Florid osseous dysplasia is a rare benign fibro-osseous multiquadrant dysplastic lesion confined to the alveolar process of jaws, generally asymptomatic and usually detected incidentally during radiologic examination and requires no treatment unless symptomatic or cosmetically concerning. In this article, we present two rare cases of florid osseous dysplasia in Indian women with their clinical, radiographic and histologic findings and a brief review of literature. The first case was asymptomatic and the lesion was detected during routine radiographic examination and required no treatment whereas, the second case presented with features of osteomyelitis. Based on the clinical findings, the case was diagnosed as chronic suppurative osteomyelitis, but, after radiologic examination, diagnosis of florid osseous dysplasia with secondary osteomyelitis was made. Besides diagnostic challenge, management of the lesion is difficult due to poor vascularity. In our case, antibiotic prophylaxis along with surgical debridement and sequestrectomy was done with regular recall visits.
Case-1
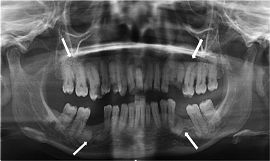
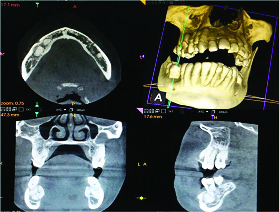
A 50-year-old female patient reported to the Department of Oral Medicine and Radiology with chief complaint of decayed teeth. Medical history was non contributory. On general examination, no abnormality was detected. On intraoral examination multiple decayed teeth and root stumps were present. Teeth were not tender to percussion. Patient was subjected to radiologic examination. Dental panoramic radiograph was taken which revealed radiopaque sclerotic lesions bilaterally in mandibular and maxillary alveolar region in relation to the apices of molar along with hypercementosis of several teeth [Table/Fig-1]. To further delineate, Cone Beam Computed Tomography (CBCT) was performed which showed multiple hyperdense lesions bilaterally in both jaws with no expansion of cortical plates [Table/Fig-2]. Based on the radiographic findings, the case was provisionally diagnosed as florid osseous dysplasia. Routine haematological investigations and biochemical analysis of serum calcium, phosphorus and alkaline phosphatase showed values within normal limits. No other bone involvement was noted. Incisional biopsy was not performed and diagnosis of florid osseous dysplasia was arrived based on its chararacteristic clinico-radiological features of asymptomatic nature and symmetric distribution of lesion confined to alveolar bone with no bony expansion, positive vitality test and normal biochemical analysis. As these lesions do not require surgical removal, conservative management for decayed tooth and extraction of root stumps under antibiotic prophylaxis were planned.
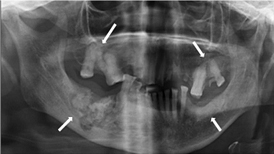
Panoramic radiograph shows radiopaque masses in bilateral maxillary and mandibular molar region with hypercementosis of several teeth.
CBCT axial section of mandible shows hyperdense masses in bilateral molar region. Coronal and sagittal section shows hyperdense masses in relation to apical region of molars confined to alveolar process.
Case-2
A 62-year-old female patient reported to the Department of Oral Medicine and Radiology with the chief complaint of pain and swelling in the right lower jaw for past four months. History revealed that patient had undergone removal of mobile teeth four months before. The pain and swelling did not subside and she also complained of pus discharge from the extraction site. Her past medical history revealed that patient is a known hypertensive.
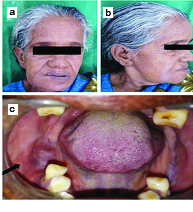
On extraoral examination, there was a localized swelling in right body of mandible approximately 4×3 cm with ill-defined margins, smooth surface and colour of the skin over the swelling appeared normal with no secondary changes. Swelling was tender and hard in consistency [Table/Fig-3a, b].
On intraoral examination, a diffuse swelling in the right buccal aspect of alveolar region in relation to the edentulous mandibular first and second molar region was found [Table/Fig-3c]. Swelling was tender and hard in consistency. On probing, pus discharge from the unhealed socket was noted. Mandibular first and second premolar were non tender to percussion, showed no mobility and was found to be vital. The case was provisionally diagnosed as chronic suppurative osteomyelitis.
a) Extraoral frontal view shows localized swelling in right body of mandible; b) Extraoral lateral view; c) Intraoral view shows swelling in buccal aspect of alveolus in edentulous tooth #46 region.
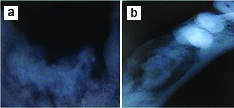
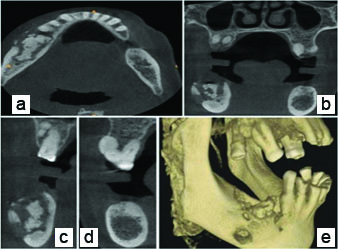
On radiographic examination, a mixed radiopaque radiolucent lesion in the Intra Oral Periapical Radiograph (IOPAR) and expansion of buccal cortex in the occlusal radiograph was noted in the mandibular right molar region [Table/Fig-4a, b]. To further delineate, dental panoramic radiograph and CBCT were taken which revealed a mixed radiopaque radiolucent lesion with ill-defined ragged margins, loss of normal trabecular pattern, presence of irregular central radiopacity suggestive of sequestrum formation and a peripheral radiolucency extending below the alveolar canal of the mandible giving a moth-eaten or worm eaten appearance and disruption of the buccal cortex in first molar region. Radiopaque lesions in bilateral maxillary posterior region and small area of increased density in mandibular left alveolus and hypercementosis of several teeth was also noted [Table/Fig-5,6a-e]. Routine haematological investigations and biochemical analysis showed values within normal limits. No other bone involvement was observed.
a) Intraoral periapical radiograph reveals mixed radiopaque radiolucent lesion and hypercementosis of premolar; b) Cropped mandibular occlusal view reveals expansion of buccal cortex.
Panoramic radiograph reveals mixed radiopaque radiolucent lesion with ill-defined ragged margins, presence of irregular central radiopacity and peripheral radiolucency giving a moth-eaten appearance in right mandibular molar region. Radiopaque lesions in bilateral maxillary and mandibular posterior along with hypercementosis of several teeth.
a) CBCT axial section shows central hyperdense and peripheral hypodense lesion with expansion and disruption of buccal cortex in right mandibular molar region; b-d) Coronal section shows mixed lesion with disruption of buccal cortex in right molar region, hyperdense lesion in bilateral maxillary and left molar; e) 3D reconstruction reveals hyperdense bone in alveolus and loss of buccal cortex in right molar region.
Lesion was surgically excised, sequestrectomy and debridement under local anaesthesia were performed. Specimen consisting of multiple gritty fragments was submitted for histopathological examination [Table/Fig-7a]. Patient was prescribed antibiotics and became asymptomatic after three weeks.
a) Excised surgical specimen showing multiple gritty fragments of tissue; b) Irregular immature trabeculae of woven bone in background of fibrous stroma with chronic inflammatory infiltrate. (H&E stain, 4×).
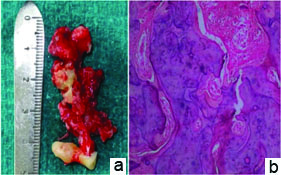
Histopathological finding revealed irregular immature trabeculae of woven bone with plump osteoblast in background of fibrous stroma, which fuse with host bone. In some areas mosaic pattern of bone was seen along with chronic inflammatory infiltrate suggestive of secondarily infected cemento-osseous dysplasia [Table/Fig-7b].
Correlating clinical feature, radiographic findings and histopathologic report, a final diagnosis of florid cemento-osseous dysplasia with secondary osteomyelitis was made.
Postoperative radiograph taken after three months showed satisfactory healing of lesion with bone formation and patient is under regular follow up [Table/Fig-8].
Postoperative panoramic radiograph taken after three months reveals healing of lesion by new bone formation.

Discussion
The term benign fibro-osseous lesion refers to a group of intraosseous lesions in which normal bone is replaced with cellular fibrous connective tissue matrix containing abnormal bone or cementum [1–3]. Cemento-osseous dysplasia belongs to benign fibro-osseous lesions. This term is replaced into osseous dysplasia in the latest WHO classification of odontogenic tumors in 2005 [4]. Osseous dysplasias are strictly localized to the tooth bearing areas of jaws or edentulous alveolar process and not associated with any other skeletal disease [1]. They are categorized into four types as: periapical, focal, florid and familial gigantiform cementoma [3,4].
The term florid cemento-osseous dysplasia was first suggested by Melrose RJ et al., in 1976 to describe the wide spread, extensive manifestations of disease in multiple quadrants of jaws, mostly in mandible with bilateral and often symmetrical presentation [5]. Earlier they were reported as diffuse sclerosing osteomyelitis, sclerotic cemental masses, gigantiform cementoma and multiple enostoses [6].
The exact aetiology and pathogenesis is not known [5,7]. It is assumed that, these lesions originate from elements of periodontal ligament based on the fact that they appear to develop in close relationship to roots of teeth or in periapical region of edentulous parts of jaw and their histological similarity to cementum, suggesting odontogenic origin [8]. The hallmark of maturation in cemento-osseous dysplasia is progressive deposition of cementum-like calcification. This increases the risk of secondary infection due to replacement of normal vascular bone into avascular cementum leading to ischemia of affected tissues [3].
It most commonly occurs in middle aged black females especially in fourth to fifth decade [2,5,7]. The age ranges between 19 to 76 years with female predilection in the ratio of 2.6:1 and racial predilection for blacks, with black:white ratio of 6:1 [6]. Their occurrence in Indian population is rare and very few cases (less than 2%) have been documented in literature [Table/Fig-9] [5,7–22].
Cases of florid osseous dysplasia reported in Indian population [7–22].
| Author | Age/sex | Site | Symptoms | Secondary osteomyelitis |
|---|
| Mangala M et al., [9] | 30/F, 38/F | Bilateral posterior mandible | Present pain, swelling | Absent |
| Jerjes W et al., [7] | 27/F | Bilateral posterior mandible | Absent | Absent |
| Shah V et al., [10] | 37F | Bilateral posterior mandible | Present pain, swelling | Absent |
| Bansal S et al., [11] | 14/M | Bilateral maxilla and mandible | Absent | Absent |
| Asnani U et al., [12] | 63/F | Bilateral posterior maxilla | Present swelling | Absent |
| Premalatha BR et al., [13] | 37/F | Bilateral posterior mandible | Absent | Absent |
| More CB et al., [14] | 60/F | Bilateral maxilla and mandible | Present pain | Absent |
| Mohammed RB et al., [15] | 52/F | Bilateral maxilla and mandible | Present pain, pus discharge (maxilla) | Present |
| Mukherjee J et al., [16] | 42/F | Bilateral posterior mandible | Absent | Absent |
| Das BK et al., [17] | 45/F | Bilateral posterior mandible | Present pain | Absent |
| Grewal HK et al., [8] | 26/M | Bilateral posterior mandible | Present pain, swelling | Absent |
| Shelly A et al., [18] | 64/F | Bilateral maxilla and mandible | Present pain | Absent |
| Mufeed A et al., [19] | 46/F | Bilateral maxilla and mandible | Present pain, pus discharge (maxilla) | Present |
| Kunjir G et al., [20] | 35/F | Bilateral maxilla and mandible | Present swelling | Absent |
| Chhabra N et al., [21] | 50/F | Bilateral maxilla and mandible | Absent | Absent |
| Chattopadhyay J et al., [22] | 41/M | Bilateral maxilla and mandible | Present pain, pus discharge (mandible) | Present |
Clinically, these lesions are most often asymptomatic and discovered incidentally during routine radiographic examination similar to our first case [23]. Few cases are symptomatic and present clinically with jaw swelling, dull pain or sensitivity, purulent discharge and sequestrum formation [2–4,23]. Among the reported cases in India, 11 patients presented with pain or swelling and three patients with pus discharge (two in maxilla and one in mandible) [Table/Fig-9]. Researchers have considered that infections are secondary to the exposure of the cemental masses following resorption of the edentulous alveolus or by extraction of teeth with roots close to the lesions or after biopsy [2,3,24]. In our second case, the secondary infection may be due to consequence of extraction of teeth. Poor vascularity and decreased healing capacity leads to secondary osteomyelitis confusing clinically with primary osteomyelitis [24]. Mohammed RB et al., and Mufeed A et al., reported similar cases with secondary osteomyelitis in maxilla in female patient [15,19] and Chattopadhyay J et al., in mandible in male patient [22] [Table/Fig-9]. Florid osseous dysplasia is not associated with any other extragnathic abnormality or skeletal disease [2] and serum chemistry levels are within normal limits [5,25]. The involved teeth may remain vital [4]. Our cases satisfy these criteria in literature.
Radiographic appearance varies depending on stage of maturation of lesion and present with three patterns. In early stage, lesions often presents with well defined radiolucency at the apices of involved teeth whereas, a mixed radiolucent radiopaque pattern with well defined radiolucent rim is demonstrated in intermediate stages and late stages presents with diffuse radiopacity with ill-defined borders [2]. Root clubbing and hypercementosis may also be present [23,25]. The first case presented with late, whereas, the second case presented with mixed and late radiographic stages. In both cases hypercementosis was noted. The overlying inflammatory process on primary lesion may alter its radiographic features. It has been reported that radiographically true chronic osteomyelitis could appear similar to secondarily infected cemento-osseous dysplasia presenting as moth eaten pattern as our second case [24].
On gross examination, the specimen will be in fragments comprised of multiple tan, brown tissue aggregates and appear crumbly. These centrally important criteria were reiterated by Melrose RJ [5]. Early stages on histological examination show rounded globules similar to cementum or irregular trabeculae of varying size in the cellular fibroblastic stroma. Mature lesions will show fusion of cemental and osseous areas [13,26].
Biopsy is usually not mandatory. As histologically cemento-osseous lesions present with similar findings and the diagnosis of florid osseous dysplasia mainly relies on clinical and radiographic findings only based on its characteristic clinico-radiologic features. [1,7,26]. The present cases satisfy the diagnostic criteria of florid osseous dysplasia.
The following conditions are considered in radiologic differential diagnosis of florid osseous dysplasia due to similar sclerotic appearance [Table/Fig-10] [7,25,26]. Diffuse sclerosing osteomyelitis often presents unilateral, symptomatic and radiopaque part is poorly delineated, without radiolucent margin [25] and affects the basal process of mandible in addition to alveolar process [23]. Gigantiform cementoma shows familial tendency and occur at earlier age with no gender predilection and cause extensive expansion of jaw [25]. Paget’s disease can be easily ruled out based on the involvement of entire jaw and additional bones of the skeleton along with abnormal increase in serum alkaline phosphatase [25].
Differential diagnosis of florid osseous dysplasia [7,25,26].
| Lesion | Predominant Age | Predominant Gender | Predominant Jaw | Predominant Region | Distinguishing Features |
|---|
| Florid osseous dysplasia | Middle age | Female>Male | Mandible | Molar premolar | Usually asymptomatic, Incidental finding, Symmetric multiquadrant distribution, Confined to alveolar bone above inferior alveolar canal Mixed and late stages present with radiolucent rim |
| Focal osseous dysplasia | 3rd to 6th decade | Female>Male | Mandible | Molar premolar | Focal, associated with apical region of tooth or previous extraction site |
| Periapical osseous dysplasia | 3rd to 4th decade | Female>Male | Mandible | Anterior | Vital, asymptomatic, seldom exceed 1 cm |
| Diffuse sclerosing osteomyelitis | Any age mostly adulthood | Male=Female | Mandible | Molar, Ramus, Angle | Unilateral, symptomatic with source of infection, poor or diffuse margins |
| Paget’s disease | Older age | Male>Female | Maxilla | Generalized | Cotton wool appearance, multiple bone involvement, increased serum alkaline phosphatase |
| Gigantiform cementoma | 1st decade | Male=Female | Maxilla and Mandible | Generalized | Familial, autosomal dominant, affected at earlier age, extensive bony expansion and facial asymmetry |
| Fibrous dysplasia | 2nd and 3rd decade | Male=Female | Maxilla>Mandible | Posterior | Asymptomatic, slow expansion, ill defined borders, homogenous ground glass appearance |
| Ossifying fibroma | 3rd to 4th decade | Female>Male | Mandible>Maxilla | Molar premolar | Occur solitary, expansion of jaw, well demarcated, painless |
Florid osseous dysplasia does not require treatment unless infections leading to complications such as osteomyelitis are encountered [4]. The best management for the asymptomatic patients is to prevent the extraction of tooth from periodontal disease and dental caries by regular recall visits with reinforcement of good home oral hygiene care and oral prophylaxis [5,18,21]. In symptomatic patients, due to the avascular nature of the lesion, it may not respond to antibiotics alone and may require surgical debridement and sequestrectomy similar to our second case [3].
Conclusion
Diagnosis of florid osseous dysplasia mainly relies on clinical and radiological findings alone. As biopsy, surgical intervention or extraction of teeth may lead to risk of infection such as secondary osteomyelitis, this lesion has to be differentiated from other similar lesions and every effort must be made to preserve the natural dentition. Long term follow up with annual radiographic examination should be carried out.
[1]. White SC, Pharoah M, Oral Radiology: Principles and Interpretation 2009 6th edSt. LouisMosby [Google Scholar]
[2]. Eversole R, Su L, El Mofty S, Benign fibro-osseous lesions of the craniofacial complex a reviewHead Neck Pathol 2008 2(3):177-202. [Google Scholar]
[3]. Alsufyani NA, Lam WN, Osseous (cemento-osseous) dysplasia of the jaws: Clinical and radiographic analysisJ Can Dent Assoc 2011 :77-70. [Google Scholar]
[4]. Barnes L, Eveson JW, Reichart P, Sidransky D, Pathology and genetics of head and neck tumoursWorld Health Organization Classification of Tumours 2005 LyonIARC Press:323 [Google Scholar]
[5]. Melrose RJ, Abrams AM, Mills BG, “Florid osseous dysplasia. A clinical pathologic study of thirty four cases,”Oral Surgery Oral Medicine and Oral Pathology 1976 41:62-82. [Google Scholar]
[6]. Peter AR, Philipsen HA, Odontogenic tumors and allied lesions 2004 1st edLondonQuintessence [Google Scholar]
[7]. Jerjes W, Banu B, Swinson B, Hopper C, Florid cemento-osseous dysplasia in a young Indian women. A case reportBr Dent J 2005 198(8):477-78. [Google Scholar]
[8]. Grewal HK, Goel P, Batra R, Chopra S, A tender swelling of the left posterior mandible: An unusual caseJ Oral Maxillofac Pathol 2014 18:332 [Google Scholar]
[9]. Mangala M, Ramesh DN, Surekha PS, Santosh P, Florid cemento osseous dysplasia: Review and report of two casesIndian J Dent Res 2006 17:131-34. [Google Scholar]
[10]. Shah V, Soni N, Manjunatha BS, Kumar S, Florid cementoosseous dysplasia— An unusual entity. A case reportJ Oral Maxillofac Pathol 2011 2(2):161-64. [Google Scholar]
[11]. Bansal S, Shetty S, Bablani D, Kulkarni S, Kumar V, Desai R, Florid osseous dysplasiaJ Oral Maxillofac Pathol 2011 15:197-200. [Google Scholar]
[12]. Asnani U, Galinde JS, Natrajan S, Sonar M, Florid cemento osseous dysplasiaJ Contemp Dent 2012 2:53-56. [Google Scholar]
[13]. Premalatha BR, Patil SG, Rao RS, Jude J, Florid cemento-oseous dysplasia-A dilemma to intervene or notInt Journal of Clinical Dental Science 2012 3:106-11. [Google Scholar]
[14]. More CB, Shirolkar R, Adalja C, Tailor MN, Florid cement-osseous dysplasia of maxilla and mandible: A rare clinical caseBraz J Oral Sci 2012 11(4):513-17. [Google Scholar]
[15]. Mohammed RB, Kumar YP, Pattipati S, Pakki SK, Florid cemento-osseous dysplasia complicated by chronic diffuse osteomyelitis in the maxillaJ Stomat Occ Med 2013 6:38-41. [Google Scholar]
[16]. Mukherjee J, Purandare B, Dolare C, Pokle M, A case report of florid cemento osseous dysplasiaInternational J of Healthcare & Biomedical Research 2013 1(4):335-39. [Google Scholar]
[17]. Das BK, Das SN, Gupta A, Nayak S, Florid cemento-osseous dysplasiaJ Oral Maxillofac Pathol 2013 17(1):150 [Google Scholar]
[18]. Shelly A, Aadithya BU, Sunita G, Nitika B, Nisha J, Florid cemento-osseous dysplasia – A case reportMalaysian Dental Journal 2014 36(1):10-13. [Google Scholar]
[19]. Mufeed A, Mangalath U, George A, Hafiz A, Infected florid osseous dysplasia: Clinical and imaging follow-upBMJ Case Rep 2015 2015:iibcr2014209099 [Google Scholar]
[20]. Kunjir G, Kumar RK, Uppalwar P, Florid cemento-osseous dysplasiaIJSS Case Reports & Reviews 2016 2(10):16-19. [Google Scholar]
[21]. Chhabra N, Chhabra A, The diagnostic dilemma of multiquadrant nonexpansile fibro cemento osseous lesion: A case reportInt J Clin Prev Dent 2016 12(2):111-14. [Google Scholar]
[22]. Chattopadhyay J, Ghanta S, Florid cemento-osseous dysplasia with multiple impacted supernumerary teeth in maxilla and mandible – A case reportInternational Journal of Contemporary Medical Research 2016 3(8):2198-200. [Google Scholar]
[23]. MacDonald Jankowski DS, Florid cemento-osseous dysplasia: A systematic reviewDentomaxillofac Radiol 2003 32:141-9. [Google Scholar]
[24]. MacDonald Jankowski DS, Focal cemento-osseous dysplasia: A systematic reviewDentomaxillofac Radiol 2008 37:350-60. [Google Scholar]
[25]. Wood NK, Goaz PW, Differential diagnosis of oral and maxillofacial lesions 2015 5th edMosby-Year Book, Inc [Google Scholar]
[26]. Neville BW, Damm DD, Allen CM, Bouquot JE, Oral and Maxillofacial Pathology 2009 3rd edSt.Louis, MissouriSaunders Elsevier [Google Scholar]