Prenatal Diagnosis and Management of Morbidly Adherent Placenta
Shreyasi Sharma1, Chanchal Singh2, Sohani Verma3, Harsh Rastogi4, Anita Kaul5
1 Research Fellow, Apollo Centre for Fetal Medicine, Indraprastha Apollo Hospital, New Delhi, India.
2 Consultant, Apollo Centre for Fetal Medicine, Indraprastha Apollo Hospital, New Delhi, India.
3 Senior Consultant, Department of Obstetrics and Gynaecology, Indraprastha Apollo Hospital, New Delhi, India.
4 Senior Consultant, Department of Radiology, Indraprastha Apollo Hospital, New Delhi, India.
5 Senior Consultant, Apollo Centre for Fetal Medicine, Indraprastha Apollo Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Chanchal Singh, Gate no 7, Apollo Centre for Fetal Medicine, Indraprastha Apollo Hospital, Sarita Vihar, New Delhi - 110076, India.
E-mail: chanchalsingh@gmail.com
Colour Doppler, Placenta accreta, Ultrasound
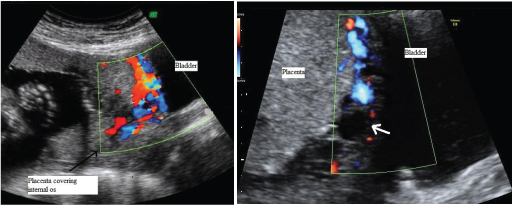
A 33-year-old G3P2L2 with previous two Lower Segment Caesarean Section (LSCS) presented to our Fetal Medicine Center for routine anomaly scan at 20 weeks gestation. Ultrasound was done using Voluson E8 (GE Healthcare, Milwaukee, WI, USA) equipped with convex 4–8 MHz abdominal transducer and 6-12 MHz transvaginal probe. Transabdominal ultrasound showed an anterior placenta covering the internal os completely (major placenta previa). This was confirmed on transvaginal ultrasound. On 2D imaging, the retroplacental sonolucent zone was irregular. Colour Doppler showed a highly vascular serosa-bladder interface raising a strong suspicion of Morbidly Adherent Placenta (MAP) [Table/Fig-1a]. Repeat ultrasound at 34 weeks showed the same findings [Table/Fig-1b].
Colour Doppler images at 20 weeks and 33 weeks showing disruption of the retroplacental sonolucent zone and vascular, confluent lagoons at the serosa-bladder interface.
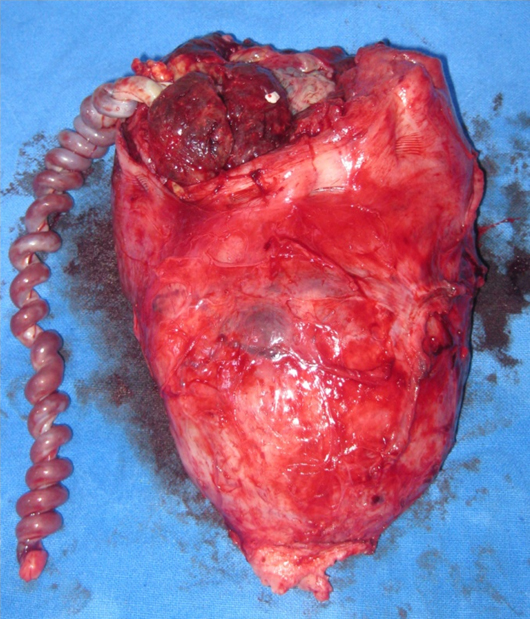
The patient did not have any complaint of vaginal bleeding or spotting throughout pregnancy. In view of strong suspicion of MAP, detailed preoperative workup and counseling was done and options including peripartum hysterectomy were discussed with the couple. A multidisciplinary team including obstetrician, fetal medicine specialist, intervention radiologist, haematologist and neonatologist were involved in patient management. Placental mapping was done by ultrasound prior to elective caesarean to plan the uterine incision so as not to cut into the placenta. Fetal growth was on the 5th centile for gestation with normal fetal Dopplers. Antenatal corticosteroids were given for fetal lung maturity. Elective upper segment caesarean section was done at 36 weeks with prophylactic preoperative uterine artery ballooning for anticipated postpartum haemorrhage. A baby girl weighing 2.0 kg with Apgar of 9,9 at 1 and 5 minutes was delivered. The placenta did not show any signs of separation intraoperatively. Total hysterectomy was done with the placenta in situ [Table/Fig-2]. Estimated blood loss was 800 ml. The patient did not require any blood transfusion. Histopathology confirmed placenta accreta [Table/Fig-3]. The mother and baby were discharged well on postoperative day three.
Caesarean hysterectomy specimen with the placenta in situ;
Histopathology of placenta (H&E stain, x20) showing lack of intervening decidua between chorionic villi and uterine myometrium.
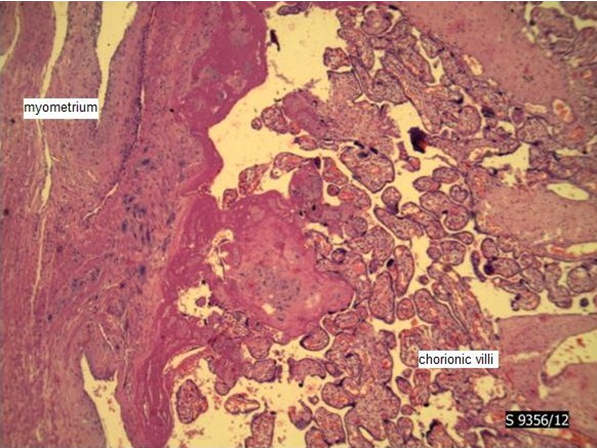
MAP is an implantation defect wherein the trophoblast invades into the myometrium in absence of an intervening decidua basalis. Risk factors include increasing maternal age, multiparity and more importantly, previous multiple dilatation and Curettage, myomectomy and/or previous caesarean delivery. Thus a careful history taking is the first step in diagnosing MAP. Recently reported incidence of MAP is as high as 1 per every 533 deliveries which is mainly attributed to the increase in caesarean deliveries [1]. The incidence increases from 0.04% in a woman with no previous caesarean section to more than 67% in a woman with previous 3 caesarean sections [1]. MAP is a potentially life-threatening condition and if unsuspected can lead to catastrophic postpartum haemorrhage, disseminated intravascular coagulopathy, renal failure, acute respiratory failure and maternal mortality [2]. Prenatal diagnosis is of paramount importance as it helps in appropriate preoperative planning, thereby decreasing potentially fatal complications. The sensitivity and specificity of ultrasound including Colour Doppler in diagnosing MAP is reported as 80-90% and 98% respectively [3]. In our patient, findings of large placental lacunae and increased vascularity at the bladder-placental interface raised a strong suspicion at the 20 week scan itself. Other ultrasound features suggestive of MAP include complete loss or disruption of the echolucent myometrial zone between placenta and bladder. The placental appearance is non-homogenous in MAP secondary to irregular shaped vascular spaces within its substance which show turbulent flow on Colour Doppler [4].
Antenatal suspicion in our patient helped in patient counseling and multidisciplinary management which is mandatory for these patients. A recently published study has proven that the morbidity in terms of requiring emergency caesarean delivery, estimated blood loss and blood transfusion requirements are significantly less when these patients are managed by a multidisciplinary team [5]. Preoperative placement of intravascular balloon catheter is a proven feasible and effective method of reducing blood loss in invasive placentation [6]. The same was done in our patient which indeed was helpful in reducing intraoperative blood loss. The good maternal and fetal outcome is attributed to timely diagnosis and adequate preparation which is essential in management of such cases.
[1]. Bauer ST, Bonanno C, Abnormal placentationSemin Perinatol 2009 33(2):88-96. [Google Scholar]
[2]. Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA, Maternal morbidity associated with multiple repeat cesarean deliveriesObstet Gynecol 2006 107(6):1226-32. [Google Scholar]
[3]. Palacios-Jaraquemada JM, Caesarean section in cases of placenta praevia andaccretaBest Pract Res Clin Obstet Gynaecol 2013 27(2):221-32. [Google Scholar]
[4]. Chou MM, Tseng JJ, Hwang JI, Ho ES, Lee YH, Sonographic appearance of tornado blood flow in placenta previa accreta/incretaUltrasound Obstet Gynecol 2001 17(4):362-63. [Google Scholar]
[5]. Bailit JL, Grobman WA, Rice MM, Reddy UM, Wapner RJ, Varner MW, Morbidly adherent placenta treatments and outcomesObstet Gynecol 2015 125(3):683-89. [Google Scholar]
[6]. Cali G, Forlani F, Giambanco L, Amico ML, Vallone M, Puccio G, Prophylactic use of intravascular balloon catheters in women with placenta accreta, increta and percretaEur J Obstet Gynecol Reprod Biol 2014 179:36-41. [Google Scholar]