Visible Evidence of Lumbar Epidural Catheter Misplacement–A Critical Incident Case Report
Rajkiran Shah1, Beena Butala2, Geeta Parikh3, Rajesh Pargi4
1 Associate Professor, Department of Anaesthesiology and Critical Care, Smt. K.M. Mehta and Smt.G.R. Doshi Institute of Kidney Diseases and Research Center, Ahmedabad, Gujarat, India.
2 Professor and Head, Department of Anaesthesiology and Critical Care, Smt. K.M. Mehta and Smt.G.R. Doshi Institute of Kidney Diseases and Research Center, Ahmedabad, Gujarat, India.
3 Professor, Department of Anaesthesiology and Critical Care, Smt. K.M. Mehta and Smt.G.R. Doshi Institute of Kidney Diseases and Research Center, Ahmedabad, Gujarat, India.
4 Resident, Department of Anaesthesiology and Critical Care, Smt. K.M. Mehta and Smt.G.R. Doshi Institute of Kidney Diseases and Research Center, Ahmedabad, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rajkiran Shah, Type B/4/3, GSECL Colony, TPS Gandhinagar, Gandhinagar-382041, Gujarat India.
E-mail: drrajkiran79@gmail.com
One of the causes of failed epidurals is catheter misplacement. Though various techniques of epidural space identification have been developed, none of them is 100% successful. Here, we present a case of lumbar epidural catheter misplacement in a patient scheduled to undergo right sided open nephrectomy. Catheter was found in the surgical field coming out of psoas major muscle.
Anaesthesia, Epidural space, Psoas muscle
Case Report
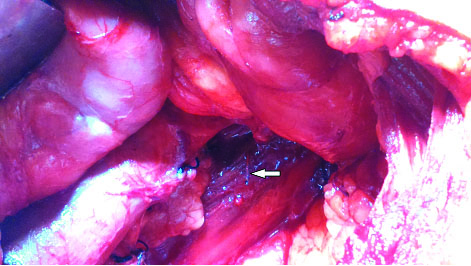
A 57-year-old, male patient (165 cm, 66 kg) was scheduled to undergo right radical nephrectomy for renal cell carcinoma. Clinical history, physical examinations and laboratory investigations of the patient were normal. After placing the patient in right lateral position, epidural space was identified at first attempt with 18G Tuohy needle (BD Perisafe, Belgium) via a midline approach at L2-L3 intervertebral space using loss of resistance to air technique. A 20G multiorifice epidural catheter was threaded through the cranially directed tip of epidural needle to the 15 cm mark. The needle was removed and the catheter was left 6 cm into the epidural space. Patient did not complain of pain or paraesthesia during the procedure. Because of paucity of time both epidural test dose (3 ml of 2% lignocaine with 1:200000 epinephrine) and analgesia was given after induction of general anaesthesia. After pre-medication with fentanyl 100 μg intravenous (IV), the patient was given balanced general anaesthesia. Induction was performed with propofol 150 mg IV and atracurium 35 mg IV was given to facilitate endotracheal intubation and was maintained with isoflurane 0.2% – 0.8% in an oxygen–nitrous oxide mixture at a 1:1 ratio. After induction, 0.25% bupivacaine 10 ml was given through epidural catheter without having any effect on haemodynamics. Surgery proceeded via right subcostal incision with the patient in the supine position. The right kidney was removed and near the end of surgery, when the surgeon was examining the renal bed, the distal portion of the epidural catheter was seen. The catheter was lying parallel to the inferior vena cava in front of psoas major muscle at the L1-L2 level [Table/Fig-1]. Retrograde dissection revealed the catheter emerging from the anterior vertebral fascia at the L2-L3 level. Further confirmation was done by flushing the catheter with the normal saline which was coming out of the multiorifice at the distal end of the catheter. Catheter was removed and intravenous tramadol was used for postoperative pain management.
Lumbar epidural catheter (arrow) coming out of psoas major muscle parallel to inferior vena cava at L1-L2 intervertebral space.
Discussion
Critical incident reporting is a valuable part of quality assurance. Identifying and mitigating risk factors associated with patient harm can improve patient safety [1]. Though various imaging studies and direct evidence case reports of epidural catheter misplacement in different regions of vertebral column have been reported, only one case of direct visible evidence of transforaminal escape of lumbar epidural catheter has been reported to our knowledge [2].
Due to lack of uniform outcome measures, incidence of failure of epidural anaesthesia and analgesia ranges from 13% to as high as 47% [3]. Factors that influence the technical failure of epidural anaesthesia and analgesia are, anatomical catheter location, patient position, puncture site, midline versus paramedian approach, methods to localize epidural space, catheter insertion and fixation and equipment related problems.
Three cases of misplaced epidural catheter into the thoracic cavity found during surgery have been reported. In all the cases, the probable cause of complication was difficult in locating the epidural space. In one case intercostal space was mistakenly identified as epidural space at 7.2 cm from the back of skin [4]. In second case, difficulty in positioning due to stiffness of neck, while in third, paramedian approach was the cause of complication [5,6]. Loss of resistance to air or saline is commonly used technique to locate epidural space. The authors have suggested alternate methods like drip infusion or use of imaging like fluoroscopy and ultrasound to locate epidural space.
In our case, length of epidural catheter inside the epidural space seems to be the probable cause of the complication. Different recommendations exist in the textbooks on the length of epidural catheter that is to be advanced into the epidural space ranging from 2-3 cm to 2-6 cm [7,8]. The shorter the length of the epidural catheter into the epidural space, more likely it is to become dislodged. This is more likely to occur postoperatively due to patient movement and change in posture. Conversely, the further the catheter advanced, the greater the chances of malposition, either transforaminal escape or into the anterolateral epidural space giving rise to unilateral block. Halpenny DG et al., reported the similar case of transforaminal escape of lumbar epidural catheter [2]. They found that transforaminal escape can occur even without elicitation of paraesthesia and without excessive threading of epidural catheter into the epidural space.
Epidurography was done in 268 patients to determine postoperative indwelling epidural catheter position by Uchino T et al., [9]. Among the 46 cases of lower thoracic and lumbar epidural catheter placement in this study, seven cases exhibited imaging agent leakage into the psoas compartment. However, out of these seven cases, one, two and four cases found to be effective, moderately effective and not effective, respectively, in terms of peroperative anaesthesia and analgesia. In the similar study of 90 patients by Sanchez A et al., comprising of two groups divided according to the length of the epidural catheter threaded (20 cm versus 12.5 cm taking the skin as reference), found to have slightly higher incidence of intervertebral foramen escape (6-7%) [10]. They also found that when an attempt was made to pass a catheter in the cephalad direction about 40% failed to pass upwards beyond the first interspace in both the groups. Another imaging study using computed tomography in 20 patients by Hogan Q et al., was done to determine epidural catheter tip position and distribution of injectate found the tip of eight catheters in or near the posterior epidural space; nine in the intervertebral foramina and two in the paravertebral tissues lateral to the intervertebral foramina [11]. Afshan G et al., recruited 102 women for epidurography and assigned them in three study groups to determine appropriate length of epidural catheter in the epidural space (3, 5 and 7 cm insertion) for postoperative analgesia [12]. They concluded that although postoperative analgesia was comparable in all the three groups, 5 cm epidural catheter is the most appropriate length to minimize the catheter related complications.
Conclusion
Unlike difficulty in epidural space identification as the cause of epidural catheter misplacement in previously reported cases, excessive threading of epidural catheter inside the epidural space could be the cause in our case. Further studies are required to recommend optimum length of epidural catheter to be placed in epidural space for successful anaesthesia and postoperative analgesia.
[1]. Zeng L, Yi Ng S, Thong S, Analysis of critical incidents during anaesthesia in a tertiary hospitalInt J Clin Med 2016 7:320-33. [Google Scholar]
[2]. Halpenny DG, Loken RG, Williams JA, Transforaminal escape of a lumbar epidural catheterCan J Anaesth 1992 39(6):594-95. [Google Scholar]
[3]. Hermanides J, Hollmann MW, Stevens MF, Lirk P, Failed epidural: Causes and managementBr J Anaesth 2012 109(2):144-54. [Google Scholar]
[4]. Kim YB, Lee SY, Intercostal misplacement of a thoracic epidural catheter -A case reportKorean J Anaesthesiol 2010 59(5):344-47. [Google Scholar]
[5]. Wadhwa R, Sharma S, Poddar D, Sharma S, Pleural puncture with thoracic epidural: A rare complication?Indian J Anaesth 2011 55(2):163-66. [Google Scholar]
[6]. Sundary MT, Epidural catheter misplaced into the thoracic cavity: Utilized to provide interpleural analgesiaAnaesth Essays Res 2015 9(1):121-23. [Google Scholar]
[7]. Miler RD, Miller’s anaesthesia 2010 7th edUnited States of AmericaElsevier [Google Scholar]
[8]. Morgan GE, Mikhail MS, Murray MJ, Clinical Anaesthesiology 2006 4th edUnited States of AmericaMcGraw-Hill Companies, Inc [Google Scholar]
[9]. Uchino T, Hagiwara S, Iwasaka H, Kudo K, Takatani J, Mizutani A, Use of imaging agent to determine postoperative indwelling epidural catheter positionKorean J Pain 2010 23(4):247-53. [Google Scholar]
[10]. Sanchez A, Acuna L, Rocha F, An analysis of the radiological visualization of the catheters placed in the epidural spaceBr J Anaesth 1967 39:485-89. [Google Scholar]
[11]. Hogan Q, Epidural catheter tip position and distribution of injectate evaluated by computed tomographyAnaesthesiology 1999 90(4):964-70. [Google Scholar]
[12]. Afshan G, Chohan U, Khan FA, Chaudhry N, Khan ZE, Khan AA, Appropriate length of epidural catheter in the epidural space for postoperative analgesia: Evaluation by epidurographyAnaesthesia 2011 66(10):913-18. [Google Scholar]