Idiopathic granulomatous lesion is a rare entity of the breast seen in young-middle aged women. Diagnosis and management of granulomatous lesions with known aetiology does not impose major clinical problems. However, most often these lesions are undetected or unnoticed due to lack of timely diagnosis and inappropriate management, as primarily it is idiopathic. Hyperprolactinemia have been proposed as one of the mechanisms underlying the development of granulomatous lesions of the breast. We report a case of hyperprolactinemia due to risperidone therapy for bipolar mood disorder in a woman who eventually developed granulomatous mastitis. Histologically, the diagnosis was confirmed by the presence of granulomatous lesion and by ruling out other potential causes. In this case, raised prolactin was possibly an important factor which was secondary to risperidone therapy. However, idiopathic granulomatous mastitis could not be completely ruled out.
Anti-psychotics, Idiopathic, Non-infective, Trucut biopsy
Case Report
A 30-year-old female with the diagnosis of Bipolar Affective Disorder (BPAD) for 15 years, visited surgery outpatient department with the complaints of pain and lump in the right breast in January 2015. She was on risperidone 4 mg, two doses at night for three years. She was on lithium previously for BPAD, but discontinued due to hypothyroidism. Lump in the right breast, was insidious in onset and gradually progressive, to a size of 4x5 cm in one month. Intermittent pricking pain was present, that increased during menstrual cycles. Pain was also present in other breast for about 20 days with no lump. No history of fever, trauma or surgery and any swelling elsewhere in the body was given by the patient.
She gave birth to a child nine years ago, breast fed for six months and discontinued because of lithium carbonate. She complained of irregular menstrual cycles over the last three years. No exposure to tobacco or oral contraceptives. There was no history of diabetes, malignancy, tuberculosis, fungal diseases or autoimmune diseases.
On examination, a 4x5 cm fluctuant lump in the upper inner quadrant of the right breast was present with local rise of temperature and tenderness. Patient was afebrile, with stable vitals. No nipple discharge or skin changes like retraction or ulceration was seen. No palpable lymph nodes were present in the axilla. Left breast, nipple and axilla were normal.
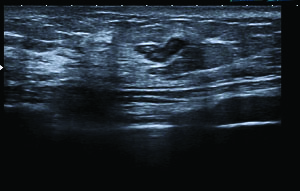
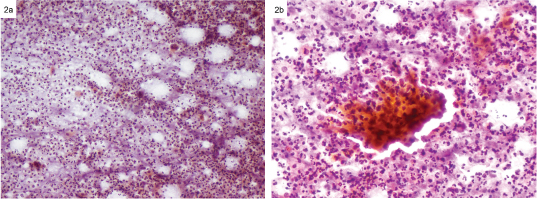
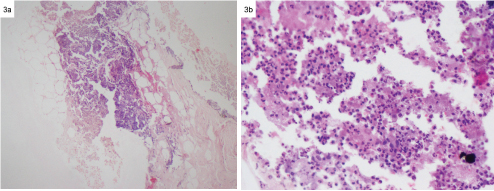
On investigating blood counts were normal. Blood culture showed no growth after 48 hours of incubation. Ultrasonography of right breast showed well defined hyperechoic lesion with peripheral hypoechoic halo seen in the supra-areolar region indicating an inflammatory lesion [Table/Fig-1]. Fine Needle Aspiration Cytology (FNAC) of the right breast lump [Table/Fig-2] showed presence of ductal epithelial cells with dense infiltrate of neutrophils, lymphocytes, histiocytic aggregates and epithelioid cells, forming granuloma with occasional multinucleated giant cells indicative of granulomatous mastitis. Wound swab, tissue culture and Polymerase Chain Reaction (PCR) were negative for Acid Fast Bacilli (AFB). Trucut biopsy [Table/Fig-3] showed an abscess with granulation tissue. Ultrasonography of abdomen and upper gastrointestinal endoscopy was normal. In suspect of infectious aetiology she was prescribed a course of antibiotic, tablet cefuroxime 500 mg twice daily for one week. Pain and redness recurred within three days with no signs of improvement. Incision and Drainage (I/D) was performed and possibility of infection was ruled out as histopathological report was negative. In view of chronic granulomatous mastitis, she was started on prednisolone 50 mg/day for 25 days. Patient was on antipsychotic medication risperidone, with history of amenorrhoea and recently developed breast lesion, her prolactin levels 59.8 ng/ ml, was estimated to be high.
Hyperechoic lesion with peripheral hypoechoic halo in right breast suggestive of inflammatory lesion.
FNAC RIGHT BREAST: a) PAP x 20- Dense aggregates of neutrophils and occasional multinucleated giant cell; b) PAP x 40- Granuloma composed of epithelioid cells and histiocytes. (Images left to right)
Trucut biopsy of right breast: a) H&E x 20 Adipose tissue with dense aggregates of neutrophils surrounded by granulation tissue; b) H&E x 40- Dense aggregates of neutrophils.
At the same time patient had poor clinical response to risperidone therapy. Raised prolactin with inadequate efficacy, therapy was changed to quetiapine. After de-challenging risperidone therapy patient condition improved, within a month along with a course of corticosteroid therapy. Ideal management could have been surgical removal of the granuloma however; surgery was called off due to altered TSH levels, poor compliance, and multiple episodes of mania, depression, unwillingness and poor socioeconomic status. Patient treatment was continued with tab. quetiapine and advised regular follow up.
Discussion
Idiopathic Granulomatous Mastitis (IGM) is a chronic inflammatory granulomatous lesion of the breast with no evidence of infection. It is a rare condition seen among women of child bearing age described first in 1972 [1]. IGM can present as discrete painful breast mass with hyperaemia, skin retraction and abscess formation. In chronic cases, clinical and radiological features are mistaken for malignancy. Diagnosis is confirmed by histopathological examination which shows non caseous granulomatous inflammation, small abscess and absence of malignant tissue. Mere presence of granulomatous tissue is not sufficient for diagnosis, due to other factors producing infectious and non-infectious granulomatous lesions of the breast, which need to be ruled out [2]. Several mechanisms have been postulated based on clinical experience and retrospective analysis of cases. Postulated aetiologies include smoking, oral contraceptive use, tumour or drug induced hyperprolactinemia and rare microbiological species of the breast flora. Ethnic origin of cases revealed most of them were from Mediterranean region and developing countries in Asia. Indeed, some of the researchers have postulated undiagnosed tuberculosis as a cause of IGM [3]. A total 200 cases have been reported with only four amongst them detected having hyperprolactinemia [4]. Among them half of the cases initially were mistaken for malignancy. Treatment depends on the severity of the disease and managed non-specifically with antibiotics, corticosteroids and immunosuppressant drugs. Even though symptomatic treatment had proven to be beneficial, surgical line of treatment is definitive [5].
The clinical course of IGM is variable, misguiding clinicians and patients. This case is of a 30-year-old woman with history of pregnancy, delivery and breast feeding which correlates well with the patho-physiological mechanisms of IGM. Extremes of age presentation have also been reported [6]. The patient was not on Oral Contraceptives (OCP) similar to a study where only 1/3rd of the cases had association of OCP use and IGM [7]. Clinical presentation correlated well with acute IGM lesions. Chronic changes like skin retraction, ulceration and fistula formation were absent similar to observations in few cases [4,7].
Mammographic and ultra sonographic evidence are insufficient as they are non specific and do not exclude other causes. A biopsy is required for confirmation with histology denoting well-formed non caseous granulomas, epithelioid histiocytes, multinucleated giant cells, lymphocytes, plasma cells and neutrophils with micro-abscess formation. Similar findings were seen in this patient after FNAC and Trucut biopsy [8,9].
Since, India is a hub for tuberculosis, it is very important to exclude this disease for management and prevention. Ziehl Neelsen’s staining of the affected tissue and wound swab were negative for AFB. Rare organisms like Corynebacterium species have caused mastitis seen in 54.8% of cases study by Taylor GB et al., [10]. This was possibly ruled out as culture of blood and wound discharge was negative for infectious organisms. These organisms are rare in humans. A full course of antibiotics for seven days did not help the patient to recover, turning towards other differential diagnosis.
In these types of cases, it is necessary to exclude known causes of granulomatous reactions of the breast. Sarcoidosis, Wegener’s granulomatosis and polyarthritis nodosa are diseases with presence of granulomas in liver, lung, kidney and blood vessels. Breast involvement is less than 1% and will not be affected unless major organs are involved. Systemic examination was normal in this case. Mammary duct ectasia is a benign condition of the breast which possesses clinical similarity to IGM presentation; histologically seen as peripheral ductal dilation with inflammation, absent in this case. Patient was non diabetic and no history of previous surgery, trauma or implants ruling out foreign body reactions [3].
Hyperprolactinemia presents as amenorrhea, galactorrhoea, infertility in women and gynaecomastia, impotence in men [11]. It can be physiological, pathological due to prolactin tumours or drug induced (due to antipsychotics, antidepressants and metoclopramide) [12]. Increased prolactin levels in non-pregnant women have been proposed as one of the mechanisms of IGM. Raised hormone is responsible for protein rich secretion accumulation in the ducts, which on extravasation into the interstitial tissue triggers an immune response, in the long run to cause granulomatous lobular mastitis. Role of prolactin via prolactin receptors in autoimmune mechanisms of skin and breast have been established [13,14].
Risperidone is an atypical antipsychotic used in conditions like schizophrenia, bipolar mood disorder, mania and dementia. It acts by blocking the D2 receptors in the pituitary, removing inhibitory effect of dopamine on prolactin secretion. Hyperprolactinemia due to risperidone is more common in comparison to other atypical antipsychotics due to its higher affinity towards dopamine receptors [12]. Effect persists even after the drug has been discontinued as it produces non cancerous tumours in the gland to continue secretion. In this case hyperprolactinemia due to risperidone could have possibly caused granulomatous lesion in the breast. Only few such cases have been reported in the past [4,15]. On assessing the causality by Naranjo scale, the relationship of the adverse drug reaction and the drug risperidone was probable [16].
Management includes changing over to a drug with lesser effect on prolactin levels like olanzapine, quetiapine or aripiprazole. Patient received antibiotics, analgesics and corticosteroids. Quetiapine was preferred antipsychotic and surgery was deferred. Literature reports and many case studies have shown successful treatment up to 80% and recurrence rates of 50% with symptomatic therapy [17].
Conclusion
Idiopathic granulomatous is a rare disease, where few cases have been reported. This report depicts a case of granulomatous mastitis in a non-pregnant woman due to hyperprolactinemia with risperidone therapy for bipolar disease. We emphasize the importance of early diagnosis of IGM, differentiating from malignancy and infections. In this case risperidone, the culprit drug could have caused the breast lesion to develop indirectly by elevating prolactin levels. Thus providing more insight to the management of drug induced hyperprolactinemia with antipsychotic therapy. There is a need for understanding the aetiology of granulomatous lesions in order to avoid unnecessary surgeries.
[1]. Kessler E, Wolloch Y, Granulomatous mastitis: A lesion clinically simulating carcinomaAm J Clin Pathol 1972 58:642-46. [Google Scholar]
[2]. Scoglie V, Wooldridge R, Leitch M, Euhus D, Sarode V, Huth J, Development and initiation of a clinical protocol for the treatment of idiopathic granulomatous mastitisJournal of Rare Disorders 2014 2(1):1-7. [Google Scholar]
[3]. Altintoprak F, Kivilcim T, Ozkan OV, Aetiology of idiopathic granulomatous mastitisWorld J Clin Cases 2014 2(12):852-58. [Google Scholar]
[4]. Lin CH, Hsu CW, Tsao TY, Chou J, Idiopathic granulomatous mastitis associated with risperidone-induced hyperprolactinemiaDiagn Pathol 2012 7(2):1-6. [Google Scholar]
[5]. Binesh F, Kargar S, Zahir ST, Behniafard N, Navabi H, Arefanian S, Idiopathic granulomatous mastitis, a clinicopathological review of 22 casesJ Clin Exp Pathol 2014 4(2):157doi:10.4172/2161-0681.1000157 [Google Scholar]
[6]. Asoglu O, Ozmen V, Karanlik H, Tunaci M, Cabioglu N, Igci A, Feasibility of surgical management in patients with granulomatous mastitisBreast J 2005 11(2):108-14. [Google Scholar]
[7]. Likhitmaskul T, Sukpanich R, Visutdiphat S, Vassanasiri W, Bilateral Idiopathic Granulomatous Mastitis: A Case ReportBangkok Medical Journal 2014 8:65-69. [Google Scholar]
[8]. Dhal I, Nayak R, Sahoo TK, Samal S, Samantara S, Idiopathic Granulomatous Mastitis of Breast and its Management: A Case ReportInternational journal of scientific study 2015 2(11):222-24. [Google Scholar]
[9]. Pistolese CA, Di Trapano R, Girardi V, Costanzo E, Di Poce I, Simonetti G, An unusual case of bilateral granulomatous mastitisCase reports in radiology 2013 dx.doi.org/10.1155/2013/694697 [Google Scholar]
[10]. Taylor GB, Paviour SD, Musaad S, Jones WO, Holland DJ, A clinicopathological review of 34 cases of inflammatory breast disease showing an association between Corynebacteria infection and granulomatous mastitisPathology 2003 35:109-19. [Google Scholar]
[11]. Majumdar A, Mangal NS, HyperprolactinemiaJ Hum Reprod Sci 2013 6(3):168-75. [Google Scholar]
[12]. La Torre D, Falorni A, Pharmacological causes of hyperprolactinemiaTher Clin Risk Manag 2007 3(5):929-51. [Google Scholar]
[13]. Omranipour R, Mohammadi SF, Samimi P, Idiopathic granulomatous lobular mastitis-report of 43 cases from Iran; Introducing a preliminary clinical practice guidelineBreast Care 2013 8(6):439-43. [Google Scholar]
[14]. Foitzik K, Langan EA, Paus R, Prolactin and the skin: A dermatological perspective on an ancient pleiotropic peptide hormoneJ Invest Dermatol 2009 129(5):1071-87. [Google Scholar]
[15]. Lin CH, Ma H, Chung MT, Chou J, Granulomatous cutaneous lesions associated with risperidone induced hyperprolactinemia in an amputated upper limbInt J Dermatol 2012 51(1):75-78. [Google Scholar]
[16]. Zaki SA, Adverse drug reaction and causality assessment scalesLung India 2011 28(2):152-53. [Google Scholar]
[17]. Mathew M, Siwawa P, Misra S, Idiopathic granulomatous mastitis: An inflammatory breast condition with review of the literatureBMJ Case Rep 2015 doi: 10.1136/bcr-2014-208086 [Google Scholar]