Lymphoma is fourth most frequent malignancy diagnosed prenatally (~1:6000 cases), with Hodgkin’s Lymphoma (HL) forming the major chunk. However, in recent times, there has been an increase in occurrence of Non-Hodgkin’s Lymphoma (NHL) due to late child bearing age and high incidence of AIDS-related NHL in developing countries. Managing NHL in pregnancy involves intricate medical, ethical and psychological issues. Diagnostic and treatment delays may influence the prognosis for indolent cases. Seen the complexity of the management decisions associated with NHL, interdisciplinary and individualized approach becomes imperative for each woman. We present a case of 25-year-old G2P0010 at 32 weeks Period of Gestation (PoG) with right sided deep cervical lymphadenopathy, who was diagnosed as aggressive malignant NHL and was subsequently started on chemotherapy after confirmation of diagnosis and eventually had an optimal feto-maternal outcome. The critical appraisal of the accessible data, identification of controversies and unresolved issues and proposal of elucidations about varied facets of NHL in pregnancy are also provided.
Case Report
A 25-year-old G2P0010 at 32 weeks PoG was admitted in Obstetrics and Gynaecology Department at VMMC and Safdarjung hospital, New Delhi with complaint of gradually increasing swelling in right side of neck since two months. Her past history was unremarkable. She was afebrile and had normal blood pressure.
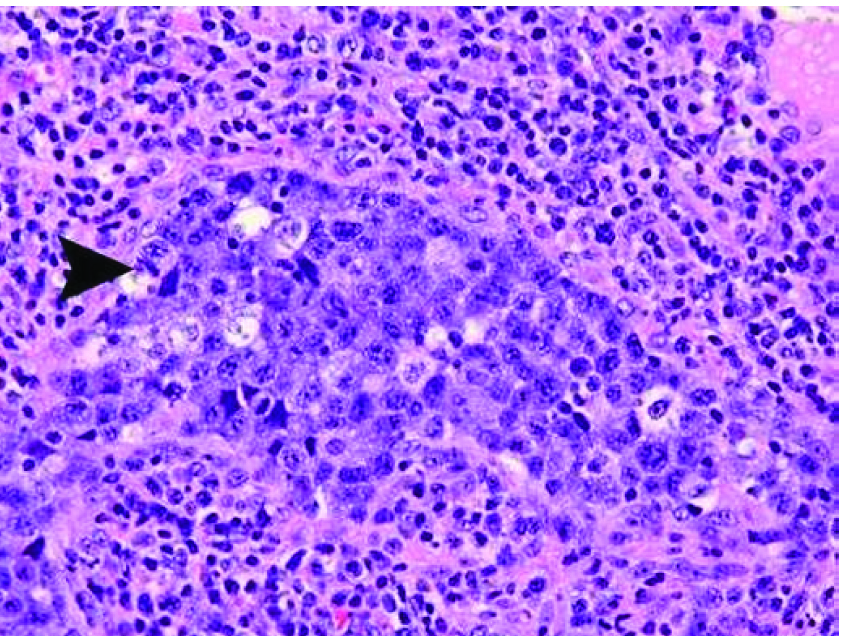
Clinical examination revealed right-sided large deep cervical lymphadenopathy measuring 3x4 cm. MRI neck showed bulky right deep cervical lymphadenopathy with peri-nodal spread, with small discrete lymph nodes in bilateral submandibular, left deep cervical and right supraclavicular region. Fine Needle Aspiration Cytology (FNAC) was then performed which was evocative of malignant lymphoma. Histopathology Examination (HPE) disclosed lymph node tissue with infiltration by sheets of large atypical cells with high nuclear/cytoplasmic ratio, vesicular nuclear chromatin and Immunohistochemistry (IHC) was Anaplastic Lymphoma Kinase-1 positive, suggestive of poorly differentiated anaplastic large cell lymphoma [Table/Fig-1]. Patient’s baseline antenatal investigations and ultrasound for biometry and anomaly scan of fetus were normal.
Histopathology suggestive of large cell anaplastic lymphoma showing sheets of large atypical cells (arrow head) HE 40X.
After giving steroid cover, first cycle of chemotherapy CHOP regimen was initiated followed by two uneventful doses of G-CSF. After one week, she developed chicken pox that was managed with tablet Acyclovir 800 mg five times a day for five days. At 34 weeks PoG, she had PPROM, and underwent LSCS for prolong leak and non-progress of labour. The procedure was uneventful.
Placenta was sent for HPE and fetal cord blood sample taken to rule out metastasis. Both mother and child recovered well in post-partum period. Next cycle of chemotherapy was planned 2 weeks postpartum. At the time of writing this report, about six months after her delivery, the mother has recuperated satisfactorily, complying justly with the chemotherapy schedule and is convalescing well.
Discussion
The NHL is a heterogeneous group of lymphoid malignancies, of either T or B-cell origin, with an estimated incidence of 0.8 cases per 100,000 women during pregnancy [1–5]. However, the current trend to postpone pregnancy and mounting incidence of HIV associated lymphoma in developing countries has led to an increase in the occurrence of NHL in pregnancy [2–4].
Usual presenting symptoms of NHL are often absent in pregnancy, delaying diagnosis. Most women (66%) present with lymphadenopathy (as in the index case). Though, aetiology still remains elusive, viral agents, most notably Epstein-Bar virus, human T-cell lymphotropic virus, Hepatitis C Virus (HCV), and HIV and immunosuppression (whether primary or iatrogenic) are well established risk factors for the development of NHL [6].
Though many variants have been reported, mostly NHL seen in pregnancy is of aggressive histology, like Diffuse Large B Cell Lymphoma (DLBCL) [5].
Apart from the local tissue diagnosis on the basis of lymph node biopsy, a pathologic placental evaluation post-delivery should be done routinely to assess the need for appropriate staging and therapy in the neonate [1]. Appropriate screening methods may be employed for detection of metastasis after delivery [5].
Bone marrow involvement is more frequent in indolent lymphomas (39%), besides a high involvement of the breast, uterus, cervix and ovaries are also observed. However, no difference in clinical behavior is observed in pregnancy. The risk of spontaneous abortion is comparable with that of normal miscarriage, without a significant increase in risk of maternal death, birth defects or late neurodevelopment delays. The NHL complicating pregnancy, being aggressive, is often disseminated with poor prognosis.
Obstetricians have the options of initiating treatment accepting some risk to the fetus, therapeutic abortion, or deferring management until delivery. Decision should be made only after taking into consideration woman’s feeling and values besides clinical status and natural history of the particular lymphoma, classification and international prognostic index [Table/Fig-2] [7].
Possible decision tree for treatment of Non-Hodgkin Disease in first trimester of pregnancy (Pereg 2007) [7].
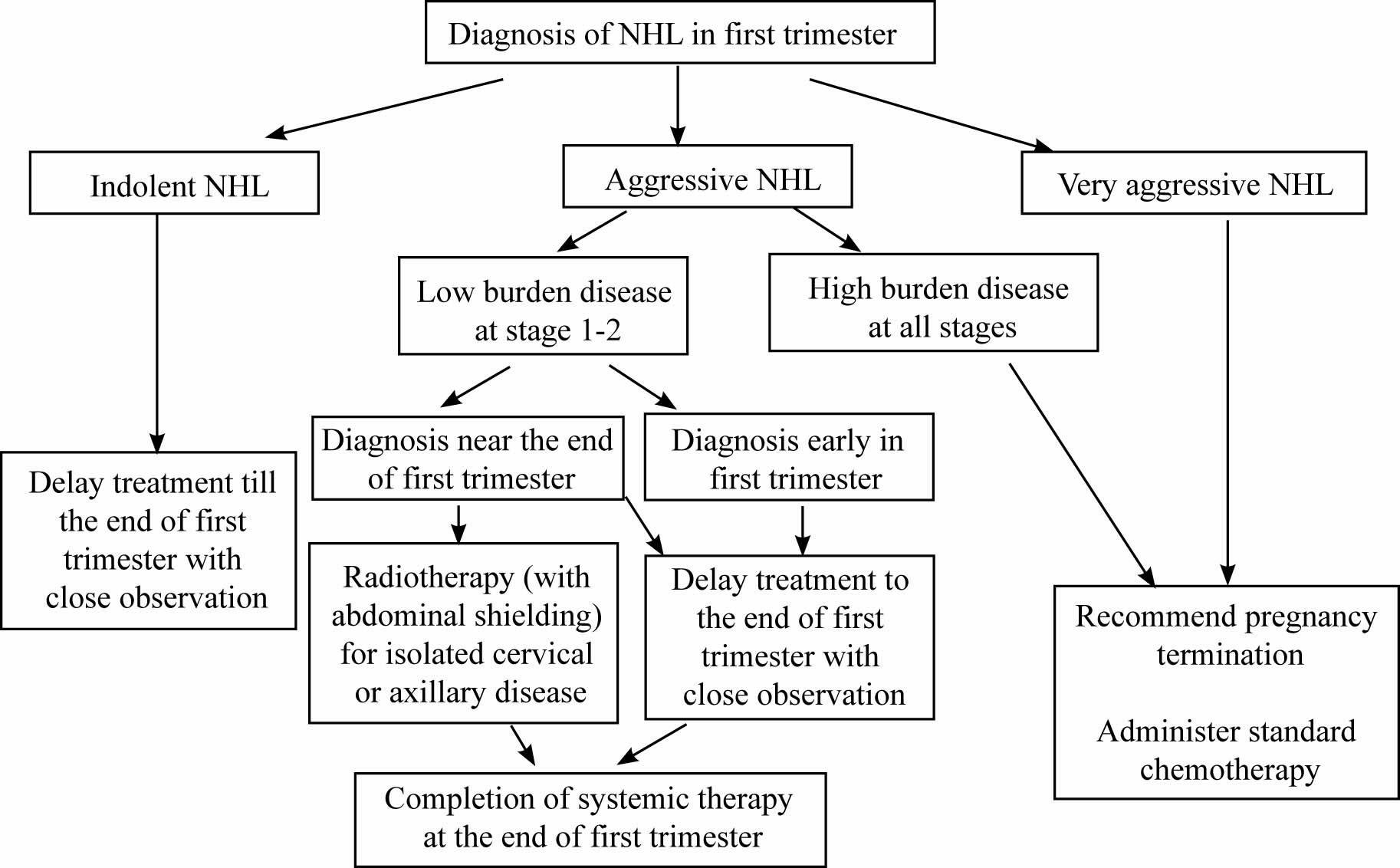
When diagnosed, patients of indolent NHL are often asymptomatic, not requiring immediate therapy. In Aggressive NHL/ Highly aggressive NHL, whenever possible, it should be deferred until the second trimester, after the completion of organogenesis. Meticulous observation until delivery could be considered in those women presenting with early stage disease, low-volume disease, no B cell symptoms and low International Prognostic Index (IPI) score [6]. Immediate therapy should be initiated in women with bulky disease or poorer prognostic indicators. Pregnancy termination (therapeutic abortion) should also be pondered over in such cases in light of high risk of fetal malformations. If termination is unacceptable to the patient, single agent treatment with Anthracycline antibiotics or Vinca-alkaloids followed by multi-agent therapy at the end of the first trimester can be contemplated.
Gained from the propitious pregnancy outcomes in several reports with chemotherapy initiation in second trimester, standard treatment chemotherapy is usually instituted irrespective of potential fetal risks [8].
The highly aggressive varieties should be managed with pregnancy termination followed by highly intensive combination chemotherapy, with or without Rituximab [9,10].
Radiation therapy is reserved for early stages of DLBCL, or post-chemotherapy in bulky disease. A full term delivery (≥37 weeks) should be targeted unless maternal and /or fetal health are endangered. Consideration should be given to postponing delivery for 2-3 weeks following treatment to allow maternal bone marrow recovery. A caesarean delivery is not warranted unless otherwise indicated, because staging laparotomy is no longer recommended. The placenta should be subjected to histological examination [7].
Optimal time for conception following NHL diagnosis/treatment should take into regard time of completion of therapy, risk of relapse, age and ovarian function of the women [1].
Soon after diagnosis, young women desiring future fertility should be counselled on available fertility preserving options before starting treatment, to facilitate prompt referral to fertility specialists. Use of GnRH analogues concurrently with chemotherapy is not a reliable means of preserving fertility [11,12]. Embryo or oocyte cryopreservation is the method of paramount importance to preserve female fertility. Ovarian stimulation should be done with Gonadotropins and Letrozole or Tamoxifen before commencing chemotherapy. Consideration of such an approach requires intensive interdisciplinary discussions involving oncologist, radiotherapists and reproductive medicine specialists.
Stewart and Gordon et al., reported a 25-year-old gravida 2 para 1 at 34 4/7 weeks’ gestation with acute liver failure, who also had a tender posterior cervical lymphadenopathy measuring 3x3 x2 cm, like the present case [13]. After induced delivery, biopsies were performed on postpartum day 2, suggestive of NHL. Further evaluation helped in establishing lymphomatous involvement of the porta hepatis as the cause of the acute liver failure in her. Despite aggressive treatment which was initiated on postpartum day four, she succumbed 6 months later.
Windom et al., reported a 26-year-gravida 2, para 1, with a twin gestation at 28 weeks’ gestation with gigantomastia without any axillary adenopathy [14]. She also had a lateral rectus palsy and trigeminal neuralgia. She developed preterm labour and delivered vaginally. During the episiotomy repair, a 1 to 2 cm, skin-covered, subcutaneous nodule on the left labium majus was discovered. Histology showed dermal infiltration by a high-grade, small, non-cleaved cell lymphoma. Further, evaluation suggested, NHL and chemotherapy with the ProMACE-CytaBOM regimen was started. After multiple relapses, she died 9 months after diagnosis. Both these cases also highlighted the significance of a high clinical suspicion, along-with an early diagnosis and initiation of therapy, as a vital tool for preventing complications of NHL in pregnant women. Also, a review by Alexander DD et al., acknowledged the mounting evidence of aetiologic heterogeneity amongst NHL and advocated future epidemiologic investigations on NHL to be boosted by scrutiny of types of NHL [15], better dependability and cogency of exposure assessment tools to evaluate occupational, environmental and personal exposures, and appraisal of susceptible subgroups.
Conclusion
The management of NHL during pregnancy is a challenging endeavor, which not only requires proficient knowledge by the clinicians but also sound clinical judgment and compassion, keeping in mind the patient and family preferences and, ultimately, the wellbeing of the neonate.
[1]. Peccatori FA, Azim HA, Orecchia R, Hoekstra HJ, Pavlidis N, Kesic V, Cancer, pregnancy and fertility: ESMO clinical practice guidelines for diagnosis, treatment and follow-upAnnals of Oncology 2013 Suppl 6:vi160-vi170. [Google Scholar]
[2]. Pentheroudakis G, Pavlidis N, Cancer and pregnancy: poena magna, not anymoreEur J Cancer 2006 42:126-40. [Google Scholar]
[3]. Stensheim H, Møller B, van Dijk T, Fosså SD, Cause-specific survival for women diagnosed with cancer during pregnancy or lactation: a registry-based cohort studyJ Clin Oncol 2009 27:45-51. [Google Scholar]
[4]. Matthews TJ, Hamilton BE, Delayed child bearing: more women are having their first child later in lifeNCHS Data Brief 2009 21:1-8. [Google Scholar]
[5]. Wang PI, Chong ST, Kielar AZ, Kelly AM, Knoepp UD, Mazza MB, Imaging of pregnant and lactating patients: part 2, evidence-based review and recommendationsAJR Am J Roentgenol 2012 198:785-92. [Google Scholar]
[6]. Avil A, Neri N, Nembo MJ, Hematological malignancies and pregnancy: treat or not treat during first trimesterInt J cancer 2012 131:2678-83. [Google Scholar]
[7]. Pereg D, Koren G, Lishner M, The treatment of Hodgkin’s and non-Hodgkin’s lymphoma in pregnancyHaematologica 2007 92:1230-37. [Google Scholar]
[8]. Brenner B, Avivi I, Lishner M, Hematological cancers in pregnancyLancet 2012 379:580-87. [Google Scholar]
[9]. Azim HA, Peccatori FA, Pavlidis N, Treatment of the pregnant mother with cancer: a systematic review on the use of cytotoxic, endocrine, targeted agents and immunotherapy during pregnancy Part I: solid tumoursCancer Treat Rev 2010 36:101-09. [Google Scholar]
[10]. Badawy A, Elnashar A, El-Ashry M, Shahat M, Gonadotropin-releasing hormone agonists for prevention of chemotherapy-induced ovarian damage: prospective randomized studyFertil Steril 2009 91:694-97. [Google Scholar]
[11]. Demeestere I, Brice P, Peccatori FA, Kentos A, Gaillard I, Zachee P, Gonadotropin-releasing hormone agonist for the prevention of chemotherapy-induced ovarian failure in patients with lymphoma: 1-year follow-up of a prospective randomized trialJ Clin Oncol 2013 31:903-09. [Google Scholar]
[12]. Andrew M. Evens, Advani R, Press OW, Lossos IS, Vose JM, Francisco J, Lymphoma occurring during pregnancy: Antenatal therapy, complications, and maternal survival in a multicenter analysisJournal of Clinical Oncology 2013 31(32):4132-39. [Google Scholar]
[13]. Stewart KS, Gordon MC, Non-Hodgkin lymphoma in pregnancy presenting as acute liver failureACOG 1999 94(5):847 [Google Scholar]
[14]. Windom KW, McDuffie RS, Non-Hodgkin’s lymphoma presenting with gigantomastia in pregnancyACOG 1999 93(5):852 [Google Scholar]
[15]. Alexander DD, Pamela J, Mink PJ, Adami HO, Chang ET, Cole P, The non-Hodgkin lymphomas: A review of the epidemiologic literatureInt J Cancer 2007 120:1-39. [Google Scholar]