Oral Carcinoma Cuniculatum: A New Entity in the Clinicopathological Spectrum of Oral Squamous Cell Carcinoma
Uma Vasant Datar1, Alka Kale2, Deepa Mane3
1 Assistant Professor, Department of Oral Pathology and Microbiology, Bharati Vidyapeeth Deemed University Dental College and Hospital, Sangli, Maharashtra, India.
2 Professor, Department of Oral Pathology and Microbiology, KLE VK Institute of Dental Sciences, Belgaum, Karnataka, India.
3 Professor, Department of Oral Pathology and Microbiology, KLE VK Institute of Dental Sciences, Belgaum, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Uma Vasant Datar, Assistant Professor, Department of Oral Pathology and Microbiology, Bharati Vidyapeeth Deemed University Dental College and Hospital, Sangli-416414, Maharashtra, India.
E-mail: dataruv@gmail.com
Carcinoma cuniculatum is principally recognized as a variant of carcinoma involving foot. The World Health Organization (WHO) recognizes Oral Carcinoma Cuniculatum (OCC) as a distinct and rare clinicopathological variant of Oral Squamous Cell Carcinoma (OSCC). OCC is confused clinically and histologically with Verrucous Carcinoma (VC) and is often misdiagnosed as either VC or OSCC. To best of our knowledge, till date, only 50 cases of this tumour have been reported in oral cavity (including the present case) and only limited number of cases have been reported from Indian subcontinent. Pathognomonic feature of OCC is proliferation of stratified squamous epithelium and its infiltration into underlying stroma forming a complex pattern of keratin cores and keratin filled crypts. These complex crypts give it a likeness of rabbit burrow hence, the name cuniculatum (cuniculatus=‘rabbit warren’). The report aims to present a case of OCC of mandibular gingiva, discuss its diagnostic features and highlight its differences from VC and OSCC.
Differential diagnosis, Rabbit burrows, Verrucous carcinoma
Case Report
A 58-year-old female patient presented with a complaint of non healing ulcer present on right mandibular gingiva since three months. The patient had visited a private dentist who performed incisional biopsy of the lesion and the histopathological report suggested well differentiated OSCC. After receiving this report the patient was guided to our institute. A thorough history and clinical information was recorded in the institute. The patient did not disclose any habit history. Oral examination revealed an ulcerated, reddish white, pebbly growth on the buccal and lingual aspect of right mandibular second molar. Panoramic radiograph of the patient showed irregular radiolucent lesion involving the alveolar bone around right mandibular second molar. With clinical presentation, radiographic evidence of bone invasion and histopathological report of OSCC, treatment planned was, hemimandibulectomy with ipsilateral Type II modified neck dissection.
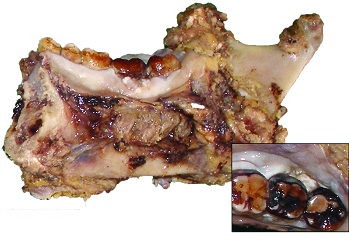
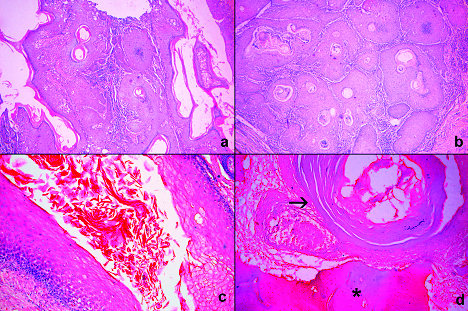
The resected specimen [Table/Fig-1] along with ipsilateral Type II modified neck dissection was sent for histopathological diagnosis. Microscopically the lesion revealed a well differentiated stratified squamous epithelium forming multiple, complex, branching keratin filled crypts [Table/Fig-2a-c]. These crypts showed the characteristic burrowing pattern. The tumour cells in the crypts showed mild cytological atypia and few mitotic figures limited to basal and parabasal layers. The tumour islands were seen invading the bony trabaculae [Table/Fig-2d]. A diagnosis of OCC was made based on the above mentioned observations. The tumour margins were clear of the tumour tissue and none of the regional lymph nodes demonstrated metastasis. After two years of postoperative follow up, the patient continues to be clinically and radiographically disease free.
Lingual view of resected hemimandibulectomy specimen is noted showing reddish white pebbly growth on the buccal and the lingual surface of right mandibular second molar, the inset shows occlusal view.
Photomicrographs showing: a) Deeply located branching crypts and keratin filled debris surrounded by squamous epithelium which resemble rabbit burrows; (H&E, 4X); b) Invasive front of cuniculatum (H&E, 4X); c) Keratin crypts surrounded by well differentiated squamous epithelium showing minimal atypia (H&E, 10X); d) Photomicrograph of decalcified section showing tumour islands invading in bone, arrow points the tumour island and * indicates the bone trabaculae (H&E, 10X).
Discussion
OCC is a rare variant of OSCC [1,2]. Carcinoma cuniculatum was first described in the foot by Arid I et al., in 1954 [3]. But OCC was first described in oral cavity by Fliegar S and Owanski T in 1977 [4]. The diagnostic feature of OCC is well differentiated epithelial cells which lack cytological atypia, exhibiting blunt papillary/pebbly surface and keratin filled crypts extending deep in the connective tissue [5,6]. These keratin filled crypts impart classic ‘rabbit burrow’ pattern to OCC. It has been noted that many pathologists are unacquainted with the lesion and the diagnostic criteria is not defined which has resulted in under-reporting of OCC.
OCC has been identified with a plethora of synonyms including epithelioma cuniculatum, Busche-Lowenstein tumour and inverted verrucous carcinoma [2,6]. The array of synonyms, failure to recognize it as a distinctive variant of OSCC and general lack of awareness about the lesion added to the rarity of the tumour and are accountable for the fewer number of published cases of OCC. Owing to this the frequency of the tumour has been underestimated [1]. The causative factors like tobacco, alcohol, trauma and Human Papillomavirus (HPV) have been indicated as aetiologic agents [1,5–7]. The presence of HPV DNA was demonstrated in cutaneous carcinoma but the association of HPV and OCC has not been proved till date [1,5,6]. In a recent case series, OCC which had preceding premalignant lesion/condition has been reported, indicating a multistep malignant transformation of premalignant lesion/condition to OCC [8].
In the cases of OCC reported till date, the most common site affected was mandibular gingiva [1,4–18]. The clinicopathological profile of cases of OCC reported till date is depicted in [Table/Fig-3], A wide age range of 7-92 years has been reported and slight male preponderance is noted [Table/Fig-3]. But in two recent case series of OCC slight female predominance was observed [6,7]. OCC presents as sessile white to pink slightly pebbly/papillary surface. Bone invasion is hallmark of OCC which was exemplified in the present case. The bone erosion was noted radiographically and the tumour islands were noted histopathologically.
Overview of previously published cases of oral carcinoma cuniculatum.
| Authors | Number of cases | Age/Gender | Site | preoperativeDiagnosis/InitialDiagnosis |
| Fliegar S and Owanski T [4] | 4 | 50/M | Maxillary molar and sinus | Osteomyelitis |
| 60/M | Maxillary molar region | Tuberculosis |
| 9/M | Maxillary premolar region | Not stated |
| 69/F | Hard palate | Not stated |
| Kahn JL et al., [13] | 3 | 62/M | Maxillary alveolus and sinus | Cystic lesion |
| 49/M | Submandibular space | Not stated |
| 52/M | Anterior floor of the mouth | Not stated |
| Delahaye JF et al., [14] | 5 | 51/M | Retromolar trigone | Squamous cell carcinoma |
| 55/M | Tonsil, floor of the mouth | Verrucouscarcinoma |
| 63/M | Subglottic larynx | Not stated |
| 31/M | Hard palate | Not stated |
| 52/M | Buccal mucosa | Not stated |
| Huault M [15] | 1 | 55/M | Mandibular alveolus | Hyperkeratoticpapilloma |
| Allon D [1] | 1 | 56/M | Maxillary gingiva | Giant cell lesion /Periodontal disease/ Malignancy |
| Raguse JD [16] | 1 | 81/F | Mandible | Osteomyelitis |
| Kruse AL and Graetz KW [17] | 1 | 74/F | Maxillary alveolus | Squamous cell carcinoma |
| Hutton A [18] | 1 | 7/M | Maxilla | Abscess |
| Pons Y et al., [9] | 3 | 72/M | Mandibular molar region | Inflammatorygranuloma |
| 82/M | Mandibular molar region | Not stated |
| 43/M | Mandibular retromolar region | Keratocyst |
| Thavaraj S et al., [5] | 1 | 61/M | Tongue | Not stated |
| Sun Y et al., [7] | 15 | Age-44-92Gender:7 Male, 8 Female | Tongue-8, Mandible-6, Oral vestibule-1 | Not stated |
| Fonseca FP et al., [10] | 2 | 62/M | Anterior mandible | Infectedorthokeratinizedkeratocyst |
| Padilla RJ and Murrah VA, [6] | 10 | 47/F | Maxillary gingiva | Osteomyelitis |
| 65/M | Mandibular gingiva | Erythroleukoplakia |
| 38/F | Mandibular gingiva | Benignproliferation |
| 72/M | Mandibular gingiva | Not stated |
| 81/F | Maxillary anterior region | Not stated |
| 67/F | Mandibular gingiva and buccal mucosa | Lichen planus/ Carcinoma |
| 79/M | Mandibular gingiva, vestibule | Not stated |
| 88/F | Maxillary ridge | Not stated |
| 75/F | Mandibular gingiva/ridge and buccal mucosa | Hyperkeratosis |
| 69/F | Mandibular alveolar region | Not stated |
| 85/F | Mandibular gingiva | Not stated |
| Shakil M et al., [11] | 1 | 63/F | Not stated | Not stated |
| Presentcase | 1 | 58/F | Mandibular gingiva | Oral squamous cell carcinoma |
| Total=50 | | | |
Histologically, OCC is characterized by presence of keratin filled crypts which are lined by stratified squamous epithelium showing minimal cellular atypia [6]. Histological differential diagnoses include well differentiated OSCC and VC [1,6]. Burrowing pattern, keratin filled crypts, lack of obvious cellular atypia and bone invasion differentiate OCC from well differentiated OSCC [2]. Correlation with clinical and radiographic features is essential for diagnosis.
OCC and VC demonstrate a peculiar overlap in their histological and clinical presentation, but they demonstrate a different biological course [1,2,6]. Hence, differentiation of the two lesions is essential [Table/Fig-4]. Both the lesions present with exophytic and endophytic components. They exhibit minimal cytological atypia, well differentiated tumour cells and excessive keratin production. These similarities are the reason for OCC being misdiagnosed as VC. The exophytic component of OCC has a blunt papillary/ cobblestone appearance whereas, VC has vertical fronds or ‘church spire-like’ structure [6,7]. Epithelial clefting and parakeratin plugging are hallmarks of VC whereas, OCC shows complex branching of keratin filled crypts. Pathognomonic feature of OCC is invasive epithelial component arranged in the form of keratin filled channels and cores which aids in diagnosing OCC [6,10]. VC has predominantly exophytic component but more restrained pushing front and it is limited to lamina propria [1]. On the other hand OCC burrows deep into underlying muscles and bone [1,6,8]. These features are evident in the present case. OCC is locally aggressive and distant metastasis is hardly reported [1].
Differential diagnosis between carcinoma cuniculatum and verrucous carcinoma.
| Carcinoma Cuniculatum | Verrucous Carcinoma |
| Aetiological Factors [1] | Alcohol, smoking | Snuff and tobacco chewing |
| Age [1,4–18] | 7-92 years | 50-80 years |
| Clinical Features [1,6,10] | Slow growing locally destructive;Blunt papillary/cobblestone surface;Infiltrating | Slow laterally growing;Broad warty, cauliflower-like growth;Exophytic |
| Radiological Features [10] | Deep invasion into the bone | Superficial bone erosion |
| Histopathological Features [1,6,10] | Well differentiated neoplastic cells with bland cytology and minimal cellular atypia;Chiefly endophytic growth pattern;Keratin filled crypts showing complex branching pattern are the hallmark of the tumour | Well differentiated neoplastic cells with bland cytology and minimal cellular atypia; Principally exophytic, and endophytic growth pattern; Vertical church-spire like keratinization and parakeratin plugging are the hallmark of the tumour |
| Immunohistochemical Findings [11] | Lesser expression of p53, Ki67 and p63;Strong expression of E cadherin, Integrin α6, Laminin 5γ2 | Strong expression of p53, Ki67 and p63;Negative for E cadherin, Integrin α6 and less expression of Laminin 5γ2 |
| Prognosis [7] | Better than OSCC, not good when compared to VC | Better than OCC and OSCC |
The burrowing pattern has been acknowledged as a hallmark of this lesion. A recent study has reported higher expression of E-cadherin, Integrin α6 and Laminin 5γ2 in OCC than in OSCC and VC, which may be the reason for the peculiar burrowing pattern of this entity [12]. Laminin 5γ2 is associated with invasion, its strong expression in OCC may be a sign of invasion and deep burrows of the lesion [12]. Accumulation of E cadherin (which is responsible for cell-cell adhesion) in OCC is presumed to be a cause of branching crypt construction [12].
Sun Y et al., also found lesser expression of Ki-67, p53 and p63 in OCC as compared OSCC and VC, suggesting that OCC is less aggressive, thus proving its known biological behaviour immunohistochemically [12]. Prognosis of OCC is reported to be good despite of evidence of metastasis. These findings support that the biological behaviour of OCC is different from VC and OSCC. But whether its prognosis is better than VC is still to be understood.
Conclusion
We reported a case of OCC, it is important to differentiate it from VC and OSCC and aspire to advance awareness of this distinct entity amongst pathologists. To reach to a correct diagnosis; deep biopsy, clinicopathological correlation is necessary and adequate sampling is essential. It is advisable that the clinicians furnish pathologists with clinical photograph to facilitate clinical correlation and provide generous biopsy from multiple sites if OCC is suspected and the pathologists are encouraged to procure extensive sectioning of the surgical specimen to aid in diagnosis. We also stress the need of establishing diagnostic criteria for OCC to distinguish it from VC.
[1]. Allon D, Kaplan I, Manor R, Calderon S, Carcinoma cuniculatum of the jaw: A rare variant of oral carcinomaOral Surg Oral Med Oral Pathol Oral Radiol Endod 2002 94:601-08. [Google Scholar]
[2]. Johnson N, Franceschi S, Ferlay J, Squamous cell carcinoma. In Barnes L, Eveson JW, Reichart P, Sidransky D, (Eds): World Health Organization Classification of TumoursPathology and Genetics of Head and Neck Tumours 2005 LyonIARC Press:168-75. [Google Scholar]
[3]. Arid I, Johnson HD, Lennox B, Epithelioma cuniculatum: A variety of squamous carcinoma peculiar to the footBr J Surg 1954 42:245-50. [Google Scholar]
[4]. Fliegar S, Owinski T, Epithelioma cuniculatum an unusual form of mouth and jaw neoplasmCzas Stomatol 1977 30:395-401. [Google Scholar]
[5]. Thavaraj S, Cobb A, Kalavrezos N, Beale T, Walker DM, Jay A, Carcinoma cuniculatum arising in the tongueHead Neck Pathol 2012 6:130-34. [Google Scholar]
[6]. Padilla RJ, Murrah VA, Carcinoma cuniculatum of the oral mucosa: a potentially underdiagnosed entity in the absence of clinical correlationOral Surg Oral Med Oral Patho Oral Radiol 2014 118:684-93. [Google Scholar]
[7]. Sun Y, Kuyama K, Burkhardt A, Yamamoto H, Clinicopathological evaluation of carcinoma cuniculatum: A variant of oral squamous cell carcinomaJ Oral Pathol Med 2012a 41:303-08. [Google Scholar]
[8]. Suzuki J, Hashimoto S, Watanabe K, Takahashi K, Usubuchi H, Suzuki H, Carcinoma cuniculatum mimicking leukoplakia of the mandibular gingivaAuris Nasus Larynx 2012 39:321-25. [Google Scholar]
[9]. Pons Y, Kerrary S, Cox A, Guerre A, Bertolus C, Gruffaz F, Mandibular cuniculatum carcinoma: Apropos of 3 cases and literature reviewHead Neck 2012 34:291-95. [Google Scholar]
[10]. Fonseca FP, Pontes HA, Pontes FS, de Carvalho PL, Senal-Filho M, Jorge J, Oral Carcinoma cuniculatum: Two cases illustrative of a diagnostic challengeOral Surg Oral Med Oral Patho Oral Radiol 2013 116(4):684-93. [Google Scholar]
[11]. Shakil M, Mohentesham I, Jose M, Prabhu V, Carcinoma cuniculatum of the oral cavity- A rare entityJ Adv Med Dent Scie 2014 2(1):124-26. [Google Scholar]
[12]. Sun Y, Kuyama K, Burkhardt A, Yamamoto H, An Immunohistochemical study of oral carcinoma cuniculatumInt J Oral Med Sci 2012b 10:333-43. [Google Scholar]
[13]. Kahn JL, Blez P, Gasser B, Carcinoma cuniculatum. Apropos of 4 cases with orofacial involvementRev Stomatol Chir Maxillofac 1991 92:27-33. [Google Scholar]
[14]. Delahaye JF, Janser JC, Rodier JF, Auge B, Cuniculatum carcinoma. 6 cases and review of the literatureJ Chir 1994 131:73-78. [Google Scholar]
[15]. Huault M, Laroche C, Levy J, Laxenaire A, Roucayrol AM, Scheffer P, Epitheloma cuniculatum. Apropos of a case in anterior gingiva with involvement of the mandibular symphyseal bone and reconstruction using a fibular osteocutaneous flap and integrated implantsRev Stomatol Chir Maxillofac 1998 99:143-48. [Google Scholar]
[16]. Raguse JD, Mennking H, Scholmann HJ, Bier J, Manifestation of carcinoma cuniculatum in the mandibleOral Oncol Extra 2006 42:173-75. [Google Scholar]
[17]. Kruse Al, Graetz KW, Carcinoma cuniculatum: A rare entity in the oral cavityJ Craniofac Surg 2009 20:1270-72. [Google Scholar]
[18]. Hutton A, McKaig S, Bardsley P, Monaghan A, Parmar S, Oral carcinoma cuniculatum in a young childJ Clin Pediatr Dent 2010 35:89-94. [Google Scholar]