Angiofibromas are rare, benign, but locally aggressive vascular tumours which account for 0.05-0.5% of all head and neck neoplasms. The common variant of angiofibromas of head and neck region is Juvenile Nasopharyngeal Angiofibroma (JNAF) which is well published in the literature. Incidence of Extranasopharygeal Angiofibromas (ENAF) is relatively rare and most of the published literature favours maxillary sinus as the most common site. We report a rare clinical entity of ENAF involving the upper lip which is first of its kind in the light of literature review owing to its anatomical location. The present article not only complements a new location of angiofibroma (in the upper lip) but also concretely reinforces the inclusion of angiofibromas in the spectrum of differential diagnosis of soft tissue lesions pertaining to oral cavity.
Locally aggressive tumour, Upper lip, Vascular tumour
Case Report
A 30-year-old male patient reported to the Department of Oral Medicine and Radiology with a chief complaint of swollen upper lip since two years. History unveiled a trauma two years ago resulting in the loss of his lower front teeth and swollen upper lip for which he didn’t receive any medical attention as the presentations were mildly symptomatic and bearable. Since then the swelling increased in milder proportions which was asymptomatic. Aesthetic concern was the factor which brought him to gain dental consultation. Past medical, family and personal histories remained insignificant.
Soft tissue examination revealed a solitary dome shaped swelling of size 0.8x1.0 cm approximately on the upper lip extending 2 cm away from the right commissure of the mouth reaching philtrum [Table/Fig-1,2]. Superiorly the swelling was at the level of the vermillion border of the lip and inferiorly extending onto the labial mucosa causing obvious clinical disfigurement. The surface over the swelling appeared smooth presenting with bluish tinge and was non-tender and soft in consistency on palpation.
Upper lip showing the swelling.

Upper lip showing the swelling.

Along the side other significant notable findings were Ellis Class IV fracture with tooth no #11, partially edentulous with teeth no #31,41, compromised periodontal health with teeth no #32,42 and mild to moderate generalized stains and calculus [Table/Fig-3].
Intraoral clinical photograph showing Ellis Class IV fracture with tooth no #11, partially edentulous with teeth no I #31,41, compromised periodontal health with teeth no #32,42 and mild to moderate generalized stains and calculus.

Based on the history (trauma two years ago) and clinical findings (lesion presenting with a bluish tinge and is asymptomatic) a working diagnosis was given as mucocele of the upper lip.
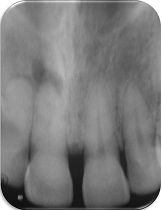
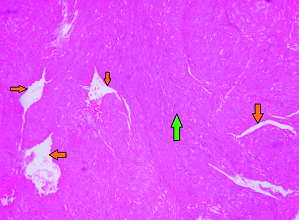
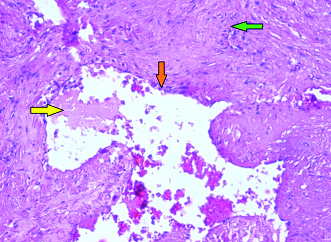
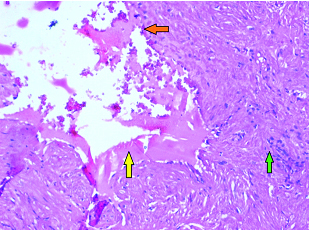
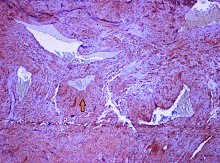
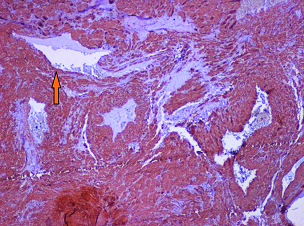
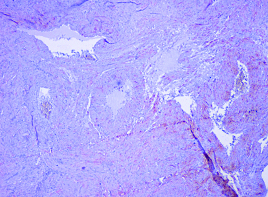
Intraoral periapical radiograph with tooth no #11 was suggestive of chronic periapical abscess [Table/Fig-4]. Excisional biopsy was planned under local anaesthesia after a promising haemogram (haematological parameters were within normal limits) and quadrant scaling was done [Table/Fig-5]. Excised specimen after histopathological examination microscopically revealed [Table/Fig-6,7 and 8] fibrocellular connective tissue stroma with dilated thin walled blood channels lined by endothelium. The blood vessels showed eosinophilic coagulum along with engorged red blood cells. The connective tissue was mature, dense and fibrous with numerous spindle shaped fibroblasts. The mentioned microscopic findings were suggestive of angiofibroma of the upper lip.
Intraoral periapical radiograph showing I periapical abscess with tooth no #11.
Intraoperative session showing excised lesion.

Photomicrograph showing numerous thin walled blood channels (orange arrows) and matured densely fibrous connective tissue with numerous spindle shaped fibroblasts (green arrow) (4X; H&E).
Photomicrograph showing eosinophilic coagulum (yellow arrow), thin walled blood channels (orange arrow) and matured densely fibrous connective tissue with numerous spindle shaped fibroblasts (green arrow) (40X; H&E).
Photomicrograph showing eosinophilic coagulum (yellow arrow), thin walled blood channels (orange arrow), matured densely fibrous connective tissue with numerous spindle shaped fibroblasts indicated by (green arrow) (40X; H&E).
Immunohistochemical staining showed that tumour cells were positive for vimentin, smooth muscle alpha actin [Table/Fig-9,10] and negative for desmin [Table/Fig-11], further reinforcing the diagnosis of angiofibroma.
Immunohistochemical staining showing stromal cells positive for vimentin (orange arrow) (4X).
Immunohistochemical staining showing positivity for smooth muscle alpha actin (orange arrow) (4X).
Immunohistochemical staining showing negativity for desmin (4X).
Patient was followed up at a monthly interval for about one and half year and no recurrence was noticed [Table/Fig-12].
Eighteen months follow up clinical photographs: a) Extraoral view; b) Intraoral view.

Discussion
Angiofibromas predominantly involve the nasopharynx and typically manifest in the younger age groups (early second decade of life) and hence are named as JNAF [1–3]. Windfuhr JP and Remmert S (2004) in their review outlined 65 cases of ENAFs with maxillary sinus as the most common site followed by the ethmoid sinus, nasal cavity, nasal septum, larynx, sphenoid sinus, cheek, conjunctiva, oropharynx, retromolar area, middle turbinate, inferior turbinate and tonsil [4]. Literature also documents the incidence of ENAFs in other rare sites such as external nose, hard palate, external ear, lacrimal sac, carotid bifurcation, oesophagus, trachea, facial nerve, middle cranial fossa and infratemporal fossa [4].
In the present report we have discussed a case of ENAF of the upper lip clinically simulating a mucocele marking rarity with respect to its presentation and extreme rarity with respect to its anatomic location. To the best of our knowledge none of the published literature has portrayed the incidence of ENAF on the upper lip hence forth the present case will highlight this aspect.
ENAF should be considered as a distinct clinical entity because it is different from nasopharyngeal angiofibroma in terms of age, sex and clinical features [1,2]. Some striking distinguishing features of ENAFs are [1,4]: its presentation in adults with an inclination for females whereas, NAF are seen in adolescents with a preponderance for males. ENAF shows less vascularity and more fibrosis components with an infrequent recurrence.
The aetiopathogenesis of angiofibroma remains unclear and is still controversial, although congenital, genetic, hormonal and vascular theories have been proposed [1]. Numerous growth factors like insulin-like growth factor, Vascular Endothelial Growth Factor (VEGF) and Transforming Growth Factor beta (TGF-ß) proposed to play a role in the pathogenesis of tumour [5].
The diagnosis of angiofibroma to a great extent depends on microscopic confirmation because of its close resemblance with other lesions, such as angiomyoma, haemangioma, lymphangioma and haemangiopericytoma [6].
On microscopic examination, angiofibroma is non-encapsulated containing both fibroblastic and vascular components [7]. The diagnosis can be further confirmed using immunohistochemistry (IHC). IHC for angiofibromas reveal positive staining for vimentin, CD34 and alpha actin [1].
In the present case a final diagnosis of angiofibroma was given based on the history of trauma, presence of dilated thin walled blood channels lined by endothelium in a mature, dense, fibrous connective tissue stroma with numerous spindle shaped fibroblasts. IHC findings also supported the diagnosis.
Literature shows that this lesion has close resemblance with other lesions like angiomyoma, haemangioma, lymphangioma and haemangiopericytoma [6]. Angiomyoma can be differentiated from angiofibroma by the presence of proliferation of mesenchymal cells, with eosinophilic cytoplasm and nuclei with a typical cigarlike aspect, and a single layer of endothelial cells lining the vascular spaces [8]. Haemangioma can be differentiated by the presence of marked lobulation and decreased stromal fibrosis [1] whereas, lymphangioma can be differentiated by the presence of marked dilatation of lymphatic vessels and spaces with thin endothelial lining containing proteinaceous fluid and lymphocytes [9]. Haemangiopericytoma can be differentiated by the presence of ‘stag-horn’ sign, formed by proliferation of fusiform to roundish undifferentiated tumour cells in dendritic branches around the capillary vessels [10]. However, solely on microscopic examination we cannot rule out haemangiopericytoma. So, IHC would be a promising diagnostic modality to differentiate haemangiopericytoma and angiofibroma. IHC for haemangiopericytoma reveal positive staining for vimentin and negative staining for CD34 and smooth muscle alpha actin [1].
There are different treatment modalities for angiofibromas which include surgery, hormonal therapy, radiation, and systemic chemotherapy. Nevertheless, surgery remains first choice of treatment [2]. There were no reports regarding the recurrence of ENAF after initial surgery [1,2]. Recurrence rate of JNF is in between 0% and 57% following treatment [5].
Conclusion
Though ENAF is rare, the clinical presentation of it masquerades other commonest lesions (as in the present case), so the inclusion of it in the array of differential diagnosis should be made a point in the evaluation of soft tissue swellings pertaining to the oral cavity.
[1]. Singh GB, Agarwal S, Arora R, Doloi P, Kumar D, A rare case of angiofibroma arising from inferior turbinate in a femaleJ Clin Diagn Res 2016 10(4):7-8. [Google Scholar]
[2]. Rao MS, Lakshmi CR, Sonylal PE, Chakravarthy VK, Murthy PS, Recurrent angiofibroma of ethmoid region-A rare variantJ Clin Diagn Res 2014 8(6):1-2. [Google Scholar]
[3]. Salimov A, Ozer S, A rare location of angiofibroma in the inferior turbinate in young womanInt Arch of Otorhinolaryngol 2015 19(2):187-90. [Google Scholar]
[4]. Windfuhr JP, Remmert S, Extranasopharyngeal angiofibroma: Etiology, incidence and managementActa Otolaryngol 2004 124:880-89. [Google Scholar]
[5]. Pardhe N, Chhibber N, Agarwal D, Jain M, Vijay P, Juvenile nasopharyngeal angiofibroma extending into the oral cavity: A rare entityJ Clin Diagn Res 2015 9(6):31-33. [Google Scholar]
[6]. Thakur RK, Madan E, Tomar A, Arora M, Angiofibroma on cheek mucosa: A rare entity and its management with laserJ Cutan Aesthet Surg 2014 7(4):227-28. [Google Scholar]
[7]. Ewe S, Dayana F, Fadzilah FM, Gendeh BS, Nasal septal angiofibroma in a postmenopausal woman: A rare entityJ Clin Diagn Res 2015 9(12):3-5. [Google Scholar]
[8]. Minni A, De Carlo A, Roukos R, Illuminati G, Cerbelli B, Angioleiomyoma of the oral cavity extended to submandibular space; An unusual tumour in an unusual deep-seated space: A case reportEur Rev Med Pharmacol Sci 2012 16(4):134-37. [Google Scholar]
[9]. Sunil S, Gopakumar D, Sreenivasan BS, Oral lymphangioma-Case reports and review of literatureContemp Clin Dent 2012 3(1):116-18. [Google Scholar]
[10]. Michi Y, Suzuki M, Kurohara K, Harada K, A case of hemangiopericytoma of the soft palate with articulate disorder and dysphagiaInt J Oral Sci 2013 5(2):111-14. [Google Scholar]