Introduction
Diabetes Mellitus (DM) is always a multifactorial metabolic disorder having a wide range of abnormalities in carbohydrate, lipid and protein metabolism. Dyslipidemia is a natural process of DM causing abnormal variations of different lipoproteins and it is one of the significant risk factors for Cardiovascular Disorder (CVD). There is a need to closely evaluate newer approaches in case of DM because even if dyslipidemia is treated, there is always a risk of CVDs in DM patients because of the hyperglycemia itself. So, lipid abnormalities should be assessed aggressively and treated as part of diabetes care. Apolipoprotein B100 (Apo B100), Apolipoprotein A1 (Apo A1) and Lipoprotein (a) {Lp(a)} are newer markers which are always welcome and necessary as many of the reported cases with normal conventional lipid profile have developed cardiac events.
Aim
Study the correlation between glycemic control and the levels of Apo A1, Apo B100 and Lp(a).
Materials and Methods
Total 56 patients of (DM) diagnosed on the basis of American Diabetic Association guidelines were recruited, out of which 28 were identified as uncontrolled-diabetic patients and remaining 28 as controlled-diabetics on the basis of Glycosylated HbA1c (HbA1c). The control group consisted of normal healthy 28 individuals. Apo B100, Apo A1 and Lp(a) along with traditional lipid profile, Fasting Blood Sugar (FBS) and HbA1c were estimated in all the subjects.
Results
Apo B100/Apo A1 ratio and Lp(a) levels showed highly significant difference (p-value <0.001) between uncontrolled diabetics, controlled diabetics and healthy Controls. Apo B100/Apo A1 ratio and Lp(a) showed significant positive correlations with HbA1c (r= 0.494, p <0.0001) and with each other.
Conclusion
Apo B100/Apo A1 ratio and Lp(a) show a highly significant positive relationship with glucose tolerance of the patients as reflected in the HbA1c values. If proper glycemic control is maintained, the levels of Apo B100/Apo A1 ratio and Lp(a) can be controlled as reflected by the lower levels of these parameters observed in controlled diabetics in comparison to uncontrolled diabetics.
Introduction
In this 21st century, we are facing a major shift in the disease pattern. Non Communicable Diseases (NCD) are now a massive challenge for the medical science. Mortality and morbidity rates are very high in case of NCD. It is now undisputed truth that there is a strong relation between DM and CVDs [1]. The metabolic risk factors for CVDs mainly include dyslipidemia, hypertension, obesity and DM [2]. Most of the CVDs are having chronic pathological process, we know many risk factors causing and even indicating future events of CVDs [3]. The need of the newer approach was necessary as many of the reported cases who had already achieved recommended levels of conventional lipid profile have developed cardiac events mainly in high risk patients [4]. These newer markers answer many of the questions by providing their wide range of specificity over traditional markers [4,5]. DM is always a very complicated metabolic disorder having wide range of abnormalities in carbohydrate, lipid and protein metabolism. Dyslipidemia is a natural process of DM causing abnormal increase of various lipoproteins. We have already discussed that dyslipidemia is one of the significant risk factor for CVDs. As a result there is a need to closely evaluate newer approach in case of DM because even if dyslipidemia is treated, there is always a risk of CVDs in DM patients. The reason is hyperglycemia itself, so lipid abnormalities should be assessed aggressively and treated as part of comprehensive diabetes care [6]. Apolipoprotein B100 (Apo B100) is the protein part of Low Density Lipoprotein (LDL), Very Low Density Lipoprotein (VLDL) and Intermediate Density Lipoprotein (IDL). Apolipoprotein A1 (Apo A1) is the protein part of High Density Lipoprotein (HDL). The hyperglycemia in DM causes formation of Advanced Glycation End products (AGEs), glycated proteins are one of the AGEs. These AGEs cause formation of pro-inflammatory products by stimulating various receptors on various cells related to formation of atherosclerosis. Apo B100 undergoes this glycosylation process and plays a vital role in formation of plaque. The process is not limited to LDL alone; it affects all the lipoproteins having Apo B100 as apolipoprotein [7]. So, it is logical to evaluate the Apo B100 in case of DM, Apo A1 being part of HDL will give fair share to check the balance between the levels of “Good Cholesterol” and “Bad Cholesterol”. Lp(a) is another reported novel marker which may have independent capacity to be a superior marker than conventional markers [8,9]. It’s basically LDL with additional apolipoprotein which is apolipoprotein(a). It has structural similarity with plasminogen and so, it inhibits the activation of plasminogen to plasmin competitively which leads to inhibition of fibrin clot lysis [10]. As we are given to understand, there may be a superiority of the apoproteins and Lipoprotein(a) {Lp(a)} over the traditional markers, there is a need to evaluate these in conditions like DM independently. In our study, we have evaluated the levels of Apo B100, Apo A1 and Lp(a) along with traditional lipid profile, FBS and HbA1c to study the relation between severity of DM and the risk markers of CVDs. Various prospective studies have claimed the relationship between the DM and levels of risk factors [11,12], but some studies couldn’t find significant relationship and reported inconsistency between DM and risk markers of CVDs [13,14]. We hope that our study conducted in different demography will give some insights regarding the prediction of the future complications by using Apo B100, Apo A1 and Lp(a) as markers so that the patients can avoid the fatal complications of DM.
Materials and Methods
The present case control study was conducted between January-2015 to September-2015 in the Department of Biochemistry, Shree Krishna Hospital, Karamsad, Anand. Total 84 subjects were recruited, 56 patients were recruited from health checkup scheme of the hospital and from the outpatient clinic of Department of Medicine and 28 healthy controls were recruited from health checkup scheme of the hospital.
A total of 56 cases of type 2 diabetes mellitus determined by Fasting Plasma Glucose >125mg/dL were included in the study. Controlled and uncontrolled diabetic patients were differentiated on the basis of HbA1C. A total number 28 of cases with HbA1C >8 % were considered as Uncontrolled Diabetics (UCD) and 28 cases with HbA1C <8 % served as Controlled Diabetics (CD) [15]. Similarly a total number of 28 served as healthy non diabetic participants, determined by Fasting Plasma Glucose <110mg/dL. We considered Apo B100/Apo A1 ratio as most important variable. Previous data of 50 healthy people (not included in the study) had a mean of 0.75 with a SD of 0.47. Assuming a difference of 0.2 in this ratio as clinically important and there is intermediate dispersion amongst means, we required a sample of size 28 per group [16]. Subjects taking lipid lowering agents were excluded from the present study. Subjects having liver disease, kidney disease were excluded from the present study.
Fasting blood samples were taken in plain vacutainer containing no anticoagulant, sodium fluoride vacutainer and potassium Ethylenediaminetetraacetic acid (EDTA) vacutainer with an aseptic blood collection technique by use of sterile gloves and thorough disinfection of vene-puncture site, through 70% ethyl alcohol. All the samples were collected in sitting position. Samples were centrifuged within one hour at 3000 rpm for 10 minutes. These would be processed to obtain serum/plasma for the estimation of serum lipid profile, fasting plasma glucose level and HbA1c. Estimation of fasting lipid profile (Triglyceride, Total Cholesterol, and HDL), fasting plasma glucose and HbA1c were carried out on fully automated COBAS INTEGRA 400 PLUS clinical chemistry analyser. Serum Total Cholesterol(TC) was analysed by Colorimetric assay with Cholesterol Oxidase- Peroxidase (CHOD-POD) [17], triglyceride was analysed by Colorimetric end-point Glycerol Phosphate Oxidase, phenol + aminophenazone (GPO-PAP) [18], serum HDL was analysed by homogenous enzymatic colorimetric [19,20], serum LDL, VLDL were calculated by using Friedewald formula [21], plasma glucose was analysed by using enzymatic hexokinase method [22] and HbA1c was analysed by using immunoturbidimetry method [23]. The serum samples were diluted and Apolipoprotein B, Apolipoprotein A-1 and Lp(a) estimation were carried out on Tulip Quantimate turbidimetry and chemistry analyser by using immunoturbidimetry method [24,25].
Ethical clearance was obtained by institution’s Human Research Ethics Committee. A study protocol was set before undertaking this study and it was approved by institutional Human Research Ethical Committee. All the participants in the study were explained clearly about the purpose and the nature of the study in the language best understood by them. Their samples were included only after obtaining a written and informed consent.
Statistical Analysis
Means and standard errors of all three groups for various parameters were calculated. Differences between means were tested by one-way Analysis Of Variance (ANOVA). Pearson’s Correlation Coefficient was used for correlation analysis. The p-value <0.05 was considered as statistically significant. Analysis was performed using SPSS (22.0 version), Microsoft office excel 2016 and MedCalc version 12.5.
Results
Out of total 56 cases, 32 subjects were males and 24 subjects were females, and out of 28 cases, 14 were males and 14 subjects were females [Table/Fig-1]. The mean age of case group was 53.68±10.95 years and in the control group, mean age was 52.46±12.12 years [Table/Fig-2]. This showed that there was no significant difference between these age groups.
Age and gender distribution.
| Age In Years | Cases | Controls |
|---|
| Male | Female | Male | Female |
|---|
| ≤35 | 2 | 1 | 2 | 1 |
| 35-45 | 4 | 2 | 3 | 1 |
| 46-55 | 11 | 14 | 3 | 3 |
| 56-65 | 12 | 4 | 4 | 8 |
| 66-80 | 3 | 3 | 2 | 1 |
| Total | 56 | 28 |
Mean comparison of various parameters in Cases and Controls.
| Parameter | Groups | Mean | Std. Deviation | Std. Error Mean | 95% Confidence Interval of the Difference |
|---|
| Lower | Upper |
|---|
| AGE (Years) | UCD | 53.68 | 11.16 | 2.11 | 49.35 | 58.01 |
| CD | 53.68 | 10.94 | 2.07 | 49.44 | 57.92 |
| Controls | 52.46 | 12.12 | 2.29 | 47.77 | 57.16 |
| S. Cholesterol (mg/dL) | UCD | 197.36 | 30.74 | 5.81 | 185.44 | 209.28 |
| CD | 191.82 | 37.05 | 7.00 | 177.45 | 206.19 |
| Controls | 180.00 | 28.04 | 5.30 | 169.13 | 190.87 |
| HDL (mg/dL) | UCD | 44.89 | 8.78 | 1.66 | 41.49 | 48.30 |
| CD | 51.07 | 14.47 | 2.73 | 45.46 | 56.68 |
| Controls | 50.29 | 12.42 | 2.35 | 45.47 | 55.10 |
| LDL (mg/dL) | UCD | 126.73 | 27.12 | 5.12 | 116.21 | 137.24 |
| CD | 112.01 | 27.98 | 5.29 | 101.17 | 122.86 |
| Controls | 109.45 | 25.78 | 4.87 | 99.45 | 119.45 |
| TC/HDL | UCD | 4.6 | 1.1 | 0.2 | 4.1 | 5.0 |
| CD | 4.0 | 1.2 | 0.2 | 3.5 | 4.4 |
| Controls | 3.7 | 0.9 | 0.2 | 3.4 | 4.1 |
| LDL/HDL | UCD | 3.0 | 0.9 | 0.2 | 2.6 | 3.3 |
| CD | 2.3 | 0.8 | 0.2 | 2.0 | 2.7 |
| Controls | 2.3 | 0.8 | 0.1 | 2.0 | 2.6 |
| Apo A1 (mg/dL) | UCD | 136.50 | 51.55 | 9.74 | 116.51 | 156.49 |
| CD | 173.04 | 48.52 | 9.17 | 154.22 | 191.85 |
| Controls | 189.11 | 46.41 | 8.77 | 171.11 | 207.10 |
| Apo B100 (mg/dL) | UCD | 186.68 | 35.71 | 6.75 | 172.83 | 200.52 |
| CD | 171.71 | 55.94 | 10.57 | 150.02 | 193.41 |
| Controls | 147.25 | 44.09 | 8.33 | 130.16 | 164.34 |
| Apo B100/Apo A1 | UCD | 1.6 | 0.8 | 0.1 | 1.3 | 1.9 |
| CD | 1.0 | 0.4 | 0.1 | 0.9 | 1.2 |
| Controls | 0.8 | 0.3 | 0.1 | 0.7 | 0.9 |
| Lp(a) (mg/dL) | UCD | 42.61 | 20.80 | 3.93 | 34.54 | 50.67 |
| CD | 22.00 | 16.85 | 3.19 | 15.46 | 28.54 |
| Controls | 15.68 | 7.77 | 1.47 | 12.67 | 18.69 |
Means of TC, LDL, TC/HDL ratio, LDL/HDL ratio, Apo B100, Lp(a) and Apo B100/Apo A1 ratio were higher in UCD and CD than the control group and remarkably higher in UCD than both CD and the control group. Means of Apo A1 were lower in UCD and CD than the control group [Table/Fig-2].
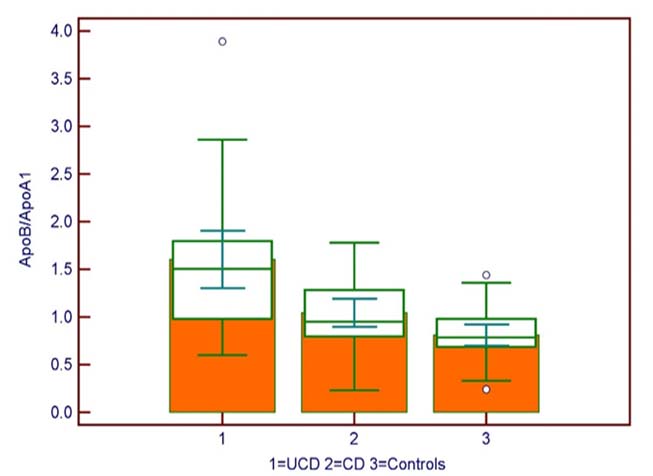
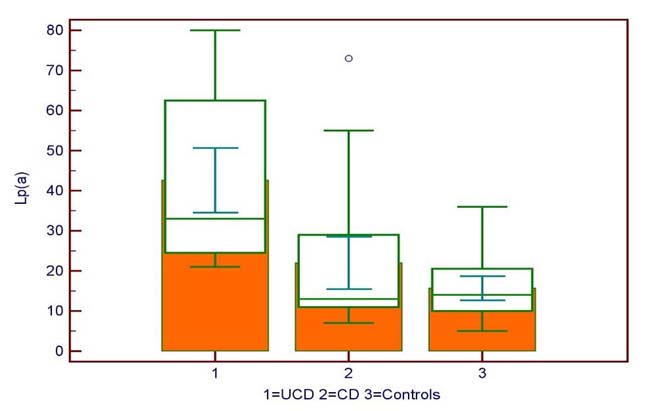
The one-way ANOVA analysis of various parameters showed highly significant difference between UCD, CD and controls in case of Apo B100/Apo A1 ratio and Lp(a) levels (p-value <0.001). There was also significant difference between Apo B100 (p-value= 0.007), Apo A1 (p-value <0.0001), TC/HDL ratio (p-value 0.015) and LDL/HDL ratio (p-value= 0.005) between UCD, CD, and the controls [Table/Fig-3,4 and 5].
One-way-ANOVA of various parameters in UCD, CD and Controls.
| Sum of Squares | DF | Mean Square | F | Sig. (p- value) |
|---|
| Apo A1 | Between Groups | 40699.500 | 2 | 20349.750 | 8.520 | <0.001** |
| Within Groups | 193468.643 | 81 | 2388.502 | |
| Total | 234168.143 | 83 | |
| Apo B100 | Between Groups | 22185.738 | 2 | 11092.869 | 5.243 | 0.007** |
| Within Groups | 171389.071 | 81 | 2115.914 | |
| Total | 193574.810 | 83 | |
| Apo B100/ Apo A1 | Between Groups | 9.296 | 2 | 4.648 | 16.765 | < 0.001** |
| Within Groups | 22.456 | 81 | 0.277 | |
| Total | 31.752 | 83 | |
| Lp(a) | Between Groups | 11104.452 | 2 | 5552.226 | 21.437 | < 0.001** |
| Within Groups | 20978.786 | 81 | 258.997 | |
| Total | 32083.238 | 83 | |
*significant at p-value <0.05 level.
**highly significant at p-value <0.01 level.
One-way-ANOVA of Apo B100/Apo A1 ratio.
The bivariate correlation analysis of Apo B100/Apo A1 ratio and Lp(a) with various parameters was done by using pearson’s correlation coefficient. Apo B100/Apo A1 ratio showed significant positive correlations between HbA1C, FBS, Lp(a), Apo B100, TC/HDL ratio, LDL/HDL ratio and LDL. Apo B100/Apo A1 ratio showed significant negative correlations between HDL and Apo A1. Lp(a) showed significant positive correlation between HbA1C, Apo B100/Apo A1 ratio, TC/HDL ratio, LDL/HDL ratio. Lp(a) showed significant negative correlations between HDL and Apo A1. Lp(a) showed no correlation with the levels of Apo B100 and marginal correlation with LDL [Table/Fig-6].
Pearson’s correlation coefficient of cases and controls.
| N | Apo B100/Apo A184 | Lp(a)84 |
|---|
| HbA1c | (r) Pearson Correlation | 0.494 | 0.514 |
| Sig. (p-value) | 0.000** | 0.000** |
| LDL | (r) Pearson Correlation | 0.391 | 0.217 |
| Sig. (p-value) | 0.000** | 0.048* |
| HDL | (r) Pearson Correlation | -0.368 | -0.262 |
| Sig. (p-value) | 0.001** | 0.016* |
| TC/HDL | (r) Pearson Correlation | 0.482 | 0.357 |
| Sig. (p-value) | 0.000** | 0.001** |
| LDL/HDL | (r) Pearson Correlation | 0.525 | 0.336 |
| Sig. (p-value) | 0.000** | 0.002** |
| ApoB100 | (r) Pearson Correlation | 0.596 | 0.13234 |
| Sig. (p-value) | 0.000** | 0.230 |
| ApoA1 | (r) Pearson Correlation | -0.705 | -0.452 |
| Sig. (p-value) | 0.000** | 0.000** |
| Apo B100/Apo A1 | (r) Pearson Correlation | 1 | 0.520 |
| Sig. (p-value) | | 0.000** |
| Lp(a) | (r) Pearson Correlation | 0.520 | 1 |
| Sig. (p-value) | 0.000** | |
*. Correlation is significant at the p-value <0.05 level. **. Correlation is highly significant at the p-value <0.01 level.
Discussion
In our study, we have chosen total 84 subjects, based on their age and sex involving 56 subjects having DM type 2 by using standard guidelines from the American Diabetes Association (ADA) [15]. The cases were divided further on the basis of HbA1C as controlled and uncontrolled according to ADA guidelines [15].
This study didn’t evaluate the outcome of CVD; many large prospective studies like Apolipoprotein-related MOrtality RISk (AMORIS) have proposed the relation between Apolipoproteins and risk of CVDs in general population [26–28]. The more recent INTERHEART studies have included 15,152 patients with a first Myocardial Infarction (MI) compared to 14,820 subjects from 52 countries world-wide matched for age, gender, ethnicity and continent [29,30]. Based on their findings, INTERHEART Modifiable Risk Score (IHMRS) have been developed [31]. The Apolipoprotein ratio independently came top of all for predicting risk of future CVDs, diabetes however on the other hand also defined as an independent risk factor for the same. There was no proper correlation made between the severity of DM and the levels of apolipoproteins in those studies.
In our study, it has been found that the mean of ApoB100, Apo B100/Apo A1 ratio and Lp(a) concentrations were significantly higher in the case group than the controls. The mean of the Apo B100/Apo A1 ratio and Lp(a) were comparatively very high in UCD than the CD and healthy controls. As various parameters in all the groups were compared, significant difference was observed in ApoB100 (p <0.005), Apo B100/Apo A1 (p <0.0001) and in Lp(a) (p-value <0.0001).
Our study had similar results like many other studies reporting increased levels of Apolipoproteins in diabetics. Katulanda G et al., found that patients with type 2 diabetes had atherogenic lipid profiles [32]: elevated ApoB often accompanied by elevated TG, high Apo B100/ Apo A1 ratio and low LDL: Apo B 100 ratio. Sniderman AD et al., found in 249 Canadian subjects that 23% had abnormal LDL [33], i.e., an elevated LDL cholesterol level; almost 40% has an elevated Apo B and therefore an elevated LDL particle number. Albers JJ et al., found that in type 2, 36% had elevated ApoB100, 36% had dense LDL [34], but only 23% had elevated LDL. With regard to Indian and especially Gujarati population, Patel JV et al., found significant higher levels of Apolipoproteins in both migrants Gujarati people in UK and their siblings in Gujarat [35].
Our study was also in line with various studies which have reported that concentration of Lp(a) is significantly higher in diabetic people than the normal individuals. Hernández C et al., found that the Lp(a) concentration was higher in patients who died from CVD (median 15.5mg/dl {range 0.5–75}) than those who remained alive or those who died from non-CVD causes [36]. Shai I et al., interpreted that increased levels of Lp(a) were independently associated with risk of CHD among diabetic women [12]. Hiraga T et al., found that the incidence of CVD was significantly higher among type 2 diabetic patients with a high serum Lp(a) than among those with a low serum Lp(a) level [37]. Mora S et al., found that Lp(a) was associated inversely with risk of type 2 diabetes independent of risk factors, in contrast to our study which shows higher level of Lp(a) in diabetics [13]. Based on same data Qibin Qi et al., have shown that effect of Lp(a) on CVD risk among diabetic patients might be different from that in the general population [14]. Such differences in results demand a further evaluation and larger population data to establish the relationship.
In our study, bivariate correlation analysis of Apo B100/Apo A1 ratio showed significant positive correlations between HbA1c, FBS, Lp(a), ApoB, TC/HDL ratio, LDL/HDL ratio and LDL. Apo B100/Apo A1 ratio showed significant negative correlations between HDL and Apo A1. The Apo B100/Apo A1 ratio was noticed to be elevated with an elevation of HbA1c and FBS, which reflect a worsening of the diabetic state, is supported by AMORIS study [26], which also postulated a positive correlation between CVDs and the above findings. Further, we could also notice an increase of Apo B100, LDL, TC/HDL ratio, LDL/HDL ratio and Lp(a). Albers JJ et al., apart from concluding the increased levels of ApoB100 in diabetics [34], they also correlated that 72% of poorly controlled type 2 diabetics had elevated Apo B100 and 62% had dense LDL with elevated HbA1c. Ródenas S et al., has established positive relationship between levels of HbA1c and plasma apoproteins and plasma lipoproteins in type II diabetic patients and the future development of CVD [38].
Lp(a) showed significant positive correlation between HbA1c, FBS, Apo B100/Apo A1 ratio, TC/HDL ratio, LDL/HDL ratio. Lp(a) showed significant negative correlations between HDL and Apo A1. Agoston-Coldea L et al., found direct correlation between Apo B100/Apo A1 ratio and Lp(a) levels. Lp(a) showed no correlation with the levels of Apo B100 and marginal correlation with LDL [39]. These results are inconsistent with some studies suggesting a slight correlation of Apo B100 and Lp(a). Guyton J et al., suggested correlations between these two parameters and also correlation with LDL which is also true in our study [40], but they also reported that when LDL and VLDL are more constant, as in their study, then the proportion of variance of Apo B100 due to Lp(a) is increased and the correlation becomes evident. But some other studies suggesting totally opposite findings and our results are in line with the studies, Kamboh M et al., who did not find correlation between Apo B100 and Lp(a) in both men and women, they found correlation between LDL and Lp(a) in men but not in women [41]. Albers JJ et al., also reported no correlation between Apo B100 and Lp(a) [34]. Theoretically, Lp(a) has totally independent metabolism than the LDL and Apo B100, although it is basically an LDL with Apo(a) as an extra apoprotein [42]. The regulation of the production of Lp(a) is at genetic level, Lp(a) concentrations highly significantly correlate with its own production rate, yet the Lp(a) catabolism does not control Lp(a) levels [43]. So, its levels cannot be correlated with the Apo B100 levels. We also observed on the basis of mean comparison, ANOVA and correlations with HbA1c that if proper glycemic control is maintained, the levels of Apo B100/Apo A1 ratio and Lp(a) can be controlled as reflected by the lower levels of these parameters observed in CD in comparison to UCD. Our study clearly showed the significant differences between the levels of various risk factors related to CVDs, so, it can be proposed that if diabetic patients maintain their glucose levels, they can avoid the future risk of CVDs to a larger extent [44].
Limitation
As this is a case control study, we were unable to follow up of our subjects to find out the outcome of the disease process and complications.
Conclusion
It can be emphasised that the Apo B100/Apo A1 ratio in diabetics seems to be elevated according to their glycemic control as reflected in the HbA1c values. In our study we also observed that some of the patients (~60%) of diabetes whose Apo B100/Apo A1 was raised, did not have a concomitant increase in the concentration of conventional lipid levels. So, it may be proposed that Apo B100/Apo A1 ratio could serve as a better marker than conventional lipid profile. If proper glycemic control is maintained, diabetic patients can reduce ApoB100/ ApoA1 ratio as reflected by the lower levels observed in CD in comparison to UCD. We also observed that if proper glycemic control is maintained, Lp(a) can also be controlled. So, it can be proposed that if diabetic patients maintain their glucose levels, they can maintain the Apo B100/ Apo A1 and Lp(a) levels and may avoid the future risk of CVDs to a larger extent.
*significant at p-value <0.05 level.
**highly significant at p-value <0.01 level.
*. Correlation is significant at the p-value <0.05 level. **. Correlation is highly significant at the p-value <0.01 level.
[1]. Grundy SM, Benjamin IJ, Burke GL, Chait A, Eckel RH, Howard BV, Diabetes and cardiovascular disease: a statement for health professionals from the American heart associationCirculation 1999 100:1134-46. [Google Scholar]
[2]. Gaziano T, Gaziano J, Epidemiology of cardiovascular disease. In: Dan L. Longo, Dennis L. Kasper, J. Larry JamesonHarrison’s Principles of Internal Medicine 2015 19ENew YorkMcGraw-Hill:266e-4. [Google Scholar]
[3]. Libby P, The Pathogenesis, Prevention, and Treatment of AtherosclerosisIn: Dan L. Longo, Dennis L. Kasper, J. Larry JamesonHarrison’s principles of internal medicine 2015 19ENew YorkMcGraw-Hill:291e-4. [Google Scholar]
[4]. Boyles, S. (2008, March 27). Cholesterol testing not enough for some: WebMD - Better information. Better health. [updated 2008 Mar 27; cited 2015 Nov 5]. Available from http://www.webmd.com/cholesterol-management/news/20080327/cholesterol-testing-not-enough-for-some [Google Scholar]
[5]. Otvos JD, Mora S, Shalaurova I, Greenland P, Mackey RH, Goff DC, Clinical implications of discordance between low-density lipoprotein cholesterol and particle numberJ Clin Lipidol 2011 5:105-13. [Google Scholar]
[6]. Longo DL, Kasper DL, Jameson JL, Harrison’s Principles of internal medicine 2015 19ENew YorkMcGraw-Hill [Google Scholar]
[7]. Rabbani N, Chittari MV, Bodmer CW, Zehnder D, Ceriello A, Thornalley PJ, Increased glycation and oxidative damage to apolipoprotein B100 of LDL cholesterol in patients with type 2 diabetes and effect of metforminDiabetes 2010 59(4):1038-45. [Google Scholar]
[8]. Kamstrup PR, Benn M, Tybjærg-Hansen A, Nordestgaard BG, Extreme lipoprotein(a) levels and risk of myocardial infarction in the general population. The copenhagen city heart study, american heart associationCirculation 2008 117:176-84. [Google Scholar]
[9]. Von Eckardstein A, Schulte H, Cullen P, Assmann G, Lipoprotein(a) further increases the risk of coronary events in men with high global cardiovascular riskJ Am Coll Cardiol 2001 37:434-39. [Google Scholar]
[10]. Rouy D, Grailhe P, Nigon F, Chapman J, Angles-Cano E, Lipoprotein(a) impairs generation of plasmin by fibrin-bound tissue-type plasminogen activator. In vitro studies in a plasma milieuArterioscler Thromb 1991 11:629-38. [Google Scholar]
[11]. McGorrian C, Yusuf S, Islam S, Jung H, Rangarajan S, Avezum A, INTERHEART Investigators. Estimating modifiable coronary heart disease risk in multiple regions of the world: the INTERHEART modifiable risk scoreEur Heart J 2011 32(5):581-89. [Google Scholar]
[12]. Shai I, Schulze M, Manson J, Stampfer M, Rifai N, Hu F, A prospective study of lipoprotein(a) and risk of coronary heart disease among women with type 2 diabetesDiabetologia 2005 48:1469-76. [Google Scholar]
[13]. Mora S, Kamstrup P, Rifai N, Nordestgaard B, Buring J, Ridker P, Lipoprotein(a) and risk of type 2 diabetesClinical Chemistry 2010 56(8):1252-60. [Google Scholar]
[14]. Qibin Q, Workalemahu T, Zhang C, Hu F, Qi L, Genetic variants, plasma lipoprotein(a) levels, and risk of cardiovascular morbidity and mortality among two prospective cohorts of type 2 diabetesEuropean Heart Journal 2011 33:325-34.doi:10.1093/eurheartj/ehr350 [Google Scholar]
[15]. American diabetes associationDiagnosis and classification of diabetes mellitusDiabetes Care 2014 37(Suppl 1):S81-90. [Google Scholar]
[16]. Norman GR, Streiner DL, Biostatistics: the bare essentials 2000 2nd editionTorontoBC Decker:76-77. [Google Scholar]
[17]. Roeschlau P, Bernt E, Gruber W, Enzymatic determination of total cholesterol in serumZ Klin Chem Klin Biochem 1974 12(5):226 [Google Scholar]
[18]. Siedel J, Schmuck R, Staepels J, Town MH, Long term stable, liquid ready to use monoreagent for the enzymatic assay of serum or plasma triglycerides (GPO-PAP method). AACC Meeting Abstract 34Clin Chem 1993 39:1127 [Google Scholar]
[19]. Sugiuchi H, Uji Y, Okabe H, Irie T, Uekama K, Kayahara N, Direct measurement of high-density lipoprotein cholesterol in serum with polyethylene glycol-modified enzymes and sulfated α-cyclodextrinClin Chem 1995 41:717-23. [Google Scholar]
[20]. Matsuzaki Y, Kawaguchi E, Morita Y, Evaluation of two kinds of reagents for direct determination of hdl-cholesterolJ Anal Bio-Sc 1996 19:419-27. [Google Scholar]
[21]. Friedewald WT, Levy RI, Fredrickson DS, Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifugeClin Chem 1972 18:499-502. [Google Scholar]
[22]. Burtis C, Ashwood E, CarbohydratesIn: Tietz textbook of clinical chemistry and molecular diagnostics 2012 ch 265th edLondonElsevier Health Sciences:719-720. [Google Scholar]
[23]. Little RR, Wiedmeyer HM, England JD, Wilke AL, Rohlfing CL, Wians FH, Interlaboratory standardization of measurements of glycohemoglobinsClin Chem 1992 38:2472-78. [Google Scholar]
[24]. Burtis C, Ashwood E, Lipids, lipoproteins, apolipoproteins, and other cardiovascular risk factorsIn: tietz textbook of clinical chemistry and molecular diagnostics 2012 ch 275th edLondonElsevier Health Sciences:785-86. [Google Scholar]
[25]. Burtis C, Ashwood E, Lipids, lipoproteins, apolipoproteins, and other cardiovascular risk factorsIn: tietz textbook of clinical chemistry and molecular diagnostics 2012 ch 275th edLondonElsevier Health Sciences:786-87. [Google Scholar]
[26]. Walldius G, Jungner I, Holme I, Aastveit AH, Kolar W, Steiner E, High apolipoprotein B, low apolipoprotein A-I, and improvement in the prediction of fatal myocardial infarction (AMORIS study): a prospective studyLancet 2001 358:2026-33. [Google Scholar]
[27]. Walldius G, Jungner I, Apolipoprotein B and apolipoprotein A-I: risk indicators of coronary heart disease and targets for lipid-modifying therapyJ Intern Med 2004 255/2:188-205. [Google Scholar]
[28]. Walldius G, Aastveit AH, Jungner I, Stroke mortality and the apoB/apoA-I ratio: results of the AMORIS prospective studyJ Intern Med 2006 259:259-66. [Google Scholar]
[29]. Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control studyLancet 2004 364:937-52. [Google Scholar]
[30]. Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control studyLancet 2005 366:1640-49. [Google Scholar]
[31]. McGorrian C, Yusuf S, Islam S, Jung H, Rangarajan S, Avezum A, INTERHEART Investigators. Estimating modifiable coronary heart disease risk in multiple regions of the world: the INTERHEART Modifiable Risk ScoreEur Heart J 2011 32(5):581-89. [Google Scholar]
[32]. Katulanda G, Katulanda P, Adler A, Peiris S, Draisey I, Wijeratne S, Apolipoproteins in diabetes dyslipidaemia in South Asians with young adult-onset diabetes: Distribution, associations and patternsAnnals of Clinical Biochemistry 2009 47:29-34.doi:10.1258/acb.2009.009080 [Google Scholar]
[33]. Sniderman AD, Lamarche B, Tilley J, Seccombe D, Frohlich J, Hypertriglyceridemic hyperapoB in type 2 diabetesDiabetes Care 2002 25:579-82. [Google Scholar]
[34]. Albers JJ, Marcovina SM, Imperatore G, Snively BM, Stafford J, Fujimoto WY, Prevalence and determinants of elevated apolipoprotein b and dense low-density lipoprotein in youths with type 1 and type 2 diabetesThe Journal of Clinical Endocrinology and Metabolism 2008 93(3):735-42. [Google Scholar]
[35]. Patel JV, Vyas A, Cruickshank JK, Prabhakaran D, Hughes E, Reddy KS, Impact of migration on coronary heart disease risk factors: comparison of Gujaratis in Britain and their contemporaries in villages of origin in IndiaAtherosclerosis 2006 185:297-306. [Google Scholar]
[36]. Hernandez C, Francisco G, Chacon P, Simo R, Lipoprotein(a) as a risk factor for cardiovascular mortality in type 2 diabetic patients: A 10-year follow-up studyDiabetes Care 2005 28(4):931-33. [Google Scholar]
[37]. Hiraga T, Kobayashi T, Okubo M, Nakanishi K, Sugimoto T, Ohashi Y, Prospective study of lipoprotein(a) as a risk factor for atherosclerotic cardiovascular disease in patients with diabetesDiabetes Care 1995 18(2):241-44. [Google Scholar]
[38]. Ródenas S, Sánchez-Cabezudo M, Cuesta C, [Correlations of the levels of HbA1c with plasma apoproteins and plasma lipoproteins in type II diabetic patients]Rev Esp Fisiol 1993 49(1):23-9.Spanish. PubMed PMID: 8378574 [Google Scholar]
[39]. Agoston-Coldea L, Mocan T, Gatfossé M, Dumitrascu DL, The correlation of apolipoprotein B, apolipoprotein B/apolipoprotein A-I ratio and lipoprotein(a) with myocardial infarctionOpen Medicine 2008 3(4):422-29.ISSN (Online) 2391-5463 [Google Scholar]
[40]. Guyton J, Dahlen G, Patsch W, Kautz J, Gotto A, Relationship of plasma lipoprotein Lp(a) levels to race and to apolipoprotein BArteriosclerosis, Thrombosis, and Vascular Biology 1985 5:265-72. [Google Scholar]
[41]. Kamboh M, Rewers M, Aston C, Hamman R, Plasma apolipoprotein a-i, apolipoprotein b, and lipoprotein(a) concentrations in normoglycemic hispanics and non-hispanic whites from the San Luis Valley, ColoradoAmerican Journal of Epidemiology 1997 146(12):1011-18. [Google Scholar]
[42]. Kostner GM, Krempler F, Lipoprotein(a)Curr Opin Lipidol 1992 3:279-84. [Google Scholar]
[43]. Kostner KM, Kostner GM, Factors affecting plasma Lp(a) levelsSemin Vasc Med 2004 4:211-14. [Google Scholar]
[44]. Kishore P, Kim SH, Crandall JP, Glycemic control and cardiovascular disease: what’s a doctor to do?Current Diabetes Reports 2012 12(3):255-64. [Google Scholar]