The eye is a unique special sensory organ which exhibits diverse histologic structures. The knowledge of normal ocular anatomy and spectrum of pathologic changes that involve these structures is necessary. The rarity at which these lesions occur complicates the recognition of their fine and sometimes subtle presentation. Furthermore, clinical signs and symptoms of ocular malignancies simulate more commonly occurring benign conditions which pose great difficulties both for treating clinicians and even experienced pathologists. Also, there exists a variation in pattern and frequency on the basis of geographical locations [1].
Very few histopathologic studies have been conducted which include the complete spectrum of ophthalmic biopsies. The present study was therefore undertaken with the objective to determine the clinico-pathological spectrum of ophthalmic lesions at a tertiary care centre in Central India.
The knowledge of spectrum of ophthalmic lesions would be helpful to the ophthalmologists in shaping the strategy for diagnosis and management of ophthalmic lesions in this region.
Materials and Methods
After the ethical committee clearance, the data involving ophthalmic biopsies were evaluated retrospectively from January 2008 to November 2014 in the Department of Pathology of our institute. Total 488 biopsies and whole specimens were received from both the out-patients and in-patients attending the ophthalmology department of our institute. A proforma was used to collect a detailed clinical history of each patient.
The specimens were fixed, processed and stained with haematoxylin and eosin (H&E), and further ancillary studies were used as and when required. Immunohistochemistry (IHC) and special stains like Perodiac acid-Schiff (PAS) and silver stains were performed in difficult and rare cases for definitive diagnosis. Histomorphological diagnosis was made and evaluated as per epidemiological and clinico-pathological data.
Results
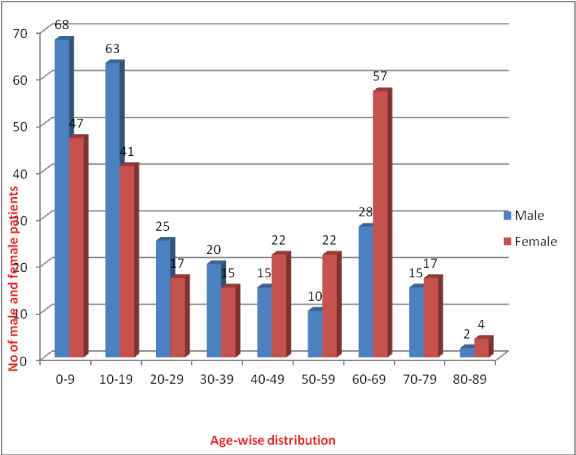
Total 488 cases of ophthalmic lesions were observed. It was found that ophthalmic lesions were highest (23.6%) in 0-9 years age group. Sex wise there was not much difference as lesions were found in 50.4% males and 49.6% females. But in the age group of 0-9 and 10-19 years, majority were males (27.6% and 25.6% respectively). While female preponderance (23.5%) was found in 60-69 years of age group [Table/Fig-1]. Ophthalmic lesions were distributed location wise to determine the sites commonly involved [Table/Fig-2].
Age and sex wise distribution of ophthalmic lesions.
Location wise distribution of ophthalmic lesions (N=488).
| Location | Cases (%) |
|---|
| Eyelid | 164(33.6%) |
| Lacrimal Sac | 121(24.8%) |
| Intra-ocular | 81(16.6%) |
| Conjunctiva and cornea | 73(15.0%) |
| Orbit | 35(7.2%) |
| Lacrimal gland | 14(2.9%) |
Clinical diagnosis was consistent with histopathological diagnosis in 76% cases. Maximum correlation was seen in the cases of malignant diagnosis. However, it was least in the cases of infectious aetiology like rhinosporidiosis and inflammatory pseudotumours which were misdiagnosed clinically as neoplastic lesions. Majority (61.1%) of the lesions were non-neoplastic. About 27.2% of the non-neoplastic lesions comprised of rhinosporidiosis [Table/Fig-3].
Histologic types of non-neoplastic lesions (N=298).
| Non-neoplastic | No. of cases | Percentage |
|---|
| Inflammatory | 121 | 40.6 |
| Cystic | 58 | 19.5 |
| Haemorrhage | 10 | 3.4 |
| Degenerative | 09 | 3.0 |
| Reactive hyperplasia | 09 | 3.0 |
| Infectious | | 91 | 30.5 |
| Rhinosporidiosis | 81 |
| Hydatid | 4 |
| Molluscum contagiosum | 2 |
| Cysticercosis | 2 |
| Fungal | 2 |
| Total | | 298 | |
Among the neoplastic lesions, 20.0% were benign and 80.0% were malignant. Among the benign ophthalmic lesions, angiomatous lesions followed by intradermal naevi were the most common, constituting 63.2% of all benign ophthalmic lesions [Table/Fig-4]. Among the malignant ophthalmic lesions, retinoblastoma, sebaceous carcinoma and SCC were the three most common tumours, constituting 69.7% of all malignant ophthalmic tumours. Retinoblastoma was common in the paediatric age group (<20 years). However, among adults >40 year age group sebaceous carcinoma (36.5%) was the commonest followed by SCC (21.0%) [Table/Fig-5].
Histologic types of benign ophthalmic lesions (N=38).
| Benign Lesion | No. of cases | Percentage |
|---|
| Angiomatous | 17 | 44.7 |
| Intradermal nevus | 07 | 18.4 |
| Compound nevus | 05 | 13.2 |
| Adenoma | 03 | 7.9 |
| Lipoma | 01 | 2.6 |
| Squamous papilloma | 01 | 2.6 |
| Schwannoma | 01 | 2.6 |
| Neurofibroma | 01 | 2.6 |
| Pilomatrixoma | 01 | 2.6 |
| Eccrine spiradenoma | 01 | 2.6 |
| Total | 38 | |
Histologic types of malignant ophthalmic lesions (N=152).
| Malignant Lesions | No. of Cases | Percentage |
|---|
| Retinoblastoma | 61 | 40.1 |
| Sebaceous carcinoma | 29 | 19.1 |
| SCC | 16 | 10.5 |
| Malignant lymphoma | 13 | 8.5 |
| Basal cell carcinoma | 06 | 3.9 |
| Rhabdomyosarcoma | 06 | 3.9 |
| Poorly differentiated carcinoma | 05 | 3.3 |
| Malignant melanoma | 05 | 3.3 |
| Adenocarcinoma | 04 | 2.6 |
| Adenoid cystic carcinoma | 02 | 1.3 |
| Undifferentiated carcinoma | 02 | 1.3 |
| Multiple myeloma | 01 | 0.7 |
| Spindle cell tumour | 01 | 0.7 |
| Primary neuroblastoma | 01 | 0.7 |
| Total | 152 | |
Among the eyelid lesions, rhinosporidiosis was the commonest followed by sebaceous carcinoma and dermoid cyst. Rare cases included pilomatrixoma and Rhabdomyosarcoma (RMS) of eyelid [Table/Fig-6].
Prevalence of different eyelid lesions (N=164).
| Eyelid Lesions | Cases (%) |
|---|
| Rhinosporidiosis | 38(23.2) |
| Sebaceous (meibomian) carcinoma | 25 (15.2) |
| Dermoid cyst | 22(13.4) |
| Chalazion | 9 (5.5) |
| Epidermal inclusion cyst | 8 (4.9) |
| Capillary haemangioma | 8 (4.9) |
| Chronic granulomatous lesions | 8 (4.9) |
| Intradermal nevus | 7 (4.3) |
| SCC | 6 (3.7) |
| Sebaceous cyst | 5 (3.0) |
| Pigmented basal cell carcinoma | 5 (3.0) |
| Malignant melanoma | 5(3.0) |
| Poorly differentiated carcinoma | 3 (1.8) |
| Sebaceous adenoma | 3 (1.8) |
| Cavernous haemangioma | 2 (1.2) |
| Undifferentiated carcinoma | 2 (1.2) |
| Molluscum contagiosum | 1 (0.6) |
| Eccrine spiradenoma | 1 (0.6) |
| Lipoma | 1 (0.6) |
| Neurofibroma | 1 (0.6) |
| Squamous papilloma | 1 (0.6) |
| Pilomatrixoma | 1 (0.6) |
| Adenoid basal cell carcinoma | 1 (0.6) |
| Rhabdomyosarcoma | 1 (0.6) |
| Total | 164 |
Corneal lesions were considered along with the conjunctival lesions. Among the corneal-conjunctival lesions, conjunctival cyst was the commonest followed by rhinosporidiosis [Table/Fig-7].
Prevalence of different corneal-conjunctival lesions (N=73).
| Conjunctival Lesions | Cases (%) |
|---|
| Conjunctival cyst | 19 (26.0) |
| Rhinosporidiosis | 17 (23.3) |
| Benign inflammatory lesion | 8 (11.0) |
| Well differentiated SCC | 8 (11.0) |
| Epidermal inclusion cyst | 5 (6.8) |
| Compound nevus | 5 (6.8) |
| Granuloma pyogenicum | 5 (6.8) |
| Capillary haemangioma | 2 (2.7) |
| Cysticercus cellulosae | 2 (2.7) |
| Poorly differentiated SCC | 2 (2.7) |
| Total | 73 |
Among the orbital lesions, non Hodgkin’s lymphoma (37.1%) was the commonest. Rare cases included primary neuroblastoma. Lacrimal sac lesions mainly included rhinosporidiosis and chronic dacryocystitis. Retinoblastoma was the most common intraocular pathology [Table/Fig-8].
Prevalence of different orbital lesions (N=35).
| Orbital Lesions | Cases (%) |
|---|
| Non Hodgkin lymphoma | 13 (37.1) |
| Inflammatory pseudotumour | 6 (17.1) |
| Cavernous haemangioma | 5 (14.3) |
| RMS | 5 (14.3) |
| Hydatid cyst | 2 (5.7) |
| Schwannoma | 1 (2.9) |
| Multiple myeloma | 1(2.9) |
| Primary neuroblastoma | 1 (2.9) |
| Spindle cell tumour | 1 (2.9) |
| Total | 35 |
Discussion
As the histopathology section of the Department of Pathology, receives biopsy specimens from the whole region, urban as well as rural, the data from this institute, although not an absolute representation, may still be considered a fair indicator of trends in distribution of ophthalmic lesions and may be taken as representative of this part of the country.
In the present study it was found that ophthalmic lesions were highest (23.6%) in 0-9 year age group. However, in study by Chauhan SC et al., majority of the cases were reported in 31-40 year age group [2]. This may be due to increased prevalence of rhinosporidiosis and retinoblastoma in this region.
Gender wise there was not much difference as lesions were found in 50.4% males and 49.6% females. But in the paediatric age group, majority were males (53.2%). While female preponderance (23.5%) was found in 60-69 years of age group. This may be because of more frequent occurrence of rhinosporidiosis in males in paediatric age group and sebaceous carcinoma in females in the elderly. Regarding sex wise distribution in malignant ophthalmic tumour, in present study 52% were males and 48% were females similar to those reported by others in Gujarat, Eastern Nepal and Singapore [2–4].
Clinical diagnosis was consistent with histopathological diagnosis in 76% cases. Accuracy was low in series by Chauhan SC et al., (49%) [2]. Other studies have reported it on higher side 84%. 91.5% and 96% [5–7]. Clinico-pathological correlation was poorest in eyelid lesions (38%) and highest for enucleation specimens (82%). This was similar to those observed by other studies [8]. Among eyelid lesions, correlation was poor mostly in cases of rhinosporidiosis clinically appearing as malignant mass, sebaceous carcinoma which were clinically considered as basal cell carcinoma and few cases of haemagioma diagnosed clinically as cystic masses. Among enucleation specimen, retinoblastoma was the reason behind high clinico-histopathological correlation. Few cases were clinically diagnosed as malignant masses which were later diagnosed as inflammatory pseudotumour histologically, case of multiple myeloma was also considered as malignant melanoma clinically. The core of a good approach for treating ophthalmic lesions continues to hinge on a good histopathologic study and diagnosis. So, clinico-pathological correlation is crucial, requiring good communication between the clinician and the pathologist.
Location wise, eyelid (33.6%) was the most commonly involved site, similar findings have been observed by Chauhan SC et al., [2]. Lacrimal gland (2.9%) was the least commonly involved site in our study but the least common site in the study of Chauhan SC et al., was lacrimal sac (2%) [2]. Rhinosporidiosis involving lacrimal sac attributed to higher number of cases in our study. In our study, as opposed to other studies the incidence of non-neoplastic lesions exceeded that of neoplastic lesions. This was probably due to the high incidence of rhinosporidiosis infection. Ocular rhinosporidiosis is worldwide in distribution but relatively more common in India [9]. Central India is amongst such areas where rhinosporidiosis is endemic, probably because of the hot and humid climate, where it is mostly seen in agricultural labourers belonging to low socioeconomic status.
Among the neoplastic lesions, malignant lesions were more commonly encountered (80.0%). This was similar to that observed by Ud-Din N et al., [10,11]. This may be because of high occurrence of retinoblastoma in both the series. However, the reverse was true in other studies [2,12–14] [Table/Fig-9].
Comparison of incidence of benign and malignant tumours with other studies.
| Study | Benign (%) | Malignant (%) |
|---|
| Ud Din N et al., [10] (Pakistan) | 38.5 | 61.5 |
| Shaikh IY et al., [13] (India) | 52.3 | 47.7 |
| Kapurdov A et al., [12] | 27.1 | 17.6 |
| Chauhan SC et al., [2] (India) | 70 | 30 |
| Bastola P et al., [14] (Nepal) | 70 | 30 |
| Charles NC et al., [11] Nigeria) | 29.5 | 31.4 |
| Present study | 20 | 80 |
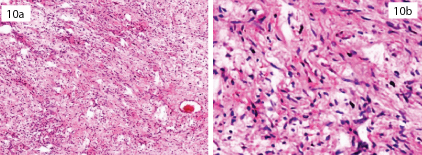
Among the benign ophthalmic lesions, angiomatous lesion (44.7%) followed by intradermal naevi (18.4%) were the most common. However, intradermal nevus has been reported as the commonest in other studies [15]. In series by Kapurdov A et al., papilloma was the commonest (70.66%) followed by nevus (14.05%) and vascular lesions (7.85%) [Table/Fig-10a,b] [12].
Neurofibroma; section shows typical small spindled cells with “S-shaped” nuclei within a variably myxoid matrix. [H&E; x10, x40].
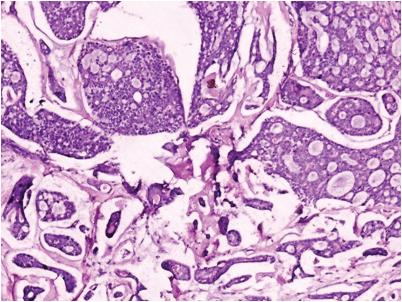
Among the malignant ophthalmic lesions, retinoblastoma (40.1%), sebaceous carcinoma (19.1%) and SCC (10.5%) were the three most common tumours. In series by Ud-Din N et al., from Pakistan, retinoblastoma was the commonest (24.5%) followed by SCC of conjunctiva (21.5%) and basal cell carcinoma (15.8%) [10]. However, in series by Kapurdov A et al., basal cell carcinoma was the commonest (68.79%) followed by SCC (12.1%) and melanoma (5.1%) [Table/Fig-11] [12].
Adenoid cystic carcinoma; section shows basaloid tumour cells with scanty cytoplasm. A cribriform pattern is seen with spaces filled with mucin. [H&E; x10].
However, in series from Nepal, SCC was the commonest (66.1%) supported by a study in Sudan which also showed it as the commonest tumour with 50.4% cases [1,16]. Poso MY et al., also reported it as the commonest tumour in their study with 33.5% cases [17]. The study expressed bimodal age distribution with one peak around 15 years and another around 55 years similar to other reports [2,4,10,18,19].
A high percentage of malignant ophthalmic lesions were observed in paediatric age group, due to retinoblastoma, which constituted 40.1% of all malignant ophthalmic lesions. Our findings were closer to those reported by other studies, 31.7%, and 32% respectively [17,18]. Thus, like in other studies, most common malignancy in children in present study was also retinoblastoma.
Some other studies however have reported lower values, 20.8% and 19.8% respectively [16,20]. It was still lower (6.7%) in series from Nepal [1]. The average age of retinoblastoma was 3.8 years with equal male to female ratio. Studies done in both Pakistan and India also reported same age distribution but with male predominance, while in Western countries the age of presentation is earlier. This earlier age of presentation in developed countries is probably due to better diagnostic facilities and increased awareness among public, which is lacking in our continent.
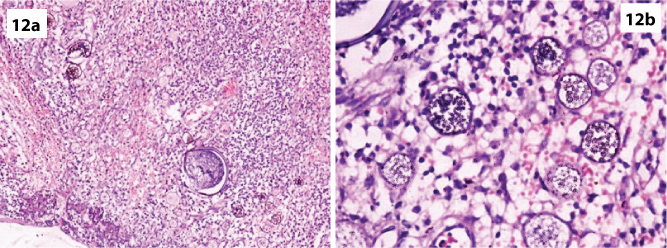
Among the benign eyelid lesions, rhinosporidiosis [Table/Fig-12a,b] was the commonest (23.2%) followed by dermoid cyst (13.4%), chalazion (5.5%), epidermal inclusion cyst (4.9%), and capillary haemangioma (4.9%). Except for the occurrence of rhinosporidiosis similar pattern was reported by Chauhan SC et al., dermoid cyst (21%), followed by epidermal inclusion cyst (14%) and intradermal nevus (12.2%) [2]. However, intradermal nevus (21.3%) was the commonest in series by Obata H et al., and vascular lesions (21.3%) were the commonest in series by Abdi U et al., [15,21]. The most common eyelid mass was chalazion (10.8%) in study by Akpe BA et al., [8].
Rhinosporidiosis of eyelid; section shows multiple thick-walled sporangia containing hundreds of spores. [H&E; x10, x40]. (Images left to right)
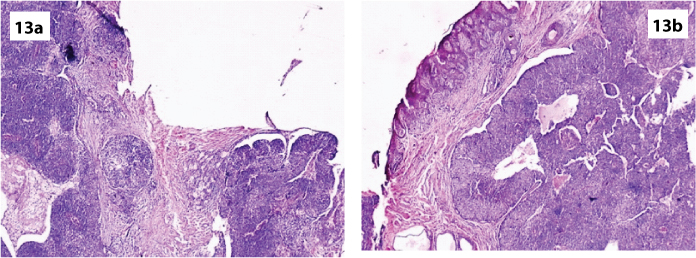
Among the malignant eyelid lesions, sebaceous carcinoma (15.2%) was the commonest which was similar to those observed by others (8.7%, 15%) [2,15]. An 86.2% of all sebaceous carcinomas occurred in eye lid and every case was >40 years of age [Table/Fig-13a,b]. The average age of presentation was 58.5 years with female preponderance. Studies in Korea, Nepal and India found 21.2%, 28.6% and 33% respectively [1,18,22]. However, according to Kass LG et al., it accounts for 1-5.5% of all eyelid malignancies in the USA [23]. However, basal cell carcinoma was the commonest in other series from Nepal, Sudan and Papua Guinea [1,16,24]. The most common malignant eyelid tumour in the United States and the United Kingdom is reported to be the basal cell carcinoma which occurs most frequently on the lower eyelid and medial canthus in elderly patients [25,26]. The most common malignant lid mass was SCC in study by Akpe BP et al., (16.9%) [8]. A high incidence of basal cell carcinoma and SCC is seen in individuals with fair skin due to exposure to sun light [27].
Sebaceous (mebomian) carcinoma. Section shows distinct nests of neoplastic cells (lobular variant). [H&E; x10].
Rare lesion encountered in eyelid included RMS which was immunohistochemically CD99, NSE1, Desmin and MyoD1 positive. Pure eyelid localization such as the case of our patient is rare. Most cases of reported eyelid RMS represent subcutaneous extension of the anterior orbital RMS.
Among the corneal-conjunctival lesions, 86.3% lesions were benign and 13.7% were malignant. Similar findings have been reported by other studies [2,15].
Among the benign corneal-conjunctival lesions, conjunctival cyst (26.0%) was the commonest followed by rhinosporidiosis (23.3%). In the study of Obata H et al., most common benign lesion was intradermal nevus (13%) [15]. While in study by Chauhan SC et al., the most common benign lesion was granuloma pyogenicum (22.5%) followed by intradermal nevus (4.5%) [2]. Squamous papilloma was the commonest benign tumour in series from West Bengal [28].
Among the malignant corneal-conjunctival lesions, SCC (13.7%) was the commonest similar to other studies [1,2,28]. An 80% of these were >40 years of age with average age of presentation at 50.7 years with female preponderance. Ultraviolet spectrum could be a factor for high incidence of this tumour, as large number of persons work in the open sun, especially farmers and workers are exposed to it. In the study of Obata H et al., however, the most common malignant lesion was malignant lymphoma (9%) [15].
Among the orbital lesions, non Hodgkin lymphoma (37.1%) was the commonest similar to other studies [2]. The other common lesions were inflammatory pseudotumour (17.1%), cavernous haemangioma (14.3%) and RMS (14.3%). About 83.3% of RMS occurred in the orbit with average age at presentation of four years. M:F ratio was 4:1. Rare case included primary neuroblastoma. IHC was performed which was positive for NSE and synaptophysin. In our patient the presentation was unusual because the age of presentation was 17 years of the age without any systemic manifestation and occured after evisceration of the eye.
The lacrimal gland carcinoma was found to be 2.9% in this series, similar to the findings of Sunderraj P et al., and Verma N et al., who found least number of 3% and 3.4% cases respectively in their studies [18,24]. Two cases of adenoid cystic carcinoma were reported.
Lacrimal sac lesions mainly included rhinosporidiosis and chronic dacryocystitis while retinoblastoma was the most common intraocular pathology. In contrast, malignant melanoma which is the most prevalent intraocular tumour in Caucasians, was rare in our series (3.3%) [29,30]. Similar rarity has also been reported in African series and in series from Nepal (5.1%) [1,29,30]. Malignant melanoma was reported 4.6% and 4.5% respectively in the studies [19,28]. The study conducted in Eastern Nepal and Nigeria reported 9.5% and 7.7% respectively of all ocular malignancies [3,31].
Limitation
The wide variation in spectrum of ophthalmic lesions and lesser number of comprehensive histopathological studies published so far from this geographical region refrain us from proper review of data and definitive conclusion.
Conclusion
Eye is the vital organ of the body for vision. Its anatomical position close to other vital structures of the head and neck increases the importance of the early diagnosis and treatment of its lesions. Varied presentation and vast spectrum of neoplastic and non-neoplastic lesions as encountered in our study emphasize the need for region-wise study of ophthalmic lesions. Rhinosporidiosis which forms an important differential in our region, due to its recurrence and dissemination to other parts of body makes early diagnosis and treatment important. Hence, to prevent this disease, awareness camps and poster distribution were organised in rural areas of the region by our institution. In this way, clinico-pathological studies have the greatest benefit to ongoing patient care and the purpose of our study will be met.