and three months. The mean immediate post operative radial shortening, loss of radial deviation and decrease in palmar tilt were 4.08±2.23, 5.91±4.01and 4.11±3.29 respectively. The corresponding values at last follow up were 4.71±2.31, 7.9±5.13 and 4.91±3.32 respectively [Table/Fig-6]. No statistically significant difference (p=0.930;874;716) in radial shortening, decrease in palmar angulation and loss of radial deviation was seen at the final follow up. These parameters were then graded and scored using the Sarmiento’s Modification of Lindstorm Criteria to assess the radiological outcome which showed that majority had a good outcome (60%) followed by fair in 25% and excellent in 15% [Table/Fig-7].
The average immediate post-operative, 6 weeks and final follow up radiographic parameters(n=20).
| Radial shortening(mm) | Loss of radial deviation(degrees) | Loss of palmar tilt(degrees) |
|---|
| Average Immediate post-operative value | 4.08±2.23 | 5.91±4.01 | 4.11±3.29 |
| Average value at 6 weeks follow up | 4.28±3.23 | 6.99±4.53 | 4.21±3.44 |
| Average value at 3 month follow up | 4.71±2.31 | 7.9±5.13 | 4.91±3.32 |
| p value(immediate vs 3 month follow up) | 0.93 | 0.87 | 0.71 |
| Student’s paired t test was used to compare means between the immediate post-operative and 3 month follow up period for three individual parameters. |
The radiological outcome based on Sarmiento’s Modification of Lindstorm Criteria (n=20).
| Frequency (Percentage) |
|---|
| Excellent | 3(15%) |
| Good | 12(60%) |
| Fair | 5(25%) |
| Poor | 0 |
Discussion
It is a well known fact that fracture of the distal radius requires accurate restoration of the anatomy and articular congruity. The co relation between incongruity and post traumatic arthritis is well established [20]. Reduced grip strength, loss of range of motion as well as instability has been noted due to misalignment [21]. Internal stabilisation of distal radius fractures provides a better restoration of the radial length as well as the volar tilt in comparison to external fixation. Locking plates provide a better technique to fix osteoporotic bones [22].
Our study has proved that there is an insignificant difference in the radial height, radial inclination and the palmar tilt in the immediate post operative and the last follow up. This highlights the fact that the fracture reduction that was achieved in the immediate post operative period is maintained throughout the follow up duration. The results are in concordance with other studies conducted using a volar LCP fixation although not the 2.7 mm volar LCP as used in our study. Rozental TD et al., and Konstantinidis L et al., found good post operative radiological outcomes with use of LCP for distal radius fracture [13,14]. A few studies have been conducted in the Indian subcontinent. Pradhan U et al., in their study concluded that treatment with open reduction and internal fixation for intra articular fractures of distal end of radius provides good radiological results [15]. Volar plate fixation also provides an overall decreased rate of complications when compared to external fixation. Moirangthem V et al., in their retrospective analysis of volar plating of distal radius fractures stated that with proper patient selection and accurate surgical techniques, volar plating continues to be a useful method of treatment for distal end radius fractures with minimal complications and allowing early return of patients to normal activities [16]. Khan MS et al., also found the use of volar LCPs for intra-articular distal radius fracture to show good results especially in comminuted distal radius fractures [17].
The 2.7 mm volar LCP is designed for fixation of complex fracture patterns especially in comminuted fractures and in the presence of osteoporosis. The smaller size of the plate and the locking screws help in addressing individual fracture fragments more precisely compared to the age old 3.5 mm system. Since the plates are much smaller, they can be placed more distally allowing sub-chondral fixation and reduced tendon and soft tissue irritation. The placement of multiple screws help in fixation of fractures in all three columns of distal radius keeping in mind the three column theory of fracture fixation [18].
The advantage of our study was that all the cases were operated at a single centre and by the same experienced orthopaedic surgeon keeping the idea and method of fracture fixation constant. The follow up examination was also done by the same team of orthopaedic surgeons. Moreover, none of our participants were lost to follow up. We believe this study has effectively demonstrated that the use of 2.7 mm volar locking plate for distal radius fracture fixation achieves good results in terms of radiological outcomes.
Limitation
The follow up of three months seems to be relatively short. A randomized controlled study is necessary to successfully highlight the advantages of this plate over other volar LCP’s and treatment modalities. A correlation with postoperative functional outcomes and a patient based subjective assessment is also desirable.
Conclusion
The use of 2.7 mm volar locking plate showed good to excellent postoperative radiological outcomes in majority of the cases. The fracture reduction achieved in the immediate postoperative period was maintained throughout the follow up duration. Therefore, the use of 2.7 mm volar locking plate for distal radius fracture fixation is a useful tool in the management of these fractures. However, a randomised controlled study is necessary to successfully highlight the advantages of this plate over other methods of fixation.
[1]. Hoare CP, Dickson DR, Armstrong DJ, Nuttall D, Watts AC, Internal fixation for treating distal radius fractures in adultsCochrane Database of Systematic Reviews 2014 7:CD011213 [Google Scholar]
[2]. McQueen MM, Court-Brown CM, Increasing age and fractures of the distal radiusCurrent Orthopaedics 2003 17(5):360-68. [Google Scholar]
[3]. Singer BR, McLauchlan GJ, Robinson CM, Christie J, Epidemiology of fractures in 15,000 adults: The influence of age and genderJournal of Bone and Joint Surgery - British Volume 1998 80(2):243-48. [Google Scholar]
[4]. McQueen M, Caspers J, Colles fracture: Does the anatomical result affect the final function?J Bone Joint Surg Br 1988 70:649-51. [Google Scholar]
[5]. Charnley J, The Closed Treatment of Common Fractures 2003 4th EditionCambridgeCambridge University Press [Google Scholar]
[6]. Obert L, Rey P, Uhring J, Gasse N, Rochet S, Lepage D, Fixation of distal radius fractures in adults: A reviewOrthopaedics & Traumatology: Surgery & Research 2013 99(2):216-34. [Google Scholar]
[7]. Chang HC, Poh SY, Seah SC, Chua DT, Cha BK, Low CO, Fragment- specific fracture fixation and double-column plating of unstable distal radial fractures using AO mini-fragment implants and Kirschner wiresInjury 2007 38:1259-67. [Google Scholar]
[8]. Leung F, Kwan K, Fang C, Distal radius fractures: Current concepts and managementBone and joint 2013 [Google Scholar]
[9]. Leung F, Zhu L, Ho H, Lu WW, Chow SP, Palmar plate fixation of AO type C2 fracture of distal radius using a locking compression plate-A biomechanical study in a cadaveric modelJ Hand Surg Br 2003 28:263-66. [Google Scholar]
[10]. Downing ND, Karantana A, A revolution in the management of fractures of the distal radius?J Bone Joint Surg Br 2008 90:1271-75. [Google Scholar]
[11]. Cordey J, Borgeaud M, Perren SM, Force transfer between the plate and the bone: relative importance of the bending stiffness of the screws friction between plate and boneInjury 2000 31(Suppl 3):C21-8. [Google Scholar]
[12]. Voigt C, Lill H, What advantages does volar plate fixation have over K-wire fixation for distal radius extension fractures in the elderly?Unfallchirurg 2006 109:845-54. [Google Scholar]
[13]. Rozental TD, Blazar PE, Functional outcome and complications after volar plating for dorsally displaced, unstable fractures of the distal radiusJ Hand Surg Am 2006 31:359-65. [Google Scholar]
[14]. Konstantinidis L, Helwig P, Strohm PC, Hirschmuller A, Kron P, Sudkamp NP, Clinical and radiological outcomes after stabilisation of complex intra-articular fractures of the distal radius with the volar 2.4mm LCPArch Orthop Trauma Surg 2010 130(6):751-57. [Google Scholar]
[15]. Pradhan U, Agrawal A, Prasad P, Chauhan V, Maheshwari R, Juyal A, Clinico- Radiological and functional outcome after surgical fixation of intraarticular fractures of distal end of radius by external fixator versus locked volar plate: A prospective randomised studyIOSR Journal of Dental and Medical Sciences 2013 6:20-26. [Google Scholar]
[16]. Moirangthem V, Bharat Kumar RJ, Vijayanand RR, Narayana Reddy M, Volar plating of distal radius fracture: A retrospective analysisJournal of Evolution of Medical and Dental Sciences 2015 4(52):9094-102. [Google Scholar]
[17]. Khan MS, Noordin S, Hashmi PM, Intra-articular distal radius fractures: Postoperative roentgenographic and functional outcomesJPMA 2016 66(3):275 [Google Scholar]
[18]. Kwan KYH, Lau TW, Leung F, Operative treatment of distal radial fractures with locking plate system-A prospective studyInternational Orthopaedics 2011 35(3):389-94. [Google Scholar]
[19]. Baker SP, O’Neill B, Haddon W Jr, Long WB, The injury severity score: A method for describing patients with multiple injuries and evaluating emergency careJ Trauma 1974 14:187-96. [Google Scholar]
[20]. Sarmiento A, Pratt GAW, Berry NC, Sinclair WF, Colles’ fractures. Functional bracing in supinationJ Bone Joint Surg Am 1975 57(3):311-17. [Google Scholar]
[21]. Gartland JJ Jr, Werley CW, Evaluation of healed Colles’ fracturesJ Bone Joint Surg Am 1951 33:895-907. [Google Scholar]
[22]. Leung F, Tu YK, Chew WY, Chow SP, Comparison of external and percutaneous pin fixation with plate fixation for intra articular distal radial fractures. A randomised studyJ Bone Joint Surg Am 2008 90(1):16-22. [Google Scholar]