An Uncommon Presentation of Brucella Endocarditis Masquerading as Neurobrucellosis
Satish Venkata Pendela1, Neha Agrawal2, Thomas Mathew3, Sudha Vidyasagar4, Pujitha Kudaravalli5
1 Junior Resident, Department of Internal Medicine, Kasturba Medical College, Manipal, Karnataka, India.
2 Junior Resident, Department of Internal Medicine, Kasturba Medical College, Manipal, Karnataka, India.
3 Junior Resident, Department of Internal Medicine, Kasturba Medical College, Manipal, Karnataka, India.
4 Professor and Head of unit, Department of Internal Medicine, Kasturba Medical College, Manipal, Karnataka, India.
5 Intern, Department of Internal Medicine, Kasturba Medical College, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Satish Venkata Pendela, Junior Resident, Department of Internal Medicine, Kasturba Medical College, Manipal-576104, Karnataka, India.
E-mail: pvsatish.135@gmail.com
Brucella endocarditis is a rare but a severe complication of brucellosis, observed in less than 2% of cases. It is the main cause responsible for up to 80% of deaths in brucellosis. Herein, we present a case of brucella endocarditis that developed on a native aortic valve, but presented to us with fever for several months and acute neurological symptoms. This case report signifies the importance of considering brucella endocarditis as one of the differentials in patients presenting with Pyrexia of Unknown Origin (PUO) and Central Nervous System (CNS) manifestations.
Brucellosis, Microbiology, Infectious diseases, Pyrexia of unknown origin, Stroke
Case Report
A 35-year-old male, farmer also engaged in raising cattle, from rural part of northern Karnataka, India, presented to the emergency room with acute onset altered speech and sensorium, right upper limb and facial weakness since two days with a background of intermittent moderate grade fever with weight loss and fatigue since nine months. He never had any medical ailments or hospital admissions prior to this. He lived in a kutcha house with his wife and two children who were all in good health.
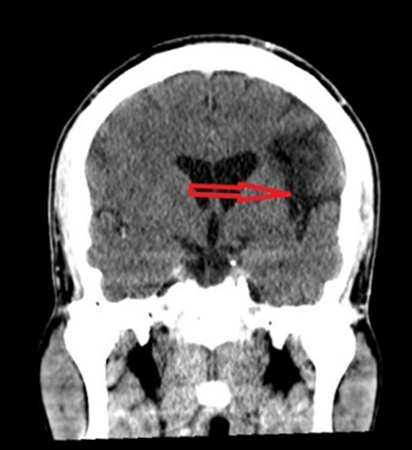
At presentation his Glasgow Coma Scale (GCS) was 14 and had minimal confusion. He was a moderately built and well nourished middle aged man. General physical examination revealed grade 3 clubbing, enlarged (2X2 cm) mobile left upper cervical superficial lymph node and moderate degree pallor. A bounding irregular pulse with a blood pressure recording of 130/40 mmHg was noted. Neurologic examination revealed Broca’s aphasia, right upper limb monoparesis and right side upper motor neuron facial palsy. Cardiovascular system examination revealed a laterally displaced hyperdynamic apex beat with precordial pulsations. A high pitched early diastolic murmur with an ejection systolic component was heard in Aortic area on auscultation. Other systemic examination did not reveal any abnormality. Routine haemogram revealed mild anaemia (Hb of 10.6 gm%) and normal total leukocyte count (5600cells/μl). CECT brain showed infarcts in the left frontal lobe [Table/Fig-1,2 and 3] and left corona radiata. An ill defined intra-axial hypodensity involving the left insular lobe with suspicious increased meningeal enhancement along the high left fronto-parietal sulci suggestive of meningoencephalitis [Table/Fig-4] was also noticed. Our potential differentials based on Pyrexia of Unknown Origin (PUO) and neurological manifestations included meningoecephalitis, systemic lupus erythematosus, retroviral illness, syphilis, infective endocarditis with systemic emboli. He was started on empirical intravenous antibiotics; Ceftriaxone (2 gm I.V. as single daily dose) while we were investigating further for the cause of his symptoms and signs. Improvement was noted in the patient’s condition as he attained near normal power the very next day without any other specific treatment. Blood and bone marrow cultures did not grow any organisms. Liver and renal function tests were normal. Scrub typhus antibodies and Weil-felix test were negative (these tests were done as Rickettsial diseases are common in this part of India). CSF analysis was done which was with in normal limits. His HIV serology, Montoux test, Syphilis serology and ANA profile were negative. As a part of PUO work up standard agglutination test for Brucella was done (as he had contact with cattle) which was positive (rising titer>1:1280). Three days later he developed one episode of transient ischemic attack involving left middle cerebral artery territory during his hospital stay in the form of motor aphasia. A 2D Echocardiography was done which showed 1.9X0.8 cm vegetation on aortic valve leaflets and sub-centric vegetation on anterior mitral leaflet.
Hypodensity in left frontal lobe suggestive of infarction.
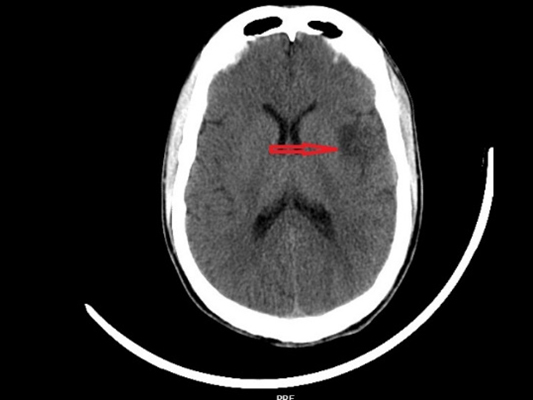
CT brain showing hypodensity in left frontal lobe.

CT brain coronal section showing hypodensity in left frontal lobe.
Contrast enhanced CT brain showing mild meningeal enhancement.

As there was history of exposure to cattle and he was having intermittent fever, diagnosis was narrowed down to systemic Brucellosis with endocarditis and embolic phenomenon, in view of high Brucella serum titers (even though blood cultures were negative) and all other PUO work-up was negative. His empirical therapy was switched over to more specific treatment with intravenous Gentamicin (5 mg/kg/day for two weeks), oral rifampin (600 mg/day for three months) and oral doxycycline (100mg twice daily for three months). Risk benefit ratio was assessed and anticoagulation was deferred for the embolic stroke. Interval cardiac surgery was planned.
Patient improved with the treatment and was discharged after complete subsidence of fever and neurological manifestations. Mitral valve replacement (with St. Jude medical-SJM 31) and Aortic valve replacement (with SJM 21) was done after three months of medical management. The valve cultures did not grow Brucella, the titers of Brucella agglutination reduced dramatically to 1:320. Postoperative ECHO showed good improvement in ejection fraction, subsequently he was started on oral anticoagulants and patient is doing better in follow up visits.
Discussion
Brucellosis is a zoonotic infection transmitted from infected animals to humans by contact with fluids. A high degree of suspicion is needed especially in young male patients and with history of exposure to farm animals [1]. Heart failure is one of the commonest causes of mortality in systemic brucellosis [2,3]. CNS manifestations like cerebro-vascular accidents, without CNS infection (Neuro-Brucellosis) are a rare presentation; no such case report has been published to the best of our knowledge. Endocarditis should be of high index suspicion in such cases. This allows an early diagnosis and appropriate medical management which can restore the valvular integrity with minimal damage. Combined medical and surgical approach is considered as the mainstay of management for brucella endocarditis [2,3].
Although endocarditis complicates only 1-2% of brucellosis cases, it is responsible for 80% of the mortality seen in brucellosis [4,5]. The patient presented to us with PUO, and his cardiac evaluation was consistent with endocarditis. Due to his history of exposure to farm animals, brucella endocarditis was suspected. Brucella endocarditis is a diagnostic challenge as yield of positive blood cultures is low, attributed to the time lag between infection and diagnosis, the fastidious nature of the organism, or due to the fact that it resides intracellularly, as with all cultures, previous antibiotic treatment interferes with culturing the organism [6]. Brucellosis can be diagnosed on either a positive blood culture, or positive serology. In a patient with a negative blood culture, a serum titre of 1:80 in a non endemic region [7], and 1:160 in an endemic region is considered diagnostic [8]. Our patient had a highly significant titre value at 1:1280, which dropped to 1:320 post treatment. Blood and bone marrow cultures were consistently sterile.
Another major complication of brucellosis is its nervous system involvement, which is seen in 2- 6.5% cases [8]. Neurobrucellosis may affect either the central nervous system manifesting as meningoencephalitis, myelo-radiculitis, cranial nerve palsies, or the peripheral nervous system, in the form of neuritis. This patient presented with a nouveau complication of brucella endocarditis; an ischemic stroke. He manifested clinically with Broca’s aphasia and right upper limb monoparesis. An initial CT scan of the brain was non diagnostic, however a subsequent contrast enhanced CT revealed an infarct in the left frontal lobe and left corona radiata. This confirmed the clinical suspicion of embolic stroke from the aortic valve vegetations. Initial management of the stroke was conservative as anticoagulation was deferred after a risk – benefit analysis deemed it to be high risk. Effective treatment includes a combination of surgery and antibiotics. Inspite of appropriate treatment, relapse rate ranges from 5-40%. The following antibiotic regimen is considered optimal; an aminoglycoside, doxycycline and rifampin, in cases with mild cardiac involvement. Patients that are diagnosed early, and do not have severe cardiac involvement can be managed with antibiotics alone. Surgical treatment is employed when; the patient has severe valvular regurgitation, massive vegetations, prosthetic valve damage, intractable cardiac failure, embolic phenomena, aneurysm of the aorta or the formation of abscess. However, surgery is not performed in acute infection, as the patient may develop para-valvular leakage. Due to the fact that this patient had vegetations of the aortic valve measuring 1.9 X0.8 cm, and that medical management was ineffective in controlling the disease, surgery was opted for. Aortic valve replacement proved the diagnosis of brucella endocarditis as the titers dropped to 1:320 following the surgery even though cultures from the valve tissues could not grow the organism.
Conclusion
Patients with PUO and stroke should be screened for brucellosis especially if a patient has history of exposure to farm animals. Management of brucella endocarditis should be started as soon as disease is identified, so that life threatening complication such as embolization of cardiac vegetations can be reduced. A combination of medical and surgical treatment is often required to treat brucella endocarditis effectively.
[1]. Agarwal SK, Rajani AR, Hussain K, Dande MM, Brucella endocarditis: an occupational hazard!BMJ Case Rep 2013 2013:piibcr2013009163 [Google Scholar]
[2]. Young EJ, An overview of human brucellosisClin Infect Dis 1995 21:283-89.quiz, 290 [Google Scholar]
[3]. Jacobs F, Abramowicz P, Vereerstraeten P, LeClerc JL, Zech F, Thys JP, Brucella endocarditis: the role of combined medical and surgical treatmentRev Infect Dis 1990 12:740-44. [Google Scholar]
[4]. Reguera JM, Alarcon A, Miralles F, Pachon J, Juarez C, Colmenero JD, Brucella endocarditis: clinical, diagnostic, and therapeutic approachEur J Clin Microbiol Infect Dis 2003 22(11):647-50. [Google Scholar]
[5]. Pappas G, Akritidis N, Bosilkovski M, Tsianos E, BrucellosisN Engl J Med 2005 352(22):2325-36. [Google Scholar]
[6]. Jeroudi MO, Halim MA, Harder EJ, Al-Siba’i MB, Ziady G, Mercer EN, Brucella endocarditisBr Heart J 1987 58(3):279-83. [Google Scholar]
[7]. Hadjinikolaou L, Triposkiadis F, Zairis M, Chlapoutakis E, Spyrou P, Successful management of Brucellamellitensis endocarditis with combined medical and surgical approachEur J Cardiothorac Surg 2001 19(6):806-10. [Google Scholar]
[8]. Sasmazel A, Baysal A, Fedakar A, Bugra O, Ozkokeli M, Buyukbayrak F, Treatment of Brucella endocarditis: 15 years of clinical and surgical experienceAnn Thorac Surg 2010 89(5):1432-36. [Google Scholar]