Paecilomyces Keratitis in Western India: A Case Report
Anmol Ulhas Naik1, Shveta Bhimashankar Gadewar2
1 Specialty Medical Officer (Ophthalmology), Department of Ophthalmology, BMC Eye Hospital, Mumbai, Maharashtra, India.
2 Specialty Medical Officer (Ophthalmology), Department of Ophthalmology, Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Mr. Anmol Ulhas Naik, B-9, Tribhuvan Jyot C.H.S., Near Gokul Bungalow, Karve Road, Dombivli West – 421202, Maharashtra, India.
E-mail: dranmolnaik@gmail.com
Cases of ocular trauma with vegetative matter are commonly encountered in ophthalmic practice in India. Many of these present with keratitis/corneal ulceration, of which fungi have a predominant share. We report a case of fungal keratitis and graft infection with Paecilomyces lilacinus, which was successfully treated with topical and systemic Voriconazole. A farmer presented with corneal ulcer and hypopyon in left eye following vegetative trauma during farming. A provisional diagnosis of fungal corneal ulcer was made based on clinical features and topical anti-fungal therapy with Natamycin was initiated. After deterioration, Therapeutic Penetrating Keratoplasty (TPK) was performed to prevent corneal perforation. Postoperatively, the graft responded well to treatment initially. Signs of graft infection appeared on the second postoperative day with perforation within 72 hours. Culture report of recipient corneal button obtained after first TPK revealed growth of P.lilacinus. A second TPK was performed and patient was started on local and oral Voriconazole. After one month follow up, the graft was clear of infection. To our knowledge, this is a rare case reported from western India, at least in recent years. With no definite consensus existing regarding management in such a scenario, extensive research is needed in this direction.
Paecilomyces lilacinus, Therapeutic penetrating keratoplasty, Voriconazole
Case Report
A 40-year-old immunocompetent farmer hailing from rural part of Maharashtra (Western India) presented with symptoms of photophobia, watering and redness in his left eye accompanied by painful loss of vision over seven to eight days. He had a history of trauma to the involved eye with a grape vine around three days prior to his symptoms. He had no history of any known systemic illness.
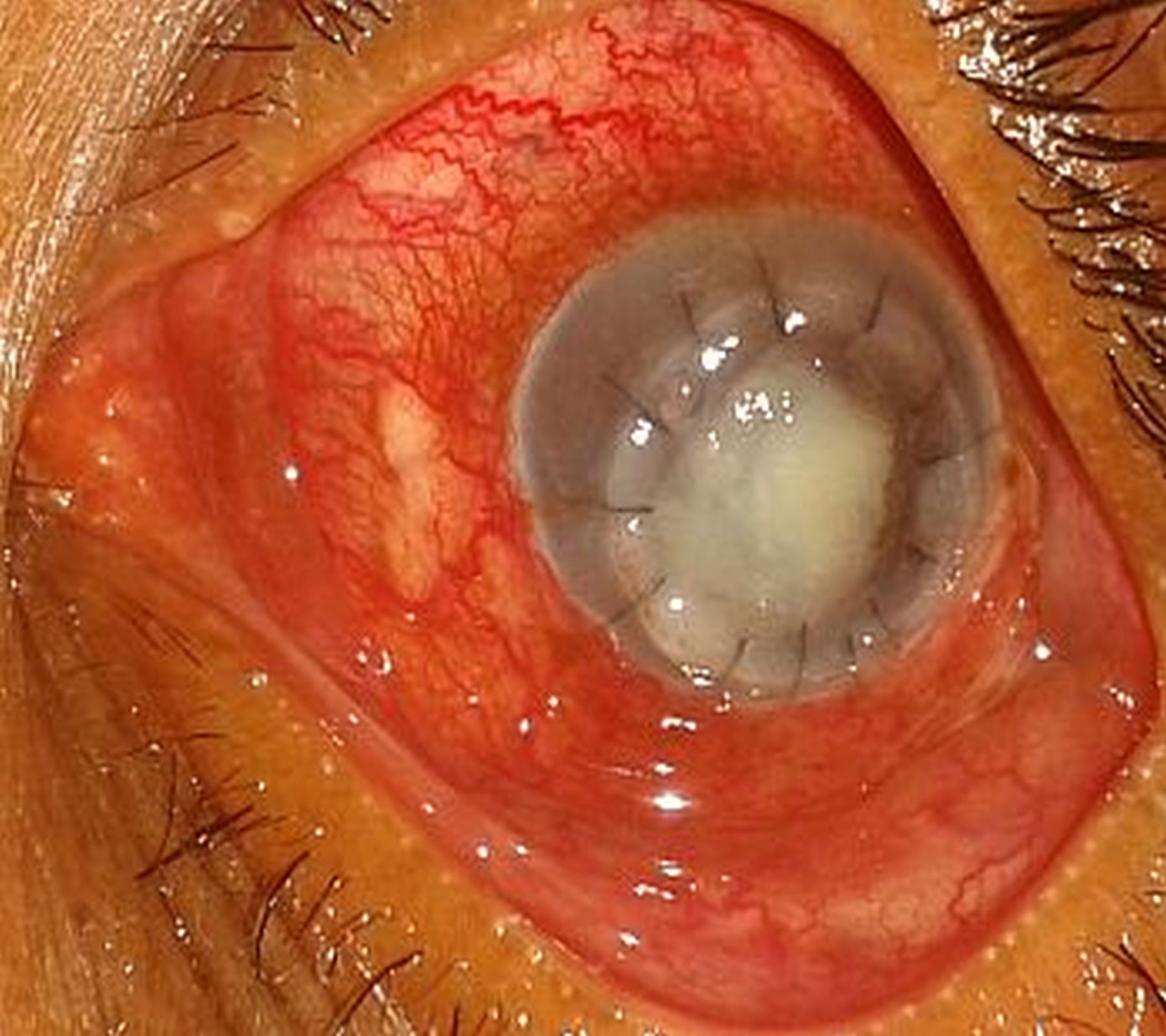
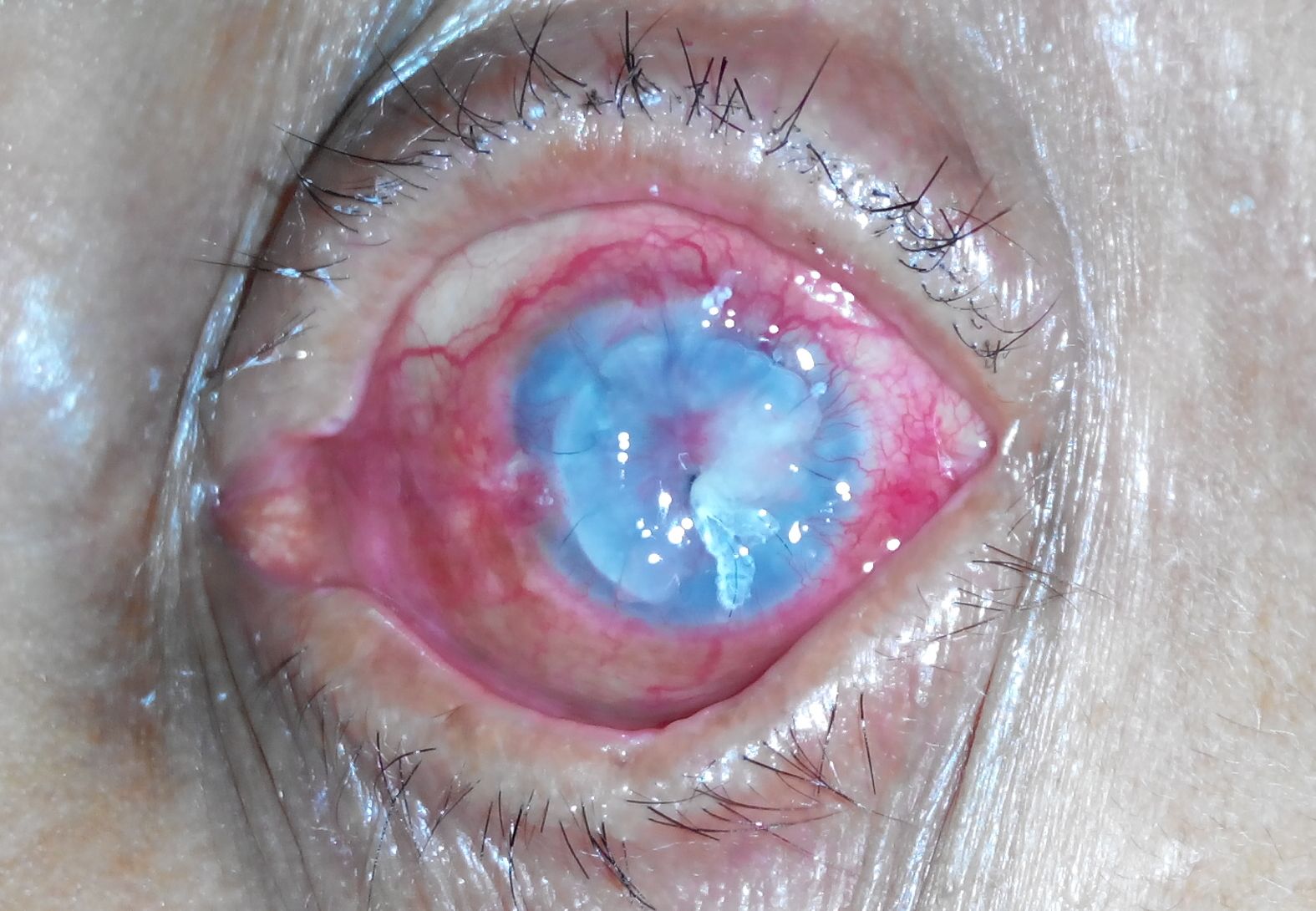
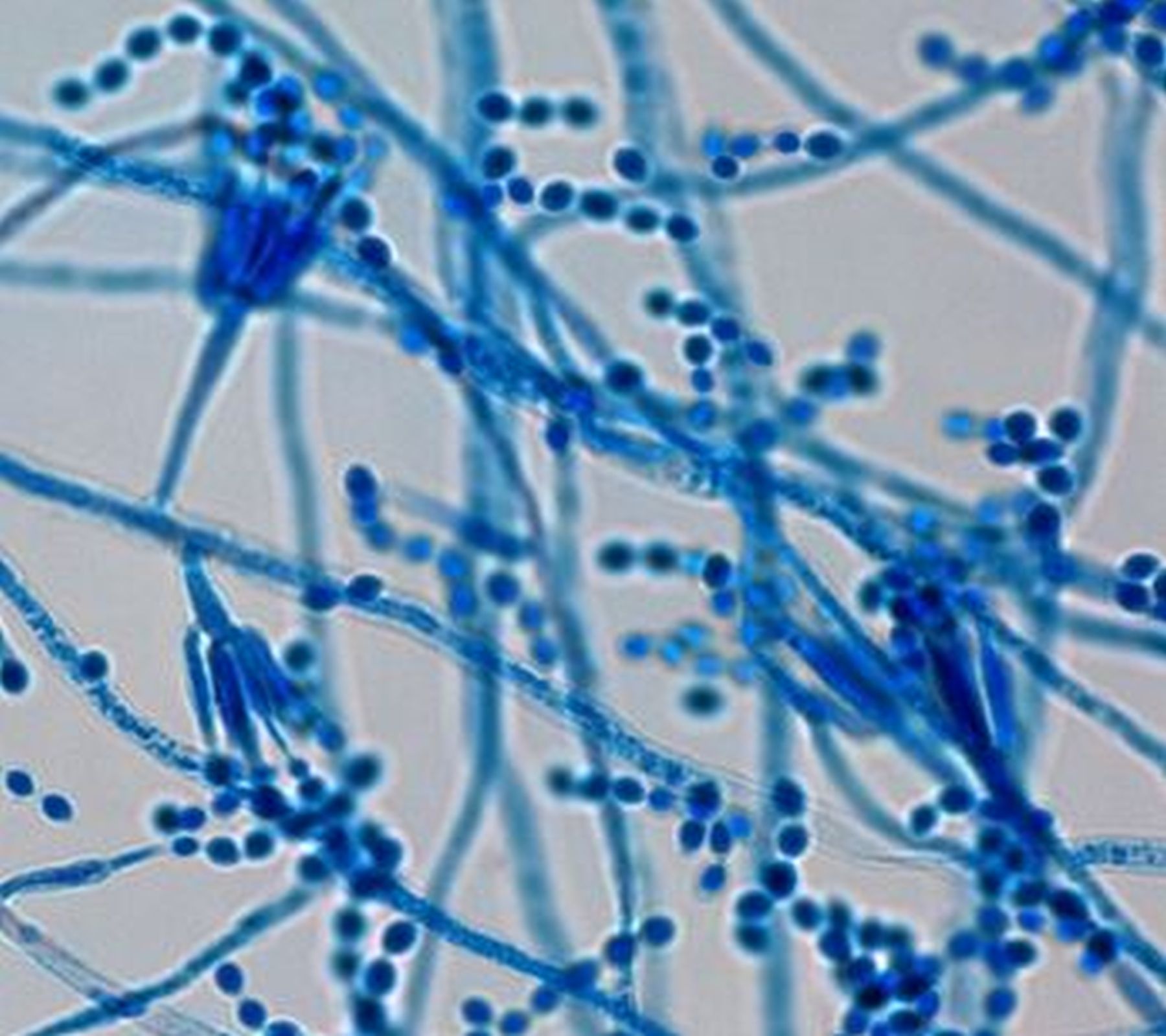
On examination, the left cornea exhibited a corneal ulcer measuring 3 mm in height and 4 mm in width with surrounding infiltrate and hypopyon [Table/Fig-1]. His Best Corrected Visual Acuity (BCVA) in the left eye was finger counting at 2 metres and that in the right eye was 20/20. Preliminary blood investigations (complete blood count, random blood sugar and serum creatinine) were normal. Corneal scrapings were sent for gram stain and potassium hydroxide (KOH) mount – both were negative. Based on the history and nature of trauma, the patient was started on Topical Moxifloxacin (0.5% qid), Tobramycin (0.3% qid), Natamycin (5% qid) eye drops and Atropine (1%) eye ointment (hora somni, i.e., at bedtime). However, there was a rapid deterioration in his ocular status within next 48 to 72 hours with an impending corneal perforation in the involved eye. Hence, a decision to perform TPK was made. Keratoplasty was performed with a 9 mm trephination of the host centre around the infiltrate with insertion of a 9.5 mm donor corneal button. The recipient corneal button was sent for gram stain, bacterial and fungal culture. Postoperatively, the patient was started on local Ofloxacin(0.3%) eye drops eight times/day, Tobramycin, Natamycin and Atropine (in doses given preoperatively). Initially the eye responded well to treatment, with clearing up of graft considerably in the first few hours. However, on the second postoperative day, there was evidence of recurrence of infection in the graft [Table/Fig-2] which rapidly progressed to an abscess and graft perforation within 72 hours [Table/Fig-3]. A TPK was performed again to remove the infected tissue. Meanwhile, within these 72 hours, the fungal culture report of the recipient corneal button of the first TPK became available and it revealed the growth of P.lilacinus fungal species. This was confirmed by lactophenol blue mount [Table/Fig-4]. Considering the fact that, P. lilacinus does not respond reliably to Natamycin and Amphotericin B [1], the patient was started on 1% topical Voriconazole eye drops six times per day and oral Voriconazole 400 mg twice a day. Postoperatively, local and systemic Voriconazole was continued for a month. He was followed up closely for a month, with no evidence of recurrence in the second graft [Table/Fig-5,6], with BCVA of counting fingers at 3 metres (in the presence of a grade three nuclear cataract).
Corneal ulcer with hypopyon at presentation;

Graft re-infection after first TPK.
Graft perforation within 72 hours after first TPK;
Microscopic section of Paecilomyces lilacinus (Magnification 400x, Stain Lactophenol blue).
Ocular picture after second TPK (first postoperative day);
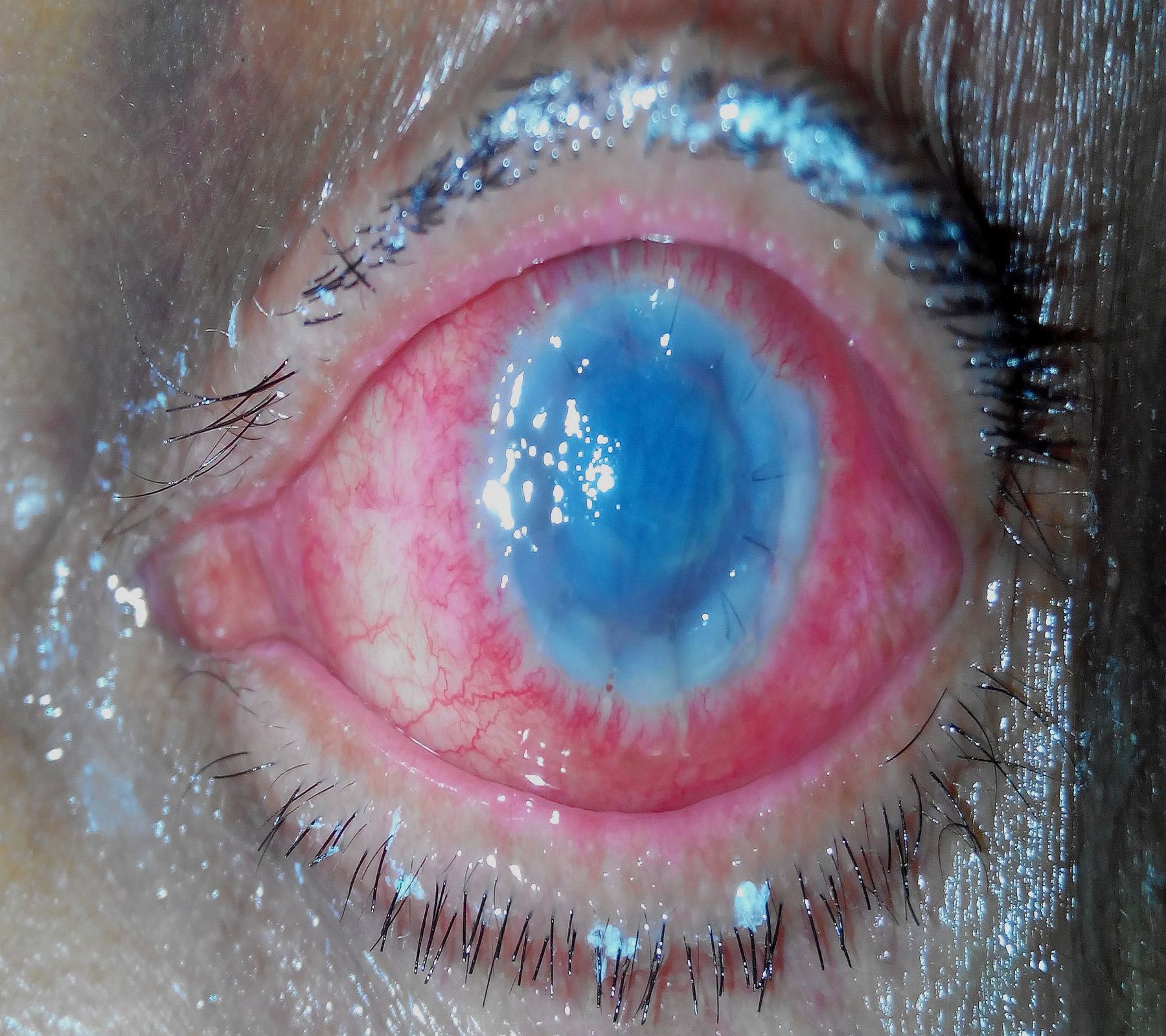
Appeareance of graft after 1 month post-op (Note - air had to be injected in the anterior chamber once as it had become shallow).

Discussion
Paecilomyces is a genus of saprobic fungi. This fungus is effective in controlling nematode populations by applying it to soil [2]. P. lilacinus is a filamentous fungus found in air and soil. Although P. lilacinus is a common saprobic fungus, P. lilacinus keratitis is a very rare, but serious disease entity. The microscopic picture of P. lilacinus demonstrates long conidiophores arising from hyphae, tapering phialides and chains of conidia [3]. The microscopic picture of our fungus was consistent with these features. The species can grow at a wide temperature range of 8°C to 38°C for a few isolates, with optimal growth in the range 26°C to 30°C, which is usually the atmospheric temperature in tropical countries. P. lilacinus is used as a biological nematocide against a wide range of plant pathogenic nematodes [4]. It is effective against eggs, larvae and adult forms. Our patient did use pesticides in his farm but could not provide the details. We believe that, this form of contact (sprayed on the grape vines) could probably have been the source of exposure.
There have been multiple reports of P. lilacinus being resistant to conventional anti-fungal agents such as Natamycin and Amphotericin B [5,6]. Voriconazole has emerged as being an effective agent against P. lilacinus [1,3,5,6]. Voriconazole, a derivative of Fluconazole, is a new triazole anti-fungal agent that interferes with fungal cell membrane synthesis [7]. Therapeutic aqueous and vitreous levels are achieved after oral administration of Voriconazole [8]. The recommended dose for topical Voriconazole administration is 1 mg/ml and that of oral administration is 200 mg every 12 hourly [9]. There is no specific consensus regarding the duration of topical and oral treatment. In this case, both modes of administration had to be continued for one month to achieve complete resolution of infection. Patients have been followed up to as long as 16 months in one study [10]. However, in our study, patient was lost to follow up after one month. Newer strategies such as intra-cameral/intra-stromal Voriconazole, Posaconazole and Echinocandins have also emerged as alternate treatment strategies in refractory cases [9]. To the best of our knowledge, this is an extremely rare case reported from Western India in the recent years. Clinically, P. lilacinus keratitis does not have any specific distinguishing features compared to other forms of fungal keratitis and the diagnosis is often delayed unless a high suspicion is held. In our case, the initial KOH mount did not reveal any fungal growth. This might have been due to inadequate sample collection/improper collecting technique. This led to a further delay in making a provisional diagnosis.
Conclusion
We reported this case to highlight the importance of suspicion of this organism to be borne in mind in cases of refractory fungal keratitis/graft recurrence. This is especially relevant due to increasing use of bio-pesticides in agriculture in developing countries of Asia and Africa.
[1]. Xiaoyong Y, Wilhelmus KR, Matoba AY, Alexandrakis G, Darlene M, Huang AJW, Pathogenesis and outcome of Paecilomyces keratitisAm J Ophthalmol 2009 147(4):691-96. [Google Scholar]
[2]. Khan A, Williams KL, Nevalainen HKM, Control of plant-parasitic nematodes by Paecilomyces lilacinus and Monacrosporium lysipagum in pot trialsBiocontrol 2006 51:643doi:10.1007/s10526-005-4241-y [Google Scholar]
[3]. Ford JG, Agee S, Greehaw ST, Successful medical treatment of a case of Paecilomyces lilacinus keratitisCornea 2008 27(9):1077-79. [Google Scholar]
[4]. Available at: http://www.agrilife.in/pdf/biopesticides/biopesti_micro/dp/Pacelo_dp.pdf Last accessed: August 2, 2014 [Google Scholar]
[5]. Deng SX, Kamal KM, Hollander DA, The use of voriconazole in the management of post-penetrating keratoplasty Paecilomyces keratitisJ Ocul Pharmacol Ther 2009 25(2):175-77. [Google Scholar]
[6]. Wu PC, Lai CH, Tan HY, Ma DHK, Hsiao CH, The successful medical treatment of a case of Paecilomyces lilacinus keratitisCornea 2010 29(3):357 [Google Scholar]
[7]. Kim KH, Kim MJ, Tehah HW, Management of fungal infection with topical and intracameral voriconazoleJ Korean Ophthalmol Soc 2008 49:1054-60. [Google Scholar]
[8]. Hariprasad SM, Mieler WF, Holz ER, Gao H, Kim JE, Chi J, Determination of vitreous, aqueous, and plasma concentration of orally administered voriconazole in humansArch Ophthalmol 2004 122:42-47. [Google Scholar]
[9]. Maharana PK, Sharma N, Nagpal R, Jhanji V, Das S, Vajpayee RB, Recent advances in diagnosis and management of Mycotic KeratitisIndian J Ophthalmol 2016 64:346-57. [Google Scholar]
[10]. Lee JA, Whitehead K, McDougall R, Management of paecilomyces keratitisEye 2007 21:262-64. [Google Scholar]