Molluscum Contagiosum of Cervix – A Case Report
Ankita Bagel1, Kalyani Raju2, Munikrishna Munisamaiah3, Bachu Narayanaswamy Raghavendra Prasad4
1 Resident, Department of Pathology, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Kolar, Karnataka. India.
2 Professor, Department of Pathology, Sri Devaraj Urs Medical College, Kolar, Karnataka, India.
3 Professor and Head, Department of OBG, Sri Devaraj Urs Medical College, Kolar, Karnataka, India.
4 Professor, Department of Medicine, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Kolar, Karnataka. India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kalyani Raju, Professor of Pathology, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Kolar-563102, Karnataka, India.
E-mail: drkalyanir@rediffmail.com
Molluscum Contagiosum (MC) is a common viral infection of skin caused by a double stranded DNA Pox virus affecting both adults and children. MC is primarily an infection of school-going children (one to five years), occasionally it affects adults and immunocompromised individuals. Transmission of virus occurs by direct contact with infected persons or contaminated objects. Most common sites are skin of face, trunk and extremities in children, genitals in adults and rarely palms, soles and mucous membranes. The occurrence of MC in genitals is lowest (3%). We present a case report of Molluscum Contagiosum of cervix which is a rare site; only one case has been reported in medical literature till date.
Female genital tract, Viral, Skin
Case Report
A 60-year-old female presented to medicine OPD for Obstructive Uropathy features since three weeks. Following systemic and local examination, foul smelling discharge per vagina was observed for which patient was referred to OBG Department. On per speculum examination, a firm reddish nodule was seen on the posterior lip of cervix with white discharge over and around it. A provisional clinical diagnosis of viral infection of cervix was considered. Cervical biopsy was taken and sent for histopathological examination. Past history revealed that the patient had undergone 2 rounds for haemodialysis for obstructive Uropathy. No other lesions were present elsewhere on the body. HIV status was negative.
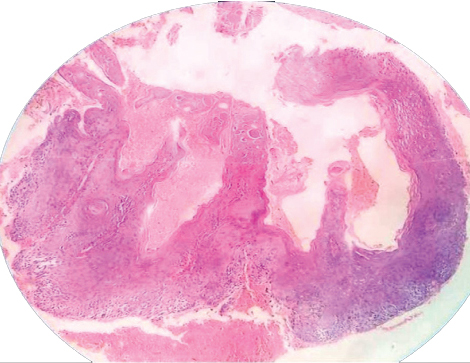
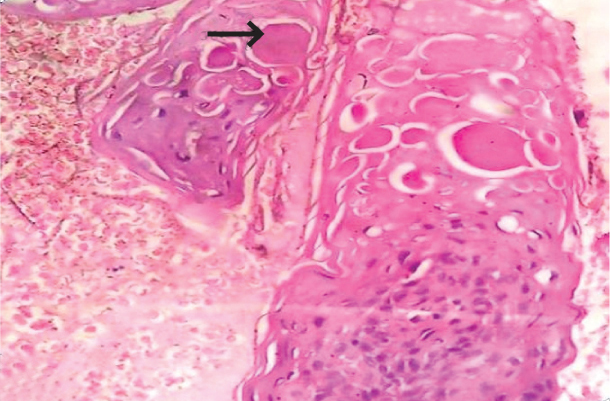
Grossly, the specimen consisted of a tiny grey-white to grey-brown soft tissue bit measuring around 0.5 cm across with mucosal surface on one side. No bullae were identified. Microscopy showed stratified squamous epithelium with focal hyperplastic changes. Focal area showed a cup shaped lesion consisting of proliferating keratinocytes having eosinophilic cytoplasmic inclusions with features of hyperkeratosis [Table/Fig-1,2]. Correlating with case history and clinical findings, histopathological diagnosis of Molluscum Contagiosum (MC) of cervix was given.
Microphotograph showing stratified squamous epithelium with cup like lesion (H&E, 10X).
Microphotograph showing proliferating keratinocytes consisting of intracytoplasmic eosinophilic inclusions (arrow) (H&E, 40X).
During the patient’s hospital stay, she was catheterized and 2 cycles of haemodialysis were done. For the cervical lesion only follow up was advised. When patient was symptomatically better, she was discharged and advised a weekly follow up weekly for which the patient did not turn up.
Discussion
Molluscum Contagiosum (MC) is a common skin viral infection caused by a double stranded DNA Pox virus affecting both adults and children. MC is primarily an infection of school-going children (1-5 years) and occasionally adults and immunocompromised individuals [1,2]. MC occurs in 2%-10% of worldwide population, its incidence increases in immunocompromised individuals like HIV infected, increasing upto 5%-18% [3]. In the present case, the patient was 60 years old female.
In medical literature, MC was first described in 1817 and its viral aetiology was determined by Juliusberg. It is known to be of Poxviridae family [4,5]. The virus is round or rectangular consisting of linear double stranded DNA [2]. This virus infects epidermal keratinocytes [6]. It utilizes microtubule cytoskeleton of eukaryotic cells for movement leading to continuous spread of virus infection [7,8].
There are 4 strains of MC virus (MCV) [1–3]. MCV 1 is most common overall and worldwide and also affects young children most commonly. MCV-2 mainly infects immunocompromised individuals especially HIV positive individuals. Transmission of virus occurs by direct contact with infected persons or contaminated objects (fomites) like towels, sponges, swimming pools, tattoo instruments, instruments at beauty salons, etc., [9]. Most common sites are skin of face, trunk and extremities in children, genitals in adults and rarely palms, soles and mucous membranes [1]. Occurrence of MC in genital areas is lowest, approximately 3% [3]. Molluscum Contagiosum of the cervix is very rare and as far as our knowledge goes, only one case is reported in English scientific literature till date [10]. In the present case, the risk factors are repeated haemodialysis, catheterisation and probably immunosuppression.
Clinically, they appear as firm, flesh coloured doughnut or umbilical shaped lesion, about 2-5 mm in diameter, centre usually filled with white curdy type material. It can also present as giant MC (>5 mm), eczematous lesions and folliculocentric lesions which can closely mimic conditions like Condyloma acuminatum, Basal cell carcinoma and Lymphangioma. With atypical presentation, it becomes a diagnostic challenge specially in HIV I positive individuals and immunosuppressed patients [1,10]. In present case, the lesion presented as reddish nodule with white discharge.
Usually clinical features are typical and histomorphological features on light microscopy are classical, which confirms the diagnosis. Hence, other molecular investigations are not done. The histomorphological features are; the dermis is indented by a sharply delimited and lobulated mass of proliferating epithelium. As the cells differentiate within the mass, their cytoplasm gradually is filled by a faintly granular eosinophilic inclusion that displaces the nucleus and enlarges the cells. These molluscum bodies are formed of viral particles that are similar in size and mode of formation to the poxviruses. Inflammation in the surrounding dermis is intense, sometimes in the form of an abscess and sometimes in the form of a pleomorphic T-cell infiltrate that can simulate a lymphomatous/leukemic process [10]. In present case, the histomorphological features of the cervical biopsy were classical.
MC is a benign and self-limiting infection and undergoes spontaneous resolution within months. Virus in later stage is considered as non-self by our body leading to activation of inflammatory pathways and causing spontaneous remission of this viral infection. But severe and prolonged course are associated with immunosuppression including HIV infection and Atopic dermatitis. If treatment is required, it should be supportive. Treatment can be in the form of curettage, laser, cryotherapy or salicylic acid [10]. In our case, the patient underwent biopsy curative treatment and supportive treatment. No follow up was done due to patient’s non-compliance.
Conclusion
MC in cervix is rare and can present as an incidental finding in a host with low immunity. As far as our knowledge goes only one case is reported in English literature till date and the present case will be the second case.
[1]. Diaconu R, Oprea B, Vasilesc MM, Niculescu EC, Ciobanu MO, Diaconu C, Inflamed molluscum contagiosum in a 6-year-old boy: a case reportRom J Morphol Embryol 2015 56(2):843-45. [Google Scholar]
[2]. Zhuang K, Ran Y, Xu F, Lama J, Atypical infantile genital Molluscum contagiosumAn Bras Dermatol 2015 90(3):403-05. [Google Scholar]
[3]. Guan H, Nuth M, Zhukovskaya N, Saw YL, Bell E, Isaacs SN, A Novel Target and Approach for Identifying Antivirals against Molluscum Contagiosum VirusAntimicrobial Agents and Chemotherapy 2014 58(12):7383-89. [Google Scholar]
[4]. ZurKenntnis JM, Des virus des Molluscum contagiosumDtsch Med Wochenschr 1905 31:1598-99. [Google Scholar]
[5]. Myskowski PL, Molluscum contagiosum. New insights, new directionsArch Dermatol 1997 133:1039-41. [Google Scholar]
[6]. Vera-Sempere FJ, Rubio L, Massmanian A, Counts and areas of S-100-positive epidermal dendritic cells in atypical molluscum contagiosum affecting HIV+ patientsHistol Histopathol 2001 16:45-51. [Google Scholar]
[7]. Ploubidou A, Moreau V, Ashman K, Reckmann I, González C, Way M, Vaccinia virus infection disrupts microtubule organization and centrosome functionEMBO J 2000 19:3932-44. [Google Scholar]
[8]. Perez-Diaz CE, Botero-Garcia CA, Rodriguez MC, Faccini-Martinez AA, Calixto OJ, Benitez F, Giant Molluscum Contagiosum in an HIV positive patientInt J Infect Dis 2015 38:153-55. [Google Scholar]
[9]. Mohan RPS, Verma S, Singh AK, Singh U, Molluscum contagiosum: report of one case with overviewBMJ Case Rep 2013 [Google Scholar]
[10]. Lang TU, Michelow P, Khalbuss WE, Monaco SE, Pantanowitz L, Molluscum contagiosum of the cervixDiagn Cytopathol 2012 40:615-16. [Google Scholar]