Sclerosing Pneumocytoma of the Lung: A Case Report
Vasugi Gramani Arumugam1, Leena Dennis Joseph2, Periyasamy Thangavel3, Rajendiran Swaminathan4, Ramya Rathinam Sunderaj5
1 Demonstrator, Department of Pathology, Sri Ramachandra Medical College, Chennai, Tamil Nadu, India.
2 Professor, Department of Pathology, Sri Ramachandra Medical College, Chennai, Tamil Nadu, India.
3 Professor, Department of Pathology, Sri Ramachandra Medical College, Chennai, Tamil Nadu, India.
4 Professor, Department of Pathology, Sri Ramachandra Medical College, Chennai, Tamil Nadu, India.
5 Postgraduate Student, Department of Pathology, Sri Ramachandra Medical College, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Leena Dennis Joseph, Professor, Department of Pathology, Sri Ramachandra Medical College, Chennai-600116, Tamil Nadu, India.
E-mail: leenadj@gmail.com
Pulmonary Sclerosing Pneumocytoma (PSP) is a rare tumour of the lung and is always benign. Diagnosis is made incidentally following chest X-ray or chest CT scan performed for other clinical conditions. We report a case of PSP in a seven-year-old girl who got admitted for evaluation of an anterior mediastinal mass. Clinically, thought of teratoma or other germ cell tumour the mass was excised and sent for histopathological examination. Grossly, we received a pneumonectomy specimen measuring 13x11x8 cm with a nodular firm grey white lesion in the medial aspect of lower and middle lobe measuring 7.5x5.5x5 cm. Macroscopically, pleura was involved and adherent to the lung. Microscopy showed, an ill-defined lesion in the lung with extensive fibrosis and lymphoplasmacytic infiltrate. The lesion was composed of round to oval cells with ill defined cell border, moderate eosinophilic cytoplasm and bland nuclei. A panel of Immunohistochemical (IHC) markers was performed and the lesional cells were positive for Epithelial Membrane Antigen (EMA) and Thyroid Transcription Factor-1 (TTF-1). The prognosis after surgical resection is good and the patient is doing well.
Fibrosis, Pulmonary, Thyroid transcription factor-1
Case Report
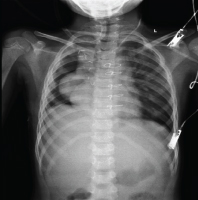
We report a case of a seven-year-old girl who presented with symptoms of recurrent episodes of dry cough, fever on and off for two years. She had normal developmental milestones and no other significant clinical history. Her physical examination was normal. Radiology suggested, an anterior mediastinal mass extending into right upper lobe infiltrating the middle and lower lobes [Table/Fig-1]. Clinically thought of as teratoma or other germ cell tumour, the mass was excised and sent for histopathological examination.
Chest X-Ray PA view showing mass in mediastinum and in the right thorax.
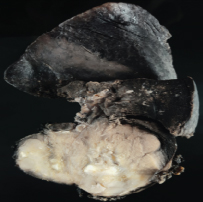
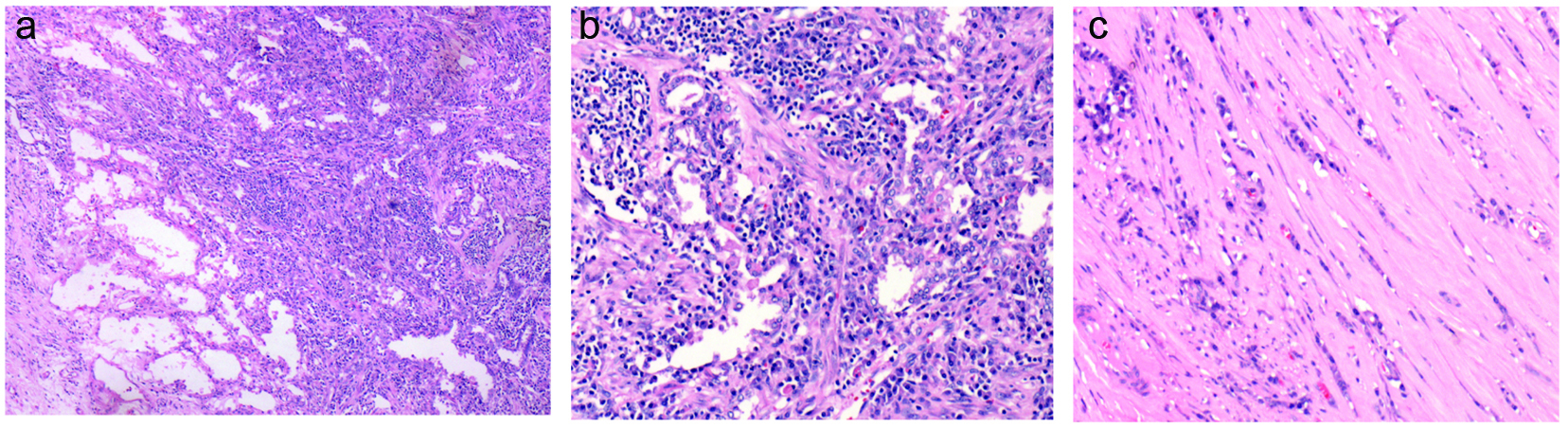
Grossly, the pneumonectomy specimen measured 13x11x8 cm. External surface showed a lesion in the lower lobe, medial aspect extending into the middle lobe. Cut surface of the lesion was grey white, hard with infiltration in to the adjacent lung and was measuring 7.5x5.5x5 cm [Table/Fig-2]. Mediastinal lymphnodes were also sent along with the lung specimen. Microscopy showed an infiltrating lesion in the lung with extensive fibrosis and lymphoplasmacytic infiltrate [Table/Fig-3a]. The lesion was composed of round to oval cells with ill defined cell border, moderate eosinophilic cytoplasm and bland nuclei arranged in tubules within the stroma [Table/Fig-3b]. Adjacent lung parenchyma showed sclerosis [Table/Fig-3c], inflammatory infiltrate predominantly composed of lymphocytes and plasma cells, along with oedema in alveoli with desquamation secondary to obstruction.
Gross image showing firm, white nodular lesion infiltrating lung parenchyma.
(a) Section showing infiltrative lesion with lymphoplasmacytic infiltrate (H&E x100). (b) Section showing peripheral cuboidal cells and round to oval stromal cells (H&E x200). (c) Section showing sclerosis adjacent to lesion (H&E x200).
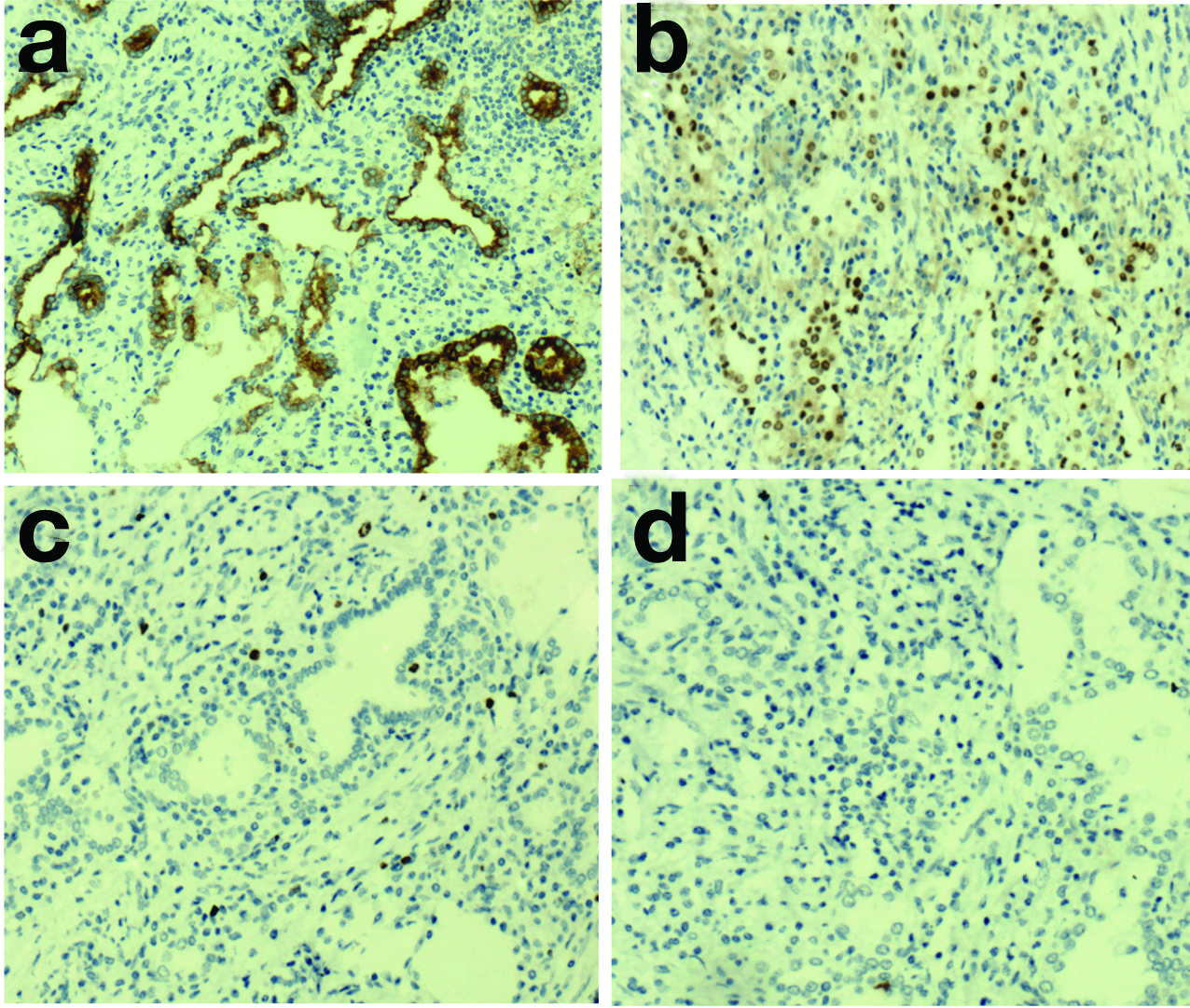
Differential diagnoses on light microscopy were Pulmonary Sclerosing Pneumocytoma (PSP), primary pulmonary neoplasm, Sugar tumour and metastatic adenocarcinoma. A panel of IHC markers were performed [Table/Fig–4]. By IHC the tubular cells were positive for EMA, TTF-1 [Table/Fig–5a,b]. Background stroma was positive for vimentin and Smooth muscle actin (SMA). Ki 67 labelling index was 1% [Table/Fig–5c] Stains for Human Melanoma Black-45 (HMB 45) [Table/Fig–5d]. Estrogen receptor (ER), Progesterone receptor (PR) were negative. The mediastinal lymphnodes showed reactive changes. The histological examination and IHC findings confirmed the diagnosis of sclerosing pneumocytoma with no mediastinal lymph node invasion. The prognosis after surgical resection was good.
Panel of immunohistochemical markers done.
| IHC Markers | Inference |
|---|
| EMA, TTF-1 | Positive in the tubular cells |
| Vimentin, SMA | Positive in the background stromal cells |
| HMB 45, ER, PR | Negative |
| Ki-67 labelling index | 1% |
(a) EMA positivity in the lesional cells (IHC x 200). (b) TTF-1 positivity in the cells (IHC x 200). (c) Ki-67 labelling in the lesional cells (IHC x 200). (d) HMB 45 negative staining (IHCx 200).
Discussion
PSP is a rare neoplasm of the lung first described by Liebow and Hubbell [1]. It has a female preponderance (male to female ratio 1:5) and affects middle aged Asian women. It is also called as sclerosing haemangioma due to the presence of prominent sclerosis and vascularization. Clinically, most patients are asymptomatic but some may present with recurrent cough, breathing difficulties, chest pain or haemoptysis [2–4]. Most of the diagnosis are made incidentally when the patient is subjected to radiological examination for other symptoms.
PSP commonly occurs in the peripheral lung parenchyma and can affect any lobe. Radiologically, it appears as a solitary, well defined, round to oval, homogenous dense mass that enhances with contrast. Few may show calcification or cystic changes. If the lesion is pleural based and polypoid, it mimics solitary fibrous tumour. Presence of “air meniscus sign” is a clue to the diagnosis of pneumocytoma [4]. Grossly, it appears as an irregular, firm, grey white nodule which sometimes may be associated with haemorrhage, calcifications or cysts.
Microscopically, the lesion has two components peripheral cuboidal cells and round to oval stromal cells. The lesional cells are arranged in a papillary pattern with intervening sclerotic and haemorrhagic areas. They has a bland appearance with relatively less or no cytological atypia. The present lesion showed admixure of lymphoplasmacytic cells in the adjacent areas. Proliferative index is generally low. Differential diagnosis includes primary pulmonary neoplasms, carcinoid tumour, metastatic deposit from a papillary tumour, sugar tumour. IHC and the bland cytology of the lesional cells help in differentiating sclerosing pneumocytoma from other possibilities. TTF-1 and EMA are positive in peripheral cuboidal and stromal cells. Similar case reports of PSP have been found in literature with their clinical presentation and treatment [Table/Fig-6] [5–9].
Similar case reports In literature [5–9].
| Reference | Patient details | IHC workup | Treatment |
|---|
| Ouafi L et al., [5] | 66/F, diagnosed in CT performed for staging of breast cancer | TTF-1, EMA positive in surface and stromal cells, Pan CK + in surface and – in stromal cells | Surgical excision, No nodal invasion |
| So Youn Shin et al., [6] | 19/M, suspected active TB on chest X ray and CT showing clustered lung nodules | TTF-1, EMA positive, HMB 45 negative, Ki-67 low proliferative index | Surgical excision, no nodal metastasis, no recurrence on follow up |
| Jung Hwan Lim et al., [7] | 36/F, solitary lung nodule, increased uptake in18FDG PET, SUVmax-3.9 | TTF-1, EMA, CK-7 were positive, ER, Synaptophysin, CD 56 were negative | Surgical excision, no recurrence on follow up |
| Fayers RW and Lim TS [8] | 45/M, left hilar mass with intense FDG avidity | TTF-1,CK-7,EMA, CK AE1/AE3 were positive,CD56, Synapto, chromo,S100, HMB-45 were negative | Radical external beam radiation therapy as the lesion was not resectable, no recurrence on follow up |
| Baysak Aand Oz AT [9] | 67/F, lesion in right paracardiac area | TTF-1,EMA, AE1/AE3 were positive,CD1a, S100 were negative | Surgical excision, no recurrence on follow up |
| Present case | 7/F, with anterior mediastinal mass on radiology | TTF-1, EMA positive in lesion, vimentin, SMA positive in stromal cellsER,PR,HMB 45 negative, Low Ki-67 index | Surgical excision, no nodal metastasis, no recurrence on follow up |
The pathogenesis of PSP has not been clearly established. The morphology of peripheral cuboidal cells looks similar to type II pneumocytes. IHC positivity for TTF-1 and EMA also indicates the epithelial origin of this tumour. Studies concluded that, PSP may be derived from primitive undifferentiated respiratory epithelium [2]. These lesions are considered benign but a majority of pneumocytomas show a false positivity (increased uptake) in 18-Fludeoxyglucose (18FDG) Positron Emission Tomography (PET). The Standardized Uptake Values (SUV) has a significant correlation with the tumour size [10].
PSP are benign lesions and the main modality of treatment is surgical resection which is considered curative. Metastasis in adjacent lymphnodes [11,12] and recurrence after resection [13] have been reported even though the tumour is benign. The prognosis after surgical resection is generally good, even in the presence of lymph node metastasis, multiple lesions or recurrences.
The child is asymptomatic with follow up for a period of one year. There is mild mediastinal shift to right, however the left lung appears unremarkable.
Conclusion
The case is presented for its radiological confusion with a malignant condition. This emphasizes the significance of histopathological evaluation of the lesion, which ruled out malignancy. The benign nature of the lesion and surgical resection being completely curative is assuring for the patient and the treating physician. The light microscopic finding supported by IHC goes a long way in alleviating the anxiety of the patient.
[1]. Liebow AA, Hubbell DS, Sclerosing haemangioma (histiocytoma, xanthoma) of the lungCancer 1956 9:53-75. [Google Scholar]
[2]. Devouassoux-Shisheboran M, Hayashi T, Linnoila RI, Koss MN, Travis WD, A clinicopathologic study of 100 cases of pulmonary sclerosing haemangioma with immunohistochemical studiesAm J Surg Pathol 2000 24:906-16. [Google Scholar]
[3]. Lei Y, Yong D, Jun-Zhong R, Zhi Y, Zi-Tong W, Treatment of 28 patients with sclerosing haemangioma of the lungJ Cardiothorac Surg 2012 7:3 [Google Scholar]
[4]. Park JS, Kim K, Shin S, Shim H, Kim HK, Surgery for pulmonary sclerosing Haemangioma: lobectomy versus limited resectionKorean J Thorac Cardiovasc Surg 2011 44:39-43. [Google Scholar]
[5]. Ouafi L, Longchampt E, Sage E, Daniel C, Pulmonary sclerosing pneumocytoma: case report and review of the literatureJ Clin Case Rep 2015 (6):544 [Google Scholar]
[6]. Shin SY, Kim MY, Clustered pulmonary sclerosing pneumocytoma in a young man a case reportJ Clinical Imaging 2014 38(4):532-35. [Google Scholar]
[7]. Lim JH, Lee N, Pulmonary sclerosing pneumocytoma mimicking lung cancer, case report and review of literatureThoracic Cancer 2016 7(4):508-11. [Google Scholar]
[8]. Fayers RW, Lim TS, Pulmonary sclerosing pneumocytoma (sclerosing haemangioma): Radical radiation therapyJournal of medical imaging and radiation oncology 2016 60(5):693-95. [Google Scholar]
[9]. Baysak A, Oz AT, A rare tumor of the lung: Pulmonary sclerosing haemangioma (pneumocytoma)Respiratory Medicine 2013 107(3):448-50. [Google Scholar]
[10]. Lee E, Park CM, Kang KW, Goo JM, Kim MA, 18F-FDG PET/CT features of pulmonary sclerosing haemangiomaActa Radiol 2013 54:24-29. [Google Scholar]
[11]. Chien NC, Lin CW, Tzeng JE, Sclerosing haemangioma with lymph metastasisRespirology 2009 14:614-16. [Google Scholar]
[12]. Jungraithmayr W, Eggeling S, Kudwig C, Kayser G, Passlick B, Sclerosing haemangioma of the lung: a benign tumour with potential for malignancy?Ann Thorac Cardiovasc Surg 2006 12:352-54. [Google Scholar]
[13]. Wei S, Tian J, Song X, Chen Y, Recurrence of pulmonary sclerosing haemangiomaThorac Cardiovasc Surg 2008 56:120-22. [Google Scholar]