There had been a considerable rise in the prevalence of Tuberculosis (TB) in recent times, particularly among immune compromised population in the South East Asian subcontinent. TB can be a great mimicker of several other pathologies particularly in cases with only extra pulmonary sites involvement in immune compromised hosts. Previous literature has reported presence of only extra pulmonary TB in immune compromised population in up to 30% cases [1].
TB of the chest wall is rare and can mimic several pathologies; hence, diagnosis can be a challenge to clinician and radiologist [2]. Primary infective pathologies of the chest wall are rare, though can be seen to develop spontaneously in immuno compromised patients. Pyogenic osteomyelitis of the ribs or septic arthritis of the costoclavicular or sternoclavicular joints without any open wound trauma or as a part of post surgical complications is seen in intravenous drug addicts. Chest wall granuloma or abscesses have been rarely associated in infants with BCG vaccination [3]. Rarely peri-cardial tuberculoma and tubercular abscesses of diaphragm may extend into chest wall and complicate to form abscesses [4,5].
Thoracic actinomycosis is another rare bacterial infection with an indolent course, whose presenting manifestations with chest wall sinus tracts, abscesses can highly simulate tuberculosis [6]. Furthermore, rarely invasive aspergillosis in immunocompromised hosts following cardiac or cancer surgery or organ transplantation has been reported to involve chest wall and pleura with permeative osteolytic lesions in bony thorax. Phlegmonous soft tissue component without a frank abscess and rib destruction in an adult individual always raises the possibility of a neoplastic process like metastasis plasmacytoma or primary chondrosarcoma of the chest wall. Calcification in chronic abscesses might mimic the mineralization in chondrosarcomas in atypical cases; hence unfamiliarity with such pathologies and their imaging features will delay in establishing the final diagnosis [7]. Chest wall tuberculosis commonly presents with cold abscess [8] and non-healing sinus tract in chest wall, however with a lack of history of exposure and presence of active TB in the chest, such isolated involvement of the chest wall can be quite a diagnostic dilemma for the physicians and radiologists. Sometimes due to indigenous herbal treatments, there is occasional development of pustules or localized induration in the overlying skin in tubercular abscesses patients, which might be even further misleading for the clinicians. The imaging manifestations of TB of chest wall on cross-sectional imaging and how imaging helps in diagnosing such cases and differentiate from other pathologies have been elaborated in this article. Cross-sectional imaging not just helps in evaluation of site of involvement and extension of the disease process but also provides some common pattern which helps to recognize these cases.
The aim of this study was to evaluate the common sites and varying imaging appearances of isolated chest wall tuberculosis, thereby, trying to find a common pattern of imaging features if any and clues to differentiate it from other similar pathologies.
Materials and Methods
After approval from the institutional ethics review committee, a hospital based cross-sectional retrospective study was conducted. The study group comprised of 21 patients presenting to the Departments of Radiodiagnosis, Surgery, Medicine, TB and Chest in a tertiary care hospital from December 2010 to June 2016.
Patients with isolated chest wall tuberculosis including clavicle, sterno-clavicular joint and sternal lesions were included in this study. Pulmonary and spinal TB were excluded from our study. Imaging studies available included radiographs, USG and CT and MRI scans. Pathological confirmation was obtained in all cases (n-11 USG aspiration and n-10 surgical aspiration). Following USG as the baseline investigation only CT scan were done in 14 patients, only MRI in four patients, both CT and MRI scans were done in three patients. USG was done in Aplio -500 Toshiba Medical Systems machine using linear 7.5-13 MHz probe. CT scans of thorax were performed using Siemens Somatom Spirit Dual Slice CT Scanner with intravenous iodinated contrast administration and MRI scans were performed using Siemens Avanto 1.5 Tesla B15 machine. Pathological confirmation was obtained in all patients, after isolating tissue samples or aspirates using USG guided aspiration or surgical drainage.
Statistical Analysis
During analysis of CT scan or MRI images, we identified location and extension of lesion, pattern of bone destruction, associated bony sclerosis, periosteal reaction, sequestrum formation, presence of a soft tissue abscess, abnormal bony signal Intensity, diffusion characteristics and pattern of post contrast enhancement. The sites of affected thoracic cage were classified as anterior rib arc (including costo-chondral junction and costo-sternal junction), middle rib arc, posterior rib arc (including costo-vertebral joint).
MRI images identified location, extension and post contrast enhancement. The long axis of soft tissue abscess were measured and classified as small if long axis was less than 5 cm, medium if long axis was between 5 cm and 10 cm and large if long axis was more than 10 cm.
Results
The demographic details, clinical presentation and imaging features of these abscesses both on USG and CT/MRI have been enlisted in master chart [Table/Fig-1]. Further salient predominant findings have been summarized in [Table/Fig-2].
Showed clinico-radiological findings in 21 patients of isolated chest wall tuberculosis.
| CaseNo | Age/sex | Clinicalpresentation | Bony affectionsite | USGfindings | CT scan | MRI scan | Abscess/Inflammatorysoft tissue mass | Pattern ofenhancement |
|---|
| BE | PR | SeqF | SA | RD | Size of lesion | Location oflesion inrelation to rib |
|---|
| 1 | 32/M | Right upperback swelling | Right 3rd, 4thand 5th ribs (MA) | EID,SP,TP | + | No | - | + | + | Medium size | Both sides of rib | Thick wall |
| 2 | 35/M | Sinus tracts inright antero-lateralchest and swelling | Right scapula(glenoidal destruction) | EID,SP | + | + | - | - | - | Large size | Both sides of rib | Thick wall |
| 3 | 45/F | Right upperchest swelling | Right 4th rib (AA) | EID, SP | + | + | - | - | - | Small size | Both sides | Thick wall |
| 4 | 13/F | Right upperchest swelling | Right 5th rib(MA) | EID, SP,TP | + | + | - | - | - | Medium size | Both sides | Thick wall |
| 5 | 55/M | Midline anteriorchest wall swelling | Sternum(Manubrium and body) | EID | + | + | + | - | - | Medium size | Outer to rib | Thick wall |
| 6 | 20/M | Bilateral postchest wall swellings | Right 11th, 12thand left 11th ribs (PA) | - | + | No | - | + | + | Small size | Both sides of rib | Thick wall |
| 7 | 23/F | Left para-medianchest swelling | Left 3rd rib (AA) | - | + | No | - | - | - | Small size | Outer to rib | Phlegmonous |
| 8 | 18/M | Anterior chestwall swellings | Multiple sites (b/l clavicles,lt scapula, sternumand bilateral ribs) | EID | + | + | + | + | + | Small size | Both sides of rib | Phlegmonous |
| 9 | 43/F | Right lateral chestwall swelling | Right scapula inferiorportion destruction | EID, SP | + | + | - | - | - | Small size | Outer to rib | Thick wall |
| 10 | 24/M | Left supra-clavicularswelling | Left clavicle withpathological fracture | EID, SP,TP | + | No | - | + | + | Small size | Outer to rib | Thick wall |
| 11 | 56/M | Left upper chest wallswelling and sinus tract | Left SCJ | EID | + | No | - | + | - | Medium size | Both sides of rib | Phlegmonous |
| 12 | 30/M | Anterior chestwall swelling | Multiple sites (manubriumand body of sternum andright sided multiple ribs) | EID,SP | + | + | + | - | - | Medium size | Both sides of rib | Thick wall |
| 13 | 28/M | Non-healing sinustract in right anteriorchest wall | Right 5th rib (AA) | - | + | No | - | - | - | Medium size | Both sides of rib | Smoothmarginated |
| 14 | 12/F | Left upper chestwall swelling | Left Clavicle withpathological fracture | - | + | + | + | - | - | Small size | Both sides of rib | Phlegmonous |
| 15 | 20/M | Right lateral chestwall swelling | No bony involvement | EID, SP, TP | - | No | - | - | - | Medium size | Outer to rib | Thick wall |
| 16 | 10/M | Right para-medianchest wall swelling | Right sidedmultiple ribs (AA) | EIB,SP,TP | + | No | - | + | - | Small size | Both sides of rib | Thick wall |
| 17 | 36/M | Left upper chestwall swelling aroundleft sterno-calvicularjoint | Left SCJ | - | + | + | + | + | + | Small size | Outer to rib | Phlegmonous |
| 18 | 60/F | Supra-sternalswelling | Right SCJ | - | + | No | - | - | - | Small size | Both sides of rib | Smoothmarginated |
| 19 | 25/M | Right breast swellingwith swollen nipple | No bonyinvolvement | EID, SP | _ | No | - | - | - | Medium size | Outer to rib | Thick wall |
| 20 | 35/M | Bilateral posteriorchest wall abscess | Right sidedlower ribs (PA) | EID | + | + | + | - | - | Larger size | Outer to rib | Smoothmarginated |
| 21 | 46/M | Left para-medianchest wall swelling | Left 5th ribanterior end (AA) | - | + | - | - | - | - | Small size | Both sides of rib | Phlegmonous |
Echogenic Internal Debris-EID, Septa –SP, Thickened underlying Pleura-TP, Bone Erosion-BE, Periosteal Reaction-PR, Sequestrum Formation-SeqF, Diffusion Weighted Images-DWI, Abscess/Inflammatory soft tissue mass: small size(<5cm), medium size(5-10cm), large size (>10cm), Abnormal Signal Alteration-SA, DWI Restriction-RD, Anterior arc of rib-AA, Middle arc of rib-MA, Posterior arc of rib-PA, Sterno-Clavicular Joint-SCJ.
Predominant findings in our results among 21 patients {summary of master chart [Table/Fig-1]}.
| Cross Sectional Imaging findings | Frequency |
|---|
| Predominant site of affection in chest wall | Para-median anterior chest wall in four (19%) patients |
| Predominant site of bony involvement | Isolated rib involvement in nine (42.8%) patients |
| Predominant pattern of bony involvement | Bony sclerosis in 11 (52.4%) patients |
| Predominant size of the abscess | <5 cm in 11 (52.4%) patients and 5-10 cm in eight (38.1%) patients |
| Predominant pattern of enhancement of the abscess wall | Thicker irregular peripheral wall enhancement in 12 (57.1%) patients and phlegmonous inflammatory mass in six (28.6%) patients |
| Percentage of patients showing associated pleural thickening on USG | Five (23.8%) patients |
| Percentage of patients showing sinus tracts | Three (14.3%) patients |
| Percentage of patients showing sequestrum formation | Five (23.8%) patients |
| Percentage of patients with multiple bony site involvement | Two (9.5%) patients (multiple sites imply more than one different bone involvement like rib and sternum and not bilateral ribs involvement). |
| Percentage of diffusion restriction on MRI | 5/7 (five patients out of seven patients who underwent MRI) |
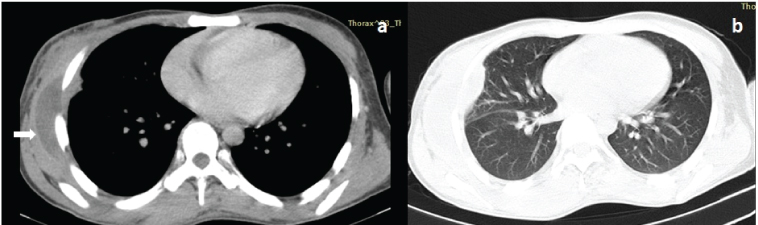
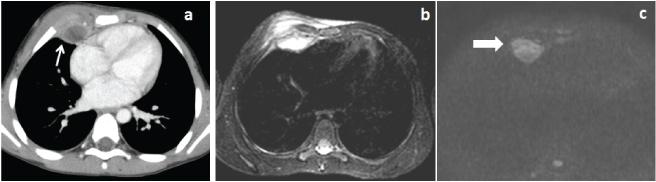
Majority of these abscesses extended on either side of the rib [Table/Fig-2,3] and 71.4% showed diffusion restriction on MRI [Table/Fig-2,4].
A 20-year-old male patient with right anterior lateral chest wall swelling. Axial post contrast CT: a) Lung window; b) Images showed thicker peripherally enhancing abscess (block arrow in image a) in right antero-lateral chest wall located external as well as internal to the rib.
A 10-year-old male patient had right chest wall swelling. Axial post contrast CT: a) Showed thick peripherally enhancing septated abscesses in right chest anterior wall (arrow), MRI scan with fat suppressed axial T2W image; b) Showed abnormal hyperintense signal intensities in right para-median anterior chest wall around the affected right costo-chondral junctions. Diffusion weighted image; c) Showed restriction in the lesion (block arrow).
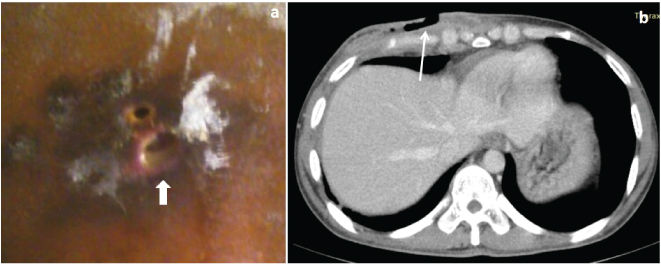
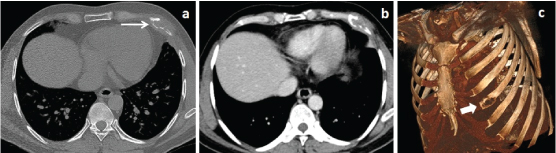
Chronic discharging sinuses were found only in three (14.3%) patients [Table/Fig-2,5]. Bony involvement was noted in 90.5% of patients, isolated rib involvement (42.8%) was the most predominant site of affection and bony sclerosis (52.4%) was the most dominant feature [Table/Fig-2,6].
A 28-year-old male presented with multiple chronic non-healing sinus tracts in right lower chest wall (block arrow in patient photograph in image a) Axial post contrast image; b) Showed right anterior chest wall abscess and sinus tract formation external to the rib (arrow).
A 46-year-old male patient had left para-median chest wall swelling. Axial CT scan images of bony algorithm: a) Post contrast; b) Images showed irregular destruction of anterior end of left fifth rib with destruction of both inner and outer cortices {arrow in [Table/Fig-6a]}.
USG showed pleural thickening in 23.8% of abscesses [Table/Fig-2,7] and USG guided aspiration was done from nine of these cases and surgical drainage or rib resection for the rest. In six out of the nine aspirates, Acid Fast Bacilli (AFB) could be isolated from culture but the remainder of the patients subsequently went to have a positive result following biopsy of excised sinus tract, ribs and culture of subsequent aspirates.
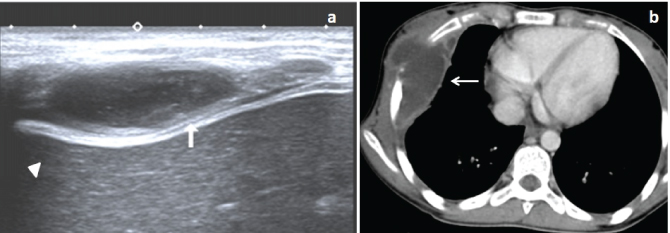
A 13-year-old female patient presented with right upper chest wall swelling. USG image a) Showed hypoechoic collection in right antero-lateral chest wall with internal echo-debris and thickened pleura (block arrow). Axial post contrast CT; b) Image showed thick peripherally enhancing loculated abscess in right chest wall both external and internal to ribs with extra-pleural extension (arrow).
Eleven patients (52.8%) were treated with only Anti-Tubercular Therapy (ATT) and rest of the 10 patients were (47.6%) treated with ATT with subsequent surgical drainage of chest wall abscesses or inflammatory mass.
Discussion
Chest wall tuberculosis has been reported to be 1% to 5% of all cases of musculoskeletal TB. However, chest wall tuberculosis represents between 1% to 2% of tuberculosis overall [9]. Chest wall tuberculosis can involve sternum, costo-chondral junctions, rib shafts, costo-vertebral joints and the vertebrae. Tuberculosis of the ribs constitutes 2% while sternum and sterno-clavicular joints constitute about 1-2% of total cases of musculoskeletal TB [10]. TB of rib lesions usually involves the mid-shaft of rib or the para-sternal area [11]. Tatelman M and Drouillard EJ described the frequency of isolated chest wall tuberculosis and found rib shaft involvement in 61% followed by the costo-vertebral joint in 35% and costo-chondral junction in13% cases [12]. In our study as well, we found maximum number of cases with isolated involvement of ribs 42.8% and commonly the anterior arc of ribs. Diagnosis of isolated chest wall tuberculosis in most of the cases is demanding because the lesions simulate pyogenic abscess or tumour and do not respond to conventional therapeutic interventions [13,14]. Chest wall tuberculosis was most frequently noted at the margins of sternum and along the rib shafts [15]. Even in more than 50% of rib TB lesions rib destruction may not be seen [8]. Lee G et al., reported rib destruction in 69% of the cases of rib tuberculosis [16], on CT scan in their study with associated soft tissue mass, osteolytic lesion in affected bones of rib cage, sequestrum and sinus tract formation suggesting chest wall tuberculosis.
According to Wiebe ER, isolated chest wall tuberculosis might occur either by hematogenous dissemination associated with activation of a dormant tuberculous focus or direct extension from a caseous lymph node of chest wall [17]. However, Burke HE on the other hand postulated local/widespread pleuritis as the initial lesion for formation of chest wall abscesses. He opined that tubercular bacilli first of all spread from a local pleuritis to locoregional nodes following which caseous material invades to chest wall layers from the para sternal or intercostals lymph nodes [18]. However, in present study we did not see any radiological evidence of any accompanying pleuritis at the time of involvement of chest wall. Chest wall abscesses sometimes invade into liver across diaphragm and in such situation patient may initially present with liver abscesses with silent chest wall lesion. These secondary liver abscesses formed from an extension of chest wall abscesses are difficult to differentiate from uncommon primary liver abscesses of tubercular origin. Cross-sectional imaging is of great value in differentiating such primary lesions from further complications or secondary extensions of chest wall abscesses [19].
Radiographic and CT scan findings of tuberculous sternal osteomyelitis have been reported as bone loss, which is relatively frequent, and rarely as sclerosis [20]. We found isolated involvement of sternum in only one patient and as part of sternoclavicular joint involvement in other three of our patients. In the literature rib tuberculosis have been described as rib erosions and destruction with adjacent abscess formation in plain radiograph and CT scan [15,21]. Erosions of the cortex were found to be more frequent feature (65%) of bony involvement in our cases, far more than sequestration and sclerosis. MRI shows marrow changes in the sternum, clavicle and rib as hypointense signal on T1WI and hyperintense signals on T2WI and fat suppressed sequences [10]. No particular pattern of this bone marrow edema was demonstrated in our cases and the distribution was close to the site of erosion of the cortex and abscess. No evidence of any intramedullary abscess was seen in any of the cases unlike in pyogenic osteomyelitis. Post gadolinium MRI images clearly depict clear extension of surrounding chest wall abscess. Abscess with thicker peripheral rim enhancement was the predominant feature seen, as part of soft tissue involvement and was found in 12 (57.1%) patients while phlegmonous inflammatory mass was found in six (28.6%) patients [Table/Fig-2]. Such chest wall abscesses with necrotic centers and rib erosions can also be found in cases of actinomycosis in immunocompromised patients, however, chest wall actinomycosis cases have always been reported in association with pulmonary and mediastinal disease. Thus, chest wall actinomycosis though rare is always preceded by pulmonary, neck or mediastinal involvement [22].
Similar imaging features are also occasionally produced by invasive bronchogenic cancer with central necrotic areas simulating abscesses as a response to chemo radiotherapy, however an appropriate history and comparative evaluation with prior imaging usually resolves such dilemma. We did not find the presence of gas in any of abscess but this can be found in cases with secondary bacterial infection and complicated by pleural, pulmonary or bronchial fistulas, hence absence of gas within the abscess cavity cannot be considered as a specific feature for cold abscesses of chest wall tuberculosis.
As per Kim HY et al., tuberculosis of the chest wall may or may not be characterized by bone or costal cartilage destruction and soft tissue masses demonstrating calcification or rim enhancement with or without evidence of underlying lung or pleural disease at CT may be the only feature [23]. An isolated chest wall and breast abscess was found in two of our patients without any bony changes. No rim calcification noted in any of these chest wall abscesses among our patients.
Newer modalities like Positron Emission Tomography-CT (PET-CT) and PET-MRI has role in the diagnosis of chest wall tuberculosis. Increased Fludeooxyglucose (FDG) uptake noted in active granulomatous inflammatory region with cold areas in necrotic or abscess regions [24].
The diagnosis of chest wall tuberculosis has to be confirmed on bacteriological or histological confirmation before ATT. Revised National Tuberculosis Control Programme (RNTCP) recommends a standard six months ATT regimen with two months of intensive phase (HRZE-Isoniazid+Rifampin+Pyrazinamide+Ethambutol) and four months of continuation phase (HR-Isoniazid+Rifampin), but treatment can be extended up to nine to 12 months depending upon clinical recovery [8,25]. If only medical treatment is not sufficient then surgical abscess drainage, excision of affected rib or wide debridement along with ATT may be needed [26].
Recent literature has established the efficacy of transdermal ultrasound-mediated anti tubercular drug delivery for the treatment of chest wall tuberculosis. Its outcome was superior to rationalized oral ATT [27].
Limitation
Descriptive study including only 21 patients without any control population which preclude assessment of actual specificity and accuracy of these imaging modalities.
Conclusion
Considering the rising trend of fulminant extra-pulmonary tuberculosis in immune compromised patients with variable presentation in partially treated cases, it is important to have adequate recognition and understanding of the radiologic manifestations of the chest wall involvement and complications of TB to facilitate diagnosis. Though CT definitely had a better sensitivity in detecting subtle and small areas of cortical erosions, defining the abscess extent, MRI did not provide any added diagnostic information. USG had a reasonable good pick up rate in detecting such collections in chest wall and even detecting bony erosions. From isolated breast abscesses to isolated sterna involvement we have found a wide range of imaging presentation in our cases, hence knowledge of the full spectrum of the chest wall TB is important to raise the suspicion in appropriate clinical settings as imaging features are largely nonspecific.
Echogenic Internal Debris-EID, Septa –SP, Thickened underlying Pleura-TP, Bone Erosion-BE, Periosteal Reaction-PR, Sequestrum Formation-SeqF, Diffusion Weighted Images-DWI, Abscess/Inflammatory soft tissue mass: small size(<5cm), medium size(5-10cm), large size (>10cm), Abnormal Signal Alteration-SA, DWI Restriction-RD, Anterior arc of rib-AA, Middle arc of rib-MA, Posterior arc of rib-PA, Sterno-Clavicular Joint-SCJ.