A Fortuitous Turn of Evidence in an Elderly Female – A Case of Pulmonary Fusariosis
Saraswathy Sreeram1, Flora Dorothy Lobo2, Vishak Acharya3, Vishwas Saralaya4
1 Assistant Professor, Department of Pathology, Manipal University, Mangaluru, Karnataka, India.
2 Professor, Department of Pathology, Manipal University, Mangaluru, Karnataka, India.
3 Professor and Head of the Department, Department of Pulmonary Medicine, Manipal University, Mangaluru, Karnataka, India.
4 Associate Professor, Department of Microbiology, Manipal University, Mangaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Saraswathy Sreeram, Kasturba Medical College, Lighthouse Hill Road, Hampankatta, Mangaluru-575001, Karnataka, India.
E-mail: swameeram@gmail.com
Pulmonary mycosis is seen infrequently in our country. It is more common in the immunocompromised. The infections caused by less known species like Fusarium have been found to be increasing in incidence in other parts of the world. We hereby report its occurrence in a 79-year-old, non-immunocompromised female who presented with pyrexia of unknown origin. Her Alanine Phosphatase (ALP) and Lactate Dehydrogenase (LHD) levels were raised. CT scan showed interstitial thickening in subpleural aspect of lungs and multiple enlarged lymph nodes in mediastinum. Liver showed multiple hypodense lesions. Metastasis was suspected for which Fine Needle Aspiration Cytology (FNAC) of liver was done which showed foci of regenerative hepatocytes with desmoplastic stromal tissue fragments and negative for tumour. Her Alpha Fetoprotein (AFP) was normal. The bronchial tree cytology showed endobronchial cells, dust-laden macrophages and chronic inflammatory cells along with fungi on Pap smear studies. This was confirmed by culture that grew Fusarium species. after one week of incubation. The acutely branching septate hyphae of Fusarium species are identical to those of Aspergillus species. In a patient who has a disseminated infection with a septate fungus, growth in culture is important to identify the specific organism and subsequently treatment with appropriate antifungals. In cases like ours, where the infection simulates malignancy, it is even more important to make the correct diagnosis to give the appropriate treatment.
Cytology, Filamentous fungi, Fusarium, Immunocompetent, Lung cancer
Case Report
A 79-year-old female presented to the emergency department with chief complaints of on and off high grade fever associated with chills and rigors and cough with expectoration since 2 months. She had a history of hypertension and ischemic heart disease since 30 years and was on treatment. She had undergone cholecystectomy 2 years ago. At admission, her blood pressure was low (90/60 mm Hg). No other abnormalities were detected in the systemic examination.
Her blood investigations showed low Haemoglobin of 8.7 g/dL and a raised Erythrocyte Sedimentation Rate (ESR) of 100 mm/hr. Peripheral smear was reported as normocytic normochromic anaemia. Her liver function tests showed a decrease in both total protein-5.8 g/dl and Albumin-2.9 g/dl and a rise in Alkaline Phosphatase (ALP-309 IU/L). Her renal function tests, Thyroid Stimulating Hormone (TSH) and urine analysis were normal. Both Rheumatoid Factor and test for malarial parasite were negative. Her Fasting Blood Sugar (FBS-107 mg/dL) and Gamma Glutamyl Transpeptidase (GGT-103.2 IU/l) were high. Sputum culture & sensitivity showed a scanty growth of Klebsiella species which was sensitive to all the antibiotics routinely used for the species. Lactate Dehydrogenase (LDH) level was also high (918 IU/L). Alpha Fetoprotein (AFP) level was normal (2.19 IU/l).
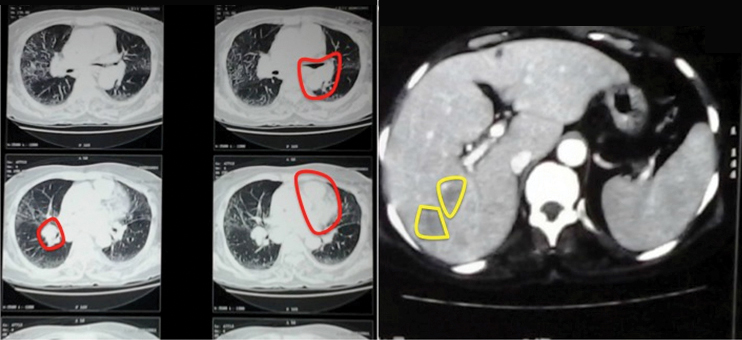
CT scan showed interstitial thickening in subpleural aspect of both lungs and multiple enlarged lymph nodes in mediastinum [Table/Fig-1]. Segments VI, VII and VIII of liver showed multiple hypodense lesions, largest measuring 6.6 x 5.1 cm [Table/Fig-1]. With these findings, a differential of lymphoma was considered.
CT scan – Lungs show subpleural thickening with enlarged mediastinal lymph nodes (left – red markings). Liver shows multiple hypodense lesions (Right – yellow markings).
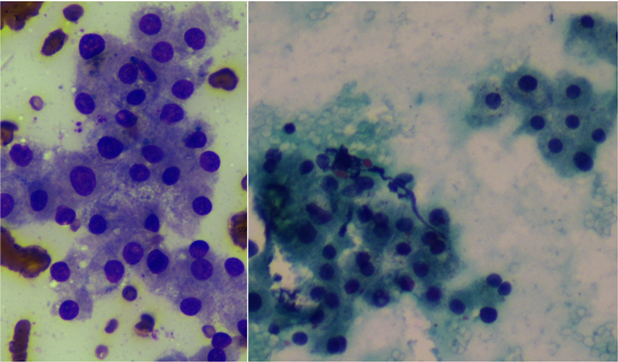
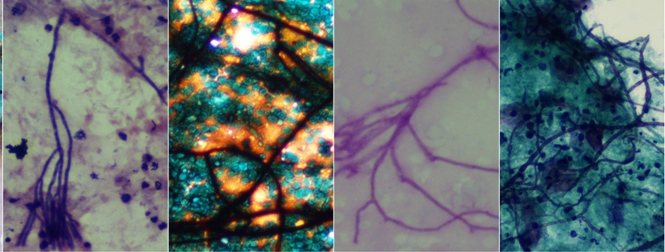
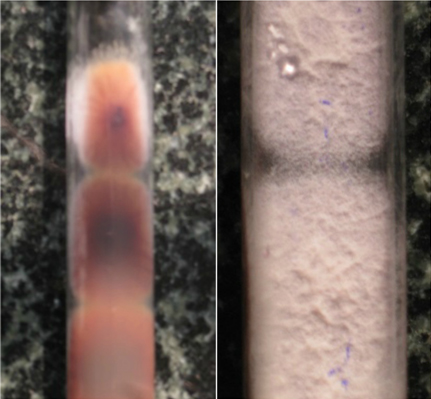
USG guided FNAC liver was done. It showed foci of regenerative hepatocytes with fibrous stromal tissue fragments and was negative for malignancy [Table/Fig-2]. Broncho Alveolar Lavage (BAL) and brush sent for cytology showed some endobronchial cells in clusters or singly scattered along with dust laden macrophages and few benign squamous epithelial cells. Background showed acute and chronic inflammatory cells. Endobronchial cell nuclei showed reactive changes. Acutely and right angle branching septate fungal hyphae were seen on Pap smear studies [Table/Fig-3]. A possibility of Aspergillosis was considered due to the above morphology. Slides were reported as negative for malignant cells with the presence of fungal hyphae. Special stains like Periodic Acid Schiff (PAS) and Gomori’s Methenamine Silver (GMS) were done to confirm the presence of fungi. Culture reports confirmed the growth of fungi of Fusarium species after one week of incubation [Table/Fig-4].
FNAC liver showing regenerative changes in hepatocytes: a) Cellular and nuclear enlargement, (May Grunwald Giemsa stain;40X); b) Binucleation and normal chromatin pattern (Pap stain; 20X).
BAL cytology showing septate fungal hyphae (from left: H&E, Gomori’s Methenamine Silver, Periodic Acid Schiff, Papanicolaou; 40X).
Fungal culture on dextrose agar yielded yellowish brown (left) to characteristic white powdery colonies (right) of Fusarium.
The patient was treated with combination of antifungals and was discharged from hospital after symptomatic improvement. On follow up after a month, the patient had recovered completely from the infection.
Discussion
Fusarium is a pervasive plant pathogen which has been known to cause severe disseminated infection in immunocompromised patients. There are two major routes of infection with Fusarium: sino-pulmonary route (more common) and the skin, in the setting of catheters [1]. Infections in non-immunocompromised patients are usually direct and localized [2]. This case is of a 70-year-old non-immunocompromised lady with predominantly pulmonary involvement mimicking a malignancy.
The major features of lung cancer on radiology are a parenchymal mass with irregular borders, lobulations, cavitation and infiltration of chest wall. However, many infectious diseases closely resemble malignancy on imaging, making them virtually indistinguishable. Some known examples of such infectious agents are Histoplasma, Cryptococcus, Aspergillus, Mucor, Blastomyces and Paracoccidiodes [3].
The radiological appearance of Fusarium infection in lung can vary from non specific infiltrates to cavitatory or nodular lesions. In our case, the CT scan showed interstitial thickening predominantly in the subpleural aspect of bilateral lungs which gave an impression of an interstitial lung disease or lymphangitis carcinomatosa. Multiple enlarged lymph nodes were seen in the mediastinum suspected to be secondaries or of tuberculous aetiology. The correct diagnosis in such cases requires correlation with clinical details and laboratory investigations. Lung involvement has been reported in all cases of disseminated fusariosis and the prognosis is directly related to the patient’s immune status [4].
Fusarium has been reported to be an emerging infection in patients with hematological malignancies [5]. Fusarium solani is the most frequent and virulent species isolated. It has been found to be an emerging opportunistic infection mostly after bone marrow transplantations. Reports of Fusarium infection in Indian literature, however, are scant [6]. Co-existence of lung cancer with Fusarium infection has also not been reported.
Fusariosis closely resembles Aspergillosis in numerous ways. The similarities include the sino-pulmonary route of entry, radiological appearance, morphology, and tendency for vascular invasion, high rate of mortality, relapse and occurrence after bone marrow transplantation. However, Fusariosis, unlike Aspergillosis, often shows a traumatic route of entry, presentation with metastatic skin lesions (60-70%), 50-70% positivity in blood culture and resistance to antifungals [5].
A clinical workup of Fusarium infection includes eliciting a history of trauma, onychomycosis, spider bite or an immunocompromised state. Physical examination often reveals skin lesions that present as nodular and subcutaneous that can progress to even cellulitis. Endophthalmitis has also been reported in many cases. Diagnostic workup includes imaging study of the lungs, bone scan and cultures of BAL, blood, swab or biopsy, as indicated. They form multicellular banana-shaped macroconidia with a basally placed foot cell [5].
A lung biopsy showing the presence of hyphae with adventitious sporulation is vital in such cases to make the diagnosis of Fusarium infection and to rule out the possibility of contamination. The acutely branching septate hyphae of Fusarium spp are identical to those of Aspergillus species. Recently methods like In Situ Hybridization (ISH) with Peptide Nucleic Acid (PNA) probes in paraffin embedded sections have been identified as valuable tools in accurate identification of Fusarium species. from fungi with identical morphology [7].
Conclusion
Unique features of this case were presentation of Fusarium infection in a non-immunocompromised elderly female mimicking a malignancy. Correct diagnosis becomes important in such cases to avoid the anxiety and panic associated with a possibility of malignancy. Early identification of less known fungi like Fusarium is also important due to its resistance to routine antifungals, often requiring combination therapy, as in our case.
[1]. Muhammed M, Feldmesser M, Shubitz LF, Lionakis MS, Sil A, Wang Y, Mouse models for the study of fungal pneumoniaLandes Bioscience 2012 3(3):329-38. [Google Scholar]
[2]. Smith JA, Kauffman CA, Pulmonary fungal infectionsRespirology 2012 17:913-26. [Google Scholar]
[3]. Gazzoni FF, Severo LC, Marchiori E, Irion KL, Guimaraes MD, Godoy MC, Fungal diseases mimicking lung cancer: Radiological pathological correlationMycoses 2014 57(4):197-20.September doi 10.1111/myc.12150 [Google Scholar]
[4]. Carneiro HA, Coleman JJ, Restrepo A, Mylonakis E, Fusarium infection in lung transplant patientsMedicine (Baltimore) 2011 90(1):69-80. [Google Scholar]
[5]. Boutati EI, Anaissie EJ, Fusarium, a Significant Emerging Pathogen in Patients With Hematologic Malignancy: Ten Years’ Experience at a Cancer Center and Implications for ManagementBlood 1997 90(3):999-1008. [Google Scholar]
[6]. Madhavan M, Ratnakar C, Veliath AJ, Kanungo R, Robinson SS, Bhat S, Primary disseminated fusarial infectionPostgrad Med J 1992 68:143-44. [Google Scholar]
[7]. Shinozaki M, Okubo Y, Sasai D, Nakayama H, Murayama SY, Ide T, Identification of Fusarium species in formalin-fixed and paraffin-embedded sections by in situ hybridization using peptic nucleic acid probesJ Clin Microbiol 2011 49(3):808-13. [Google Scholar]