Fracture of the distal end of radius represents the most common fractures of the upper extremity accounting for 16-20% of all fractures treated by orthopaedic surgeons world-wide [1,2]. Due to increased rate of complications such as malunion, subluxation/dislocation of distal radio-ulnar joint or late collapse of fracture with procedures such as closed reduction and cast immobilization, ligamentotaxis with external fixator and percutaneous pin fixation are no longer acceptable. Furthermore, these procedures often result in poor functional and cosmetic outcome [3,4]. The residual deformity of wrist adversely affects the hand function causing pain, limitation of supination and pronation, and decreased grip strength as a result of radio-carpal and distal radio-ulnar joint arthritis [5,6].
Hence, anatomical articular reduction and stable fixation with or without bone grafting, greatly reduces the incidence of post-traumatic osteoarthrosis and stiffness. The accuracy of fracture reduction co-relates directly to the final outcome [7–9]. The advantages of plate osteosynthesis are direct fracture reduction, stable rigid fixation, the possibility of immediate post-operative mobilization and early return to function [10–12]. With the advent of Locking Compression Plate (LCP), the bone fragments can be held together in place even after union to prevent secondary displacement of unstable fractures, especially in elderly osteoporotic bone [13–15].
Hence, this study evaluated the functional and radiological outcome of internal fixation with volar plate osteosynthesis in the management of unstable fractures of distal end radius.
Materials and Methods
We reviewed 53 patients from January 2011 to December 2015, treated for unstable distal radius fractures using a volar locking compression plate in our institution who fulfilled the inclusion criteria. The institutional ethics committee approval for the study was granted (IEC: RC/14/43).
Instability was established using the Lafontaine’s criteria for unstable fractures of the distal end of radius [16]. He suggested 5 factors that indicated instability. They were initial dorsal angulation greater than 20 degrees, dorsal comminution, radio carpal intra-articular involvement, associated ulna fractures, and age greater than 60 years.
Inclusion criteria: According to Lafontaine et al., fractures presenting with three or more of these factors correlated with loss of position despite cast immobilization and were thus considered unstable. Exclusion criteria included any fracture older than 2 weeks, distal radius fractures extending to shaft of radius, concomitant fractures of ipsilateral limb, open fractures, patients with less than 1 year of follow-up and any previous fractures around the wrist.
After obtaining an informed written consent, patients fulfilling the inclusion criteria were taken up for open reduction and internal fixation with plate osteosynthesis. Out of the 53 patients, 30 of them underwent general anaesthesia and rest 23 underwent ultrasound guided brachial plexus block. Tourniquet was used in all the cases. Through anterior Henry’s approach /Ellis approach, the fracture was approached. The pronator quadratus was detached sub-periosteally from the lateral border of radius. The distal part of the incision was curved laterally to gain better access to the articular surface. Anatomic reduction was achieved using manual ligamentotaxis or dis-impacting the fracture fragments using osteotome. A volar 3.5 mm locking titanium plate (Sharma surgicals, India) was used. The reduction and screw placement were checked under image intensifier. Additional stabilization, if found necessary, was done either with k-wires or with 4 mm cancellous screws. At the end of the procedure, the detached end of the pronator quadratus was reattached to the edge of brachioradialis to provide coverage for the distal plate. Carpal tunnel was not
decompressed in any of our cases. Bone grafting was done for severely comminuted and osteoporotic fractures. Distal Radio-Ulnar Joint (DRUJ) instability was assessed in all cases intraoperatively after the fixation of the distal radius by ballotment test, with the forearm in a neutral position. DRUJ instability was suspected if there was a soft endpoint with an increase in the antero-posterior translation of 5–10 mm as compared to the uninjured wrist [17]. In such cases, DRUJ was temporarily transfixed with radio-ulnar K-wire for a period of 4 weeks and the wire was removed in the out-patient department. All the patients were operated via the same approach as described above by a single team of surgeons comprising of a senior professor, an associate professor and 2 assistant professors.
Post-operatively, radiographs were taken to evaluate the reduction and fixation. Wrist was immobilized in a short below elbow plaster splint till suture removal. During this period, patients were instructed to do active and passive finger motion exercises. After splint removal patients were started on wrist and finger range of motion exercises. For those with DRUJ fixation, forearm rotation was restricted for a total of four weeks post-operatively. Most patients were given a home physiotherapy program but patients who were 65 years and above were advised twice a week visit to physiotherapy department for supervised mobilization. Strenuous use of the hand including heavy weight lifting was not allowed for 12 weeks after surgery. All patients were followed up at 1month, 3 months, 6 months and at the end of 1 year post-operatively. At the time of follow-up, antero-posterior and lateral view radiographs of both wrists were taken on a single exposure for analysis. Radiological outcome was assessed as per Sarmiento’s modification of Lindstorm criteria [18] and functional outcome using the modified Mayo wrist scoring system [19].
Results
Out of the 53 patients with unstable distal end radius fracture, 42 were males and 11 females with an average age of 39.12±31.78 years (18–71 years). Road traffic accident was the most common mode of injury accounting for 35 of the distal radius fractures. Rest 18 of them sustained a fall resulting in distal radius fracture. Thirty of the 53 patients were right hand dominant [Table/Fig-1]. All patients were followed up for a minimum duration of 12 months (range: 12-32 months). All fractures were classified according to AO/OTA classification. There were 9 23-A3 fractures, 11 23-B2 fractures, 15 23-B3 fractures, 10 23-C2 fractures and 8 23-C3 fractures. 11 patients had associated ulnar styloid fracture (1 23-B2, 2 23-B3, 3 23-C2 and 5 23-C3). None of them underwent ulnar styloid fixation. DRUJ instability was diagnosed in seven (13.20%; 2 23-A3,1 23-B2,1 23-B3, 1 23-C2 and 2 23-C3) patients intraoperatively. They underwent additional radio-ulnar k-wire fixation. The radiological parameters such as palmar tilt, radial height, radial inclination and ulnar variance of the affected wrist and normal side were tabulated preoperatively and post-operatively at each visit.
Clinical profile of patients.
| Mean age at presentation | 39.12±31.78 years (18–71 years) |
| Sex | Male - 42Female - 11 |
| Mode of injury | Road Traffic Accident - 35Fall - 18 |
| Type of fracture | A3 - 09B2- 11B3- 15C2- 10C3- 08 |
| Hand dominance | Right- 30Left-23 |
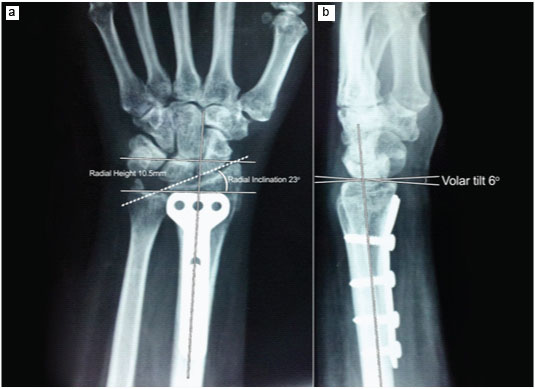
In addition to plating, 5 patients underwent additional k-wiring for radial styloid fixation. K-wire was removed in the Outpatient Department (OPD) after radiological fracture union. Primary bone grafting was done in 5 cases (1 23-B3, 2 23-C2 and 2 23-C3). Out of the 53 cases, 51 of them united radiologically with a mean duration of 3.34 months (range: 2.5-4.2 months). In 2 cases, there was a delay in union. X-ray images showed sub-articular and metaphyseal defect for which bone grafting was done. Both the fractures eventually united at 15 and 18 weeks, respectively. The average postoperative radial inclination, radial height, palmar tilt and ulnar variance, calculated at 7 to 12 weeks was found to be was found to be 21.03±4.25 degrees, 10.11±1.64mm, 9.64±5.94 degrees and −0.27±0.67 mm respectively. At the end of 1 year of follow-up, the average radial inclination, radial height, palmar tilt and ulnar variance changed to 20.94±4.44 degrees, 10.03±1.20 mm, 9.51±5.23 degrees and −0.15±1.99 mm respectively [Table/Fig-2,3]. No significant difference (p<0.001) in the radiological parameters were noted at the end of 1 year follow-up, indicating no further significant collapse of fracture [Table/Fig-4].
Radiographic analysis of a 35-year-old male patient with AO 23-B2 distal radius fracture at the end of 1 year: (a) Radial inclination of 23 degrees and radial height of 10.5 mm on Antero-posterior view; (b) Palmar tilt of 6 degrees on lateral view radiograph.
| Parameters | Postoperatively(7–12 weeks) | At 1 year follow-up |
|---|
| Radial inclination | 21.03±4.25 degrees | 20.94±4.44 degrees |
| Radial Height | 10.11±1.64mm | 10.03±1.20 mm |
| Palmar tilt | 9.64±5.94 degrees | 9.51±5.23 degrees |
| Ulnar variance | −0.27±0.67 mm | −0.15±1.99 mm |
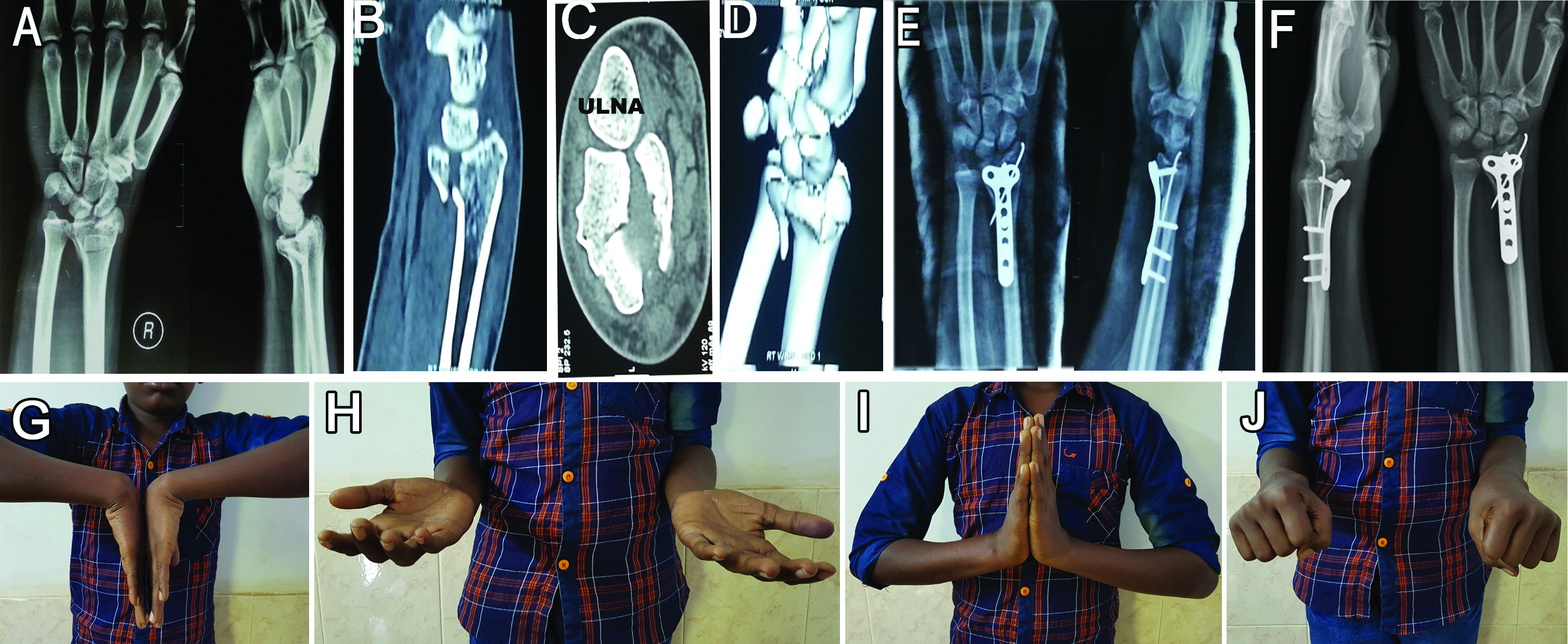
Preoperative radiographs: (a) of 19-year-old boy with AO 23-C3 distal radius fracture. CT scan; (b-d) showing the intra-articular comminution; (e) Immediate postoperative radiographs showing good reduction of fragments; (f) Radiographs at the end of 1 year showing no further collapse of fracture and restored radiological parameters; (g-j) showing excellent functional outcome.
The average wrist range of motion at the end of 1 year of follow-up was 61.13±12.88 degrees flexion (range 35 to 85 degrees) and 50.66±18.43 degrees extension (range 35 to 90 degrees). The average forearm range of motion was 77.43±11.40 degrees supination (range 50 to 90 degrees) and 84.37±5.35 degrees pronation (range 70 to 90 degrees) at 1 year of follow-up. Hand grip strength (compared to opposite side), as assessed by a hand held dynamometer improved from 55.45±21.55% (range 40 to 90%) at 6 weeks follow-up to 89.00±4.55%(range 75 to 100) at 1 year follow-up, respectively [Table/Fig-5,6].
Functional evaluation of patients at the end of 6 weeks post-op and 1 year follow-up.
| Parameters | 6 weeks post-op | 1 year follow-up |
|---|
| Flexion | 40.14±14.11 degrees | 61.13±12.88 degrees |
| Extension | 29.12±7.44 degrees | 50.66±18.43 degrees |
| Supination | 54.95±10.01 degrees | 77.43±11.40 degrees |
| Pronation | 74.15±8.14 degrees | 84.37±5.35 degrees |
| Grip strength (compared to opposite side) | 55.45±21.55% | 89.00±4.55% |
Preoperative radiographs: (a) of 34-year-old lady with AO 23-B2 distal radius fracture. (b) Immediate postoperative radiographs showing good reduction of fragments with plate in-situ; (c) Radiographs at the end of 15 months showing no further collapse of fracture and restored radiological parameters; (d-h) showing excellent functional outcome.

At the end of 1 year follow-up, 11(20.75%) patients had excellent outcome, 26(49.06%) had good outcome, 10 (18.87%) patients had satisfactory outcome and 6(11.32%) patients had poor outcome as per the modified Mayo wrist scoring system [Table/Fig-7]. These 6 patients (1 23-B3, 1 23-C2 and 4 23-C3) had poor functional outcome owing to their complications and non-compliance to postoperative rehabilitation. Overall, 8 patients had complications [Table/Fig-8]. There were no cases of tendon ruptures or non-union in our study.
Functional and radiological outcome of unstable distal radius fractures.
| Scoring System | 1 year Follow-up |
|---|
| Modified Mayo wrist scoring system | Excellent- 11 (20.75%)Good- 26 (49.06%)Satisfactory- 10 (18.87%)Poor- 06 (11.32%) |
| Sarmiento’s modification of Lindstorm criteria | Excellent- 36 (67.92%)Good- 10 (18.87%)Fair- 07 (13.21%)Poor- 0 |
Complications with their functional outcome.
| Complication | Numberof cases | Intervention | Functional outcome(At 1 year follow-up) |
|---|
| 1. Screw penetration into the joint due to excessive of collapse in spite of primary bone grafting | 1 | Implant exit was done after fracture union at 3 months follow-up. | Fair |
| 2. Significant prominence of screws noted on the postoperative x-rays.(more than 2 threads protruding out of the dorsal cortex). | 4 | Two patients had pain on palmar flexion of the wrist. They underwent implant removal at 6th month and 8th month respectively. Rest two were asymptomatic. No further intervention was done. | Excellent-2 patientsGood-2 patients |
| 3. Superficial wound infection | 1 | Intravenous antibiotics for 10 days. Infection subsided. | Excellent |
| 4. Persistent pain with decreased range of motion at the wrist. | 2 | Implant exit was done after fracture union at 6 months and 9 months respectively. VAS improved from 7 to 1 in one case and in the other case remained at 5 even after implant exit. X-ray of this patient showed reduction of radio-carpal joint space, erosions and juxta-articular cysts suggestive of radio-carpal arthritis. She opted no further treatment. | Satisfactory-1 patientPoor-1 patient |
On radiological scoring by Sarmiento’s modification of Lindstorm criteria, 36(67.92%) patients had excellent results, 10(18.87%) patients had good results and 7(13.21%) patients had fair results. Fair results were attributed to poor reduction and alignment of fracture fragments.
Discussion
An anatomical reduction of the articular surface with a stable fixation is the main goal in the treatment of intra-articular distal radius fractures. Improper reduction or residual intra-articular incongruity leads to secondary arthritis and poor functional outcome in the long term [5,6]. Various treatment modalities have been described for distal radius fracture fixation. Treatment options range from closed reduction and cast application to open reduction with plates and screws. Plating allows direct visualization of fracture fragments and restoration of the anatomy, decreased morbidity by allowing early mobilization, and early return of wrist function. Locking plates address intra-articular and metaphyseal comminution and are very helpful in osteoporotic fractures preventing late collapse of fracture fragments. Biomechanical studies comparing volar fixed-angle locking plates with that of conventional dorsal plates report volar fixed-angled plates to be superior in terms of their strength. Dorsal plating of distal radius has not gained popularity due the fact that, inspite of dorsal plating, the volar collapse of fracture occurred [20]. Complications associated with plating include risk of infection as compared to closed procedures, tendon irritation or rupture. These may warrant implant removal in some cases.
DRUJ instability was previously recognized as a poor prognostic factor in the management of distal radius fractures. However, studies suggest that anatomically reduced and rigidly fixed distal radius fractures with locking plates have no significant difference in the final functional outcome between patients treated with and without ulnar styloid fractures, despite the degree of displacement and the location of the fractures [21]. In our study, seven (13.20%; 2 23-A3,1 23-B2,1 23-B3, 1 23-C2 and 2 23-C3) patients, diagnosed to have DRUJ instability intraoperatively underwent additional radio-ulnar K-wire fixation. The K-wire was removed in the Out-Patient Department after 4 weeks. These patients had reduced pronation at 6 weeks of follow-up but there was no difference compared to the non-fixed group at the end of 3 months. DRUJ fixation had no negative impact on the outcome of the study at the end of 1 year follow-up.
Studies have been done to demonstrate the advantages of fixation of ulnar styloid fractures along with distal radius fractures, but not many have been successful. The results have been variable [21]. In a study done by Zenke Y et al., the good functional outcome of distal radius fractures did not depend on the fixation of ulnar styloid [22]. They concluded that most of the ulnar styloid fractures healed with fibrous union and remained asymptomatic. Jae Kwang Kim et al., studied ulnar styloid fractures in seventy-six (55%) of the 138 patients and they concluded that an accompanying ulnar styloid fracture in patients with stable fixation of a distal radial fracture has no apparent adverse effect on wrist function or stability of the distal radioulnar joint [23].
In our study, the dominant side, when injured recovered early, with grip strength 95% of the contra lateral side at 6 months follow-up and remained the same at 1 year of follow-up. Grip strength of the non-dominant injured side only reached 82% of the normal side even at 1year of follow-up. Pronation improved more rapidly than supination at 6 weeks of follow-up but both returned to near normal at the 1 year of assessment. No significant difference (p<0.001) in the radiological parameters were noted at the end of 1 year as compared to 6 weeks of follow-up, indicating that the fracture fixation was rigid and no further significant collapse of the fracture occurred.
At the end of 1 year follow-up, out of the 53, 37(69.81%) patients had excellent to good results, compared to 6(11.32%) patients who had poor outcome as per the modified Mayo wrist scoring system owing to the complications mentioned above. The limitations of our study were lack of controls and non- uniformity of fracture pattern.
Conclusion
We conclude that, non-fixation of ulnar styloid fracture did not have a negative impact on the outcome of the study. DRUJ stabilization for instability with K-wire for 4 weeks resulted in favourable outcome. For unstable fractures of the distal end of radius, volar locking plate osteosynthesis is a valid and effective treatment option ensuring a successful functional and radiological outcome.
Conflict of Interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Consent
Written informed consent was obtained from all the patients for publication of this report and accompanying images. This study has the approval of the institutional ethics committee.