We describe a 77-year-old male who had right upper limb ischemic symptoms and history of unsuccessful right subclavian artery angioplasty. According to ultrasound findings, upper limb angiography was performed which confirmed stenosis of the left vertebral and right subclavian arteries. Percutaneous angioplasty and stenting of left vertebral and right subclavian arteries were performed in two separate sessions. Retrograde approach was scheduled for right subclavian artery angioplasty which is challenging due to potential risks to adjacent vertebral artery. This case reports underscores that percutaneous approaches may be preferential given their confirmed long-term efficacy and lower morbidity.
Angiography, Percutaneous transluminal angioplasty, Stenosis, Subclavian, Vertebral
Case Report
A 77-year-old male patient was referred to our hospital with ischemic symptoms including pallor, paresthesia, pulseless and rest pain of the right hand since two years. He also had dizziness for several months. His past history was unremarkable except for mild hypertension that was treated with amlodipine 5 mg daily and smoking 50 pack/year. He had a history of unsuccessful angioplasty of right subclavian artery two months ago in another center. On physical examination, there was a significant difference between right and left upper limb blood pressures. His heart and lung examinations were non contributory except S4 in cardiac auscultation. He had no chest discomfort or new onset dyspnea. A 12-lead ECG showed sinus rhythm with left axis deviation and left bundle branch block pattern. Transthoracic echocardiography revealed ejection fraction of 55%, mild left ventricular hypertrophy, mild diastolic dysfunction and mild mitral regurgitation.
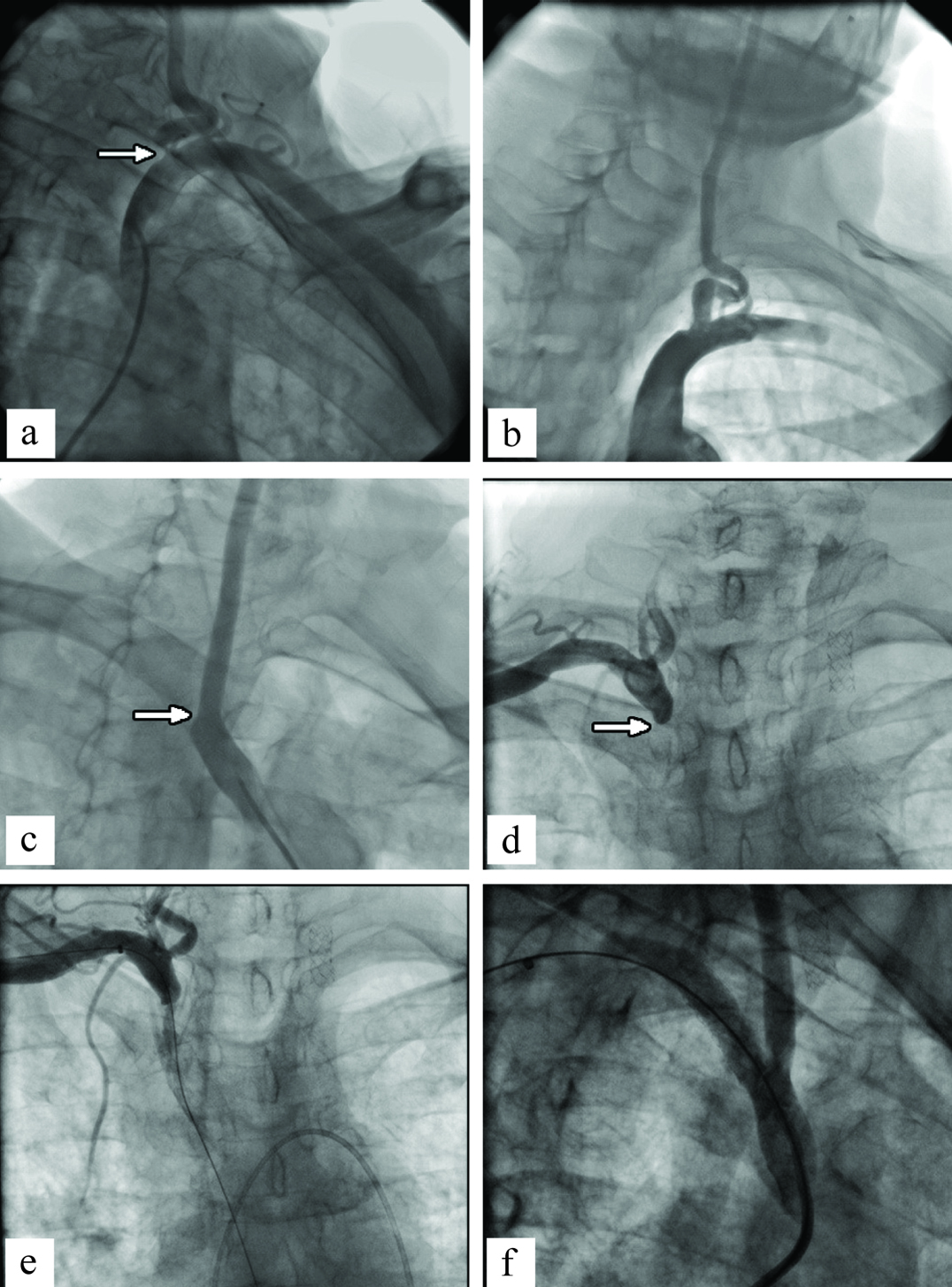
Duplex ultrasound demonstrated low flow in the right axillary and brachial artery. Based on clinical and duplex ultrasound findings upper limb angiography was performed which confirmed significant stenosis of the left vertebral and right subclavian arteries. The patient was selected for percutaneous transluminal angioplasty and stenting of left vertebral and right subclavian arteries in two separate sessions, respectively [Table/Fig-1]. On the first session, after selective angiography of left brachiocephalic artery, left vertebral artery revealed significant stenosis at origin. Due to this finding, guiding catheter (JR 3.5cm-7F) was engaged and wiring with Sionblue was performed; pre-dilation with Trek balloon (2.5 mm-15 mm) and Trek (4 mm-15 mm) was done. Then, peripheral stent (Palmazblue: 6 mm-18 mm) was deployed and post-dilation with Powerflex (7 mm-20 mm) was accomplished. On the next session, 2 weeks later, selective angiography of right brachiocephalic artery and retrograde injection of right brachiocephalic artery via redial artery showed that right subclavian artery was cut off at origin. Due to unsuccessful angioplasty of right subclavian artery in the past, retrograde approach via radial artery access was considered and Cook sheath (6F-70 cm) was placed; wiring with Conquestpro and pre-dilation with Trek balloon (4 mm-15 mm) and Invatec balloon (5mm- 20 mm) was performed. Then, guiding catheter (JR 3.5 cm- 8 F) via antegrade approach (from right femoral artery) was engaged and Genesis stent (8 mm-29 mm) was deployed and post-dilation with Powerflex balloon (9 mm-20 mm) was accomplished.
(a) selective angiography of left brachiocephalic artery showed that left vertebral artery had significant stenosis at origin; (b) final result of angioplasty and stenting of left vertebral artery; (c&d) selective angiography of right brachiocephalic artery and retrograde injection of right brachiocephalic artery via radial artery respectively revealed that right subclavian artery was cut off at origin; (e) retrograde approach via radial artery access was considered and wiring with Conquest pro was performed; (f) final result of angioplasty and stenting of right subclavian artery.
The patient was in good condition and discharged from hospital on ASA 81 mg and Clopidogrel 75 mg daily. He felt well in the following visit in cardiology clinic one and three months later and had no remarkable complaint.
Discussion
Subclavian artery stenosis can be a cause of substantial morbidity as it can initiate symptomatic ischemic problems affecting the upper extremities, brain and in some patients the heart [1,2]. Similar to the treatment of peripheral arterial disease in the lower limb, we may consider that endovascular revascularization to be the choice treatment option in subclavian artery lesions. However, it is not easy to evaluate results of patients with subclavian artery stenosis treated in an identical way. Percutaneous approaches may be preferential given their confirmed long term efficacy, lower morbidity and mortality, and cost effectiveness. Retrograde approach for chronic lesions of peripheral arteries including subclavian arteries could be so potentially an effective option; however, it may be challenging with regard to potential complications including dissection and compromising of the other arteries like carotids [3–5].
Subclavian artery stenosis or occlusion does not have a high incidence (1.9%) and is asymptomatic in a large number of cases. Just, symptomatic patients present for treatment that may underestimate the true incidence. Subclavian artery stenosis can be a cause of substantial morbidity as it can commence symptomatic ischemic problems affecting the upper extremities, brain and in some patients the heart. Atherosclerosis is the most frequent cause of this circumstance, but other less familiar underlying pathologies include arteritis, inflammation due to radiation exposure, fibromuscular dysplasia and compression syndromes should not be forgotten [1,2,6].
Akin to the treatment of peripheral arterial disease in the lower limb, we may conclude that endovascular revascularization to be the choice treatment decision in subclavian artery lesions. However; it is not easy to estimate results of patients with subclavian artery stenosis treated in an equal way. Although, our patient showed significant stenosis of right subclavian artery, the left side subclavian artery is more frequently affected.
Treatment options consist of open extraanatomic bypass grafting (Carotid-Subclavian Bypass (CSB), Carotid-Subclavian Transposition (CST) and Cross Over Bypass (COB) (axillo-axillary or subclavian–subclavian bypass) and Percutaneous Transluminal Angioplasty (PTA) and stenting [7].
It is not easy to weigh PTA against open extra-anatomic procedures because subclavian artery stenosis requiring treatment occurs occasionally. Furthermore, treatment options and materials are diverse that make the comparisons more complicated. Randomized controlled trials are lacking to accomplish a comprehensive conclusion. In general, primary and secondary patency rates are equivalent in both approaches although there are some reports of pre-eminence of open extra-anatomic procedures [4,5].
On the other hand, PTA and stenting is a minimally invasive approach that makes it so accepted in the recent years for peripheral arteries interventions [5].
Peripheral artery disease evaluation classically focuses on the review of lower extremity symptoms and physical findings. A small number of clinicians deem, the impact of upper extremity arterial disease; which, further leads to hand and arm symptoms, can be related with major neurologic and cardiac squeals [1].
Proper therapy after subclavian artery stenting has not been well established. The incidence of stent thrombosis is unusual due to large caliber of the artery. Per se, patients undergoing subclavian artery stenting should be treated with dual anti-platelet therapy for one month after the procedure (Clopidogrel 75 mg daily, aspirin 81 mg daily). After this one month period, aspirin alone should be maintained for an indefinite period [3,5,8].
We presented an interesting case with right subclavian and left vertebral artery stenosis that had history of unsuccessful right subclavian artery angioplasty. According to this circumstance and patient complaints including dizziness for several months, we approached to left vertebral artery initially. After left vertebral artery angioplasty, according to consultation with interventionists, we decided to approach to right subclavian artery. Thus, retrograde approach was scheduled for right subclavian artery angioplasty which is challenging due to potential risks of adjacent vertebral artery to be complicated; however, we achieved interestingly good results that exceeded our expectations.
Post-stenting follow up should be set up at one, six and 12-month intervals primarily and yearly subsequently. Besides history and physical examination, recording of bilateral arm blood pressures at each visit should be done. A color Doppler ultrasound with velocity assessment should be carried out with any suspicious symptoms or a greater than 10 mmHg difference in both arms blood pressure recordings [5].
Conclusion
In conclusion, vascular medicine clinicians including cardiologists and vascular surgeons should evaluate the patients with arterial disease for subclavian stenosis on a regular basis. There are excellent and effective treatment, preferences if diagnosed early. When the need for revascularization comes up, percutaneous approaches may be privileged given their definite long-term efficacy, lower morbidity and mortality, and cost effectiveness.
Disclosure Statement
The authors declare no conflict of interests.
Author Contributions
Study conception: MHN, Data collection: MHN, AM, Investigation: all authors, Writing: IK, Critical review and revision: all authors, Final approval of the article: all authors, Accountability for all aspects of the work: all authors.
[1]. Hennerici M, Klemm C, Rautenberg W, The subclavian steal phenomenon: a common vascular disorder with rare neurologic deficitsNeurology 1988 38:669-73. [Google Scholar]
[2]. Labropoulos N, Nandivada P, Bekelis K, Prevalence and impact of the subclavian steal syndromeAnn Surg 2010 252:166-70. [Google Scholar]
[3]. Brountzos EN, Petersen B, Binkert C, Panagiotou I, Kaufman JA, Primary stenting of subclavian and innominate artery occlusive disease: a single center’s experienceCardiovasc Intervent Radiol 2004 27:616-23. [Google Scholar]
[4]. Henry M, Henry I, Polydorou A, Polydorou A, Hugel M, Percutaneous transluminal angioplasty of the subclavian arteriesInt Angiol 2007 26:324-40. [Google Scholar]
[5]. Patel SN, White CJ, Collins TJ, Daniel GA, Jenkins JS, Reilly JP, Catheter-based treatment of the subclavian and innominate arteriesCatheter Cardiovasc Interv 2008 71:963-68. [Google Scholar]
[6]. Shadman R, Criqui MH, Bundens WP, Fronek A, Denenberg JO, Gamst AC, Subclavian artery stenosis: prevalence, risk factors, and association with cardiovascular diseasesJ Am Coll Cardiol 2004 44:618-23. [Google Scholar]
[7]. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FGR, Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II)J Vasc Surg 2007 45(Suppl S):S5-67. [Google Scholar]
[8]. Schillinger M, Haumer M, Schillinger S, Mlekusch W, Ahmadi R, Minar E, Outcome of conservative versus interventional treatment of subclavian artery stenosisJ Endovasc Ther 2002 9:139-46. [Google Scholar]