Gingival displacement procedure is an important component of fixed prosthodontics. It helps in delivery of the impression material subgingivally to record the finish line as well as the tooth contour apical to it, so as to produce restorations with closely adapted margins in harmony with the tooth anatomy and gingiva. While displacing gingiva with retraction cords, the health of the tissues must be maintained. In case of multiple anterior tooth preparations with close root proximity, placing the retraction cord simultaneously around all teeth will result in strangulation of interdental papillae. This can impair gingival health as well as cause black inter-dental triangles. To avoid this, ‘every other tooth’ technique of gingival displacement in combination with sectional impressions may be used to provide a better master cast in multiple tooth preparations. The present case report describes the use of this simple combination procedure for the restoration of lower six anterior teeth as a part of full mouth rehabilitation.
Case Report
The case report intends to present a combination technique used to restore lower six anterior teeth that was done as a part of full mouth rehabilitation.
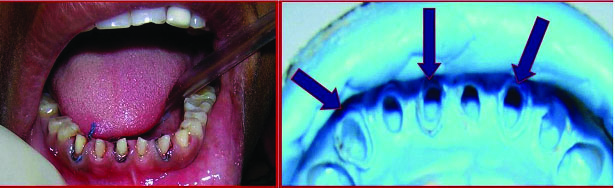
A 25-year-old female patient [Table/Fig-1] reported to Department of Prosthodontics for replacement of missing teeth and complained of flat teeth and difficulty in chewing food. Intraoral examination revealed missing right mandibular first molar, severe attrition of the posterior teeth, flattening of canine tips, attrition of mandibular incisors, collapse of bite, temporomandibular joint click and overjet was 6 mm with a 5 mm overbite. There was no traumatic occlusion with respect to anterior teeth. The case was taken up for full mouth rehabilitation. A bite raising appliance was given to raise the bite by 3 mm. After a four month watch period of assessing patient acceptability and compliance, it was decided to start full mouth rehabilitation by first restoring the lower anterior teeth. Orthopantomograph (OPG) and full mouth Intra Oral Periapical Radiograph (IOPAR) revealed regressed pulp chambers and eliminated the need for root canal treatment. The clinical crown height of mandibular anterior teeth was less with attrition of incisors and considerable flattening of canines [Table/Fig-2]. Full crowns were planned as they are stronger; provide good retention, better durability and aesthetics as compared to partial crowns and composite restoration.

Pre-operative intraoral view of mandibular anteriors.

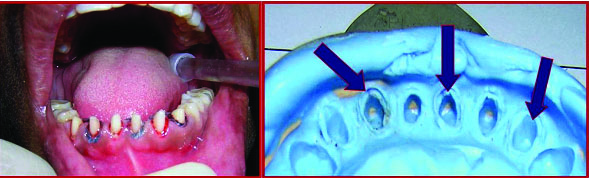
Tooth Preparation: As bite was raised [Table/Fig-3] there was no need of reducing the incisal surfaces. All the axial surfaces of teeth #33, 32, 31, 41, 42, 43 were reduced by 1.5 mm with a distinct shoulder margin. As gingival sulci were shallow, equi-gingival margins were planned. Incisally, a functional cusp bevel was placed on the labio-incisal line angle. [Table/Fig-4] shows tooth preparations of lower six anterior teeth.

Teeth preparations with respect to teeth #31,32,33,41,42,43.

Gingival Displacement and Impression Making: Considering the root proximity with lower anterior teeth and to avoid strangulation of inter dental papillae, it was decided not to displace gingiva of all adjacent teeth at the same time. The ‘every other tooth’ technique was adopted. Gingival displacement of three alternate teeth was done followed by a sectional impression of the anterior segment. Two sectional impressions were required. Two custom sectional trays with a spacer thickness of two wax sheets and tissue stops on occlusal surfaces of teeth #34,44 were prepared. The trays were customized to cover mandibular teeth from tooth #34 to 44. A full arch custom special tray with two wax sheet spacer thickness and four tissue stops (on teeth #34,44,37,47) was made.
Gingival displacement of teeth #33,31,42 followed by corresponding sectional impression was made [Table/Fig-5]. Later, gingival displacement of teeth #32,41,43 followed by corresponding sectional impression was made [Table/Fig-6]. Finally, a full arch impression without gingival displacement was made and kept aside [Table/Fig-7]. All the impressions were made using medium viscosity addition silicone impression material. Temporization was done and patient was recalled.
Gingival displacement in relation to teeth #43,41,32 and corresponding sectional impression.
Gingival displacement in relation to teeth #42,31,33 and corresponding sectional impression.

Master Cast and Die Preparation: The two sectional impressions were poured in die stone and the corresponding six dies for teeth #33,32,31,41,42,43 were prepared. The obtained dies were positioned in their respective places in the full arch impression and stabilized [Table/Fig-8]. This full arch impression with wax stabilized dies was poured in die stone to obtain the master cast [Table/Fig-9].
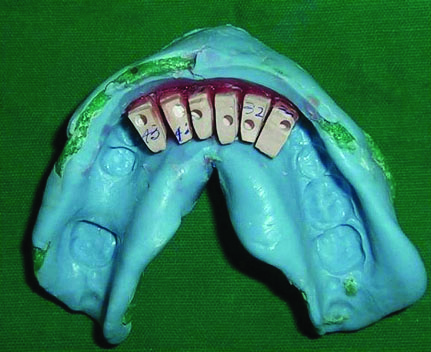
Master cast with dies coated with die spacer for ceramic crowns.

Fabrication of Crowns: From the master cast, six refractory dies were prepared over which glass infiltrated copings were fabricated. Try in of copings was done [Table/Fig-10]. Later, they were layered and fired for In-Ceram spinell (magnesium aluminium oxide) all ceramic crowns. [Table/Fig-11] shows final cemented restorations. Space closure with crowns was also judged using mock wax up models; this required larger crowns mesiodistally and the emergence profile created was too bulky and could lead to food lodgement. It was decided to maintain the anterior diastemas as they would be self cleansing. Moreover, lower anterior teeth were not visible when the patient smiled and so there was no aesthetic compromise. [Table/Fig-12] shows restored lower anterior teeth six months later along with the completed posterior restorations.
Try in of copings on master cast and in mouth.
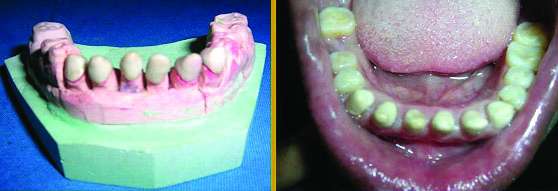
Final all ceramic restorations in relation to lower six anterior teeth. (left)

Lower anterior restorations six months later. Note the completion of posterior restorations. (right)

The remaining posterior and missing teeth were restored and the full mouth rehabilitation was completed at a later date. As the presented technique was applied only with respect to lower anteriors and not with other teeth, the description is restricted to the lower anteriors.
Discussion
This case report presents an alternate tooth/every other tooth gingival displacement procedure in combination with two sectional impressions to produce a better master cast.
Biologic width is the dimension that healthy gingival tissues occupy above the alveolar bone crest. It is detrimental to the periodontal health and all restorative procedures must be carried out in harmony with the same [1]. According to Holmes HM, the term gingival displacement is more appropriate than gingival retraction while describing soft tissue management procedure in fixed prosthodontics [2]. Long term health and stability of periodontal structures determines the success of fixed prosthodontic restorations [3].
The objective of gingival displacement is to reversibly displace gingiva in a lateral direction so that a bulk of low viscosity hydrophobic impression material is introduced into the intracrevicular space. A critical sulcular width of 0.2 mm is required to register accurate margin detail and for sufficient strength of impression material [4,5].
Maintaining the normal appearance and health of gingiva is the ultimate goal of tissue management. This means that gingiva must be healthy before treatment and there must be minimal trauma during treatment [6,7].
The criteria for gingival displacement and retraction material used include effective displacement, haemostasis, no damage to gingiva and minimal systemic effects [8]. While gingiva is being displaced, it is subjected to retraction, relapse, displacement and collapse. However, the periodontal ligament fibres around the teeth provide good support and minimize collapse of the gingival tissues, once the retraction agent is removed [9,10]. Simultaneous gingival displacement around adjacent teeth with close root proximity can strain and strangulate the inter-dental papillae causing papillary recession and large black triangular gingival embrasures and this can be prevented by every other tooth technique [11].
Over years, many impression procedures [9,10,12] and techniques of gingival displacement [6,13] have been made available. The choice of technique depends on case presentation, requirement, operator preference and patient acceptance. In this case, because of the close root proximity between the teeth, gingival displacement of all adjacent teeth was not done together, but alternate tooth gingival displacement was done. One full arch impression was made without gingival displacement. Two sectional impressions of only the anterior segment were made after every other tooth gingival displacement. A sectional impression is a negative likeness made in sections [14]. The presented technique required two extra impressions in contrast to just one, however, a master cast with well defined finish lines was obtained [Table/Fig-7].
Bhansali S et al., and others have used and recommended this technique as a procedure for preserving interdental papilla [15]. Literature suggests that this technique is beneficial for gingival health while restoring multiple teeth especially the lower anterior teeth [11].
Patient was very co-operative all through the restorative procedures and was very happy with the final restorations. She was motivated for further treatment. Once the lower anterior restorations were completed, further restoration of posterior teeth as well as replacement of missing teeth was done incrementally.
Conclusion
This case report presents a combination technique of impression making and soft tissue management while restoring multiple anterior teeth. The technique is easy, simple to use and provides a master cast with well defined finish lines and can be used while restoring multiple teeth with close root proximity.
Declaration: A paper presentation describing this combination technique was done by the author in the eighth National Convention of Postgraduate Students of Indian Prosthodontic Society at Mahatma Gandhi Institute of Dental Sciences, Puducherry, India, held 23-25 June 2006. The paper was titled, ‘Combination of Sectional Impressions and Every Other Tooth Gingival Displacement- A simple Solution for a Better Master Cast in Multiple Tooth Preparations- A Clinical Report’.
[1]. Carranza FA, Newmann MG, Clinical Periodontology 1996 8th editionPhiladelphiaWB Saunders:723-24. [Google Scholar]
[2]. Holmes HM, Gingival displacement not retractionDent Surv 1968 44(12):35-36. [Google Scholar]
[3]. Ferencz JL, Maintaining and enhancing gingival architecture in fixed prosthodonticsJ Prosthet Dent 1991 65:650-57. [Google Scholar]
[4]. Laufer BZ, Baharav H, Cardash HS, The linear accuracy of impressions and stone dies as affected by the thickness of the impression marginInt J Prosthodont 1994 7:247-52. [Google Scholar]
[5]. Prasad KD, Hegde C, Agarwal G, Shetty M, Gingival displacement in prosthodontics. A critical review of existing methodsJ Interdisciplinary Dent 2011 1(2):80-86. [Google Scholar]
[6]. Baba NZ, Goodacre CJ, Jekki R, Won J, Gingival displacement for impression making in fixed prosthodontics, contemporary principles, materials and techniquesDent Clin North Am 2014 58(1):45-68. [Google Scholar]
[7]. Rosensteil SF, Land MF, Fujimoto J, Contemporary Fixed Prosthodontics 1995 2nd editionSt. Louismosby:305 [Google Scholar]
[8]. Schillingberg HT, Hobo S, Whitsett LD, Jacobi R, Brackett SE, Fundamentals of Fixed Prosthodontics 1997 3rd edILQuintessence:261 [Google Scholar]
[9]. Livaditis GJ, The matrix impression system for fixed prosthodonticsJ Prosthet Dent 1998 79:208-16. [Google Scholar]
[10]. Livaditis GJ, Comparison of new matrix system with traditional fixed prosthodontic impression proceduresJ Prosthet Dent 1998 79:200-07. [Google Scholar]
[11]. Donovan TE, Chee WW, Current concepts in gingival displacementDent Clin North Am 2004 48:433-44. [Google Scholar]
[12]. Donovan TE, Chee WW, A review of contemporary impression materials and techniquesDent Clin North Am 2004 48(2):445-70. [Google Scholar]
[13]. Khajuria R, Madan R, Sharma V, Singh R, Gingival dilation- A boon in fixed prosthodonticsAnnals of Dental Specialty 2014 2(4):129-33. [Google Scholar]
[14]. The Glossary of Prosthodontic TermsJ Prosthet Dent 2005 94:61-62. [Google Scholar]
[15]. Bhansali S, Bhansali N, Singh K, Agarwal B, An impression technique for preserving interdental papillaeJ Indian Prosthodont Soc 2010 10(4):226-29. [Google Scholar]