Giant Inguinal Herniae Managed by Primary Repair: A Case Series
Madhur Anand1, Ranendra Hajong2, Narang Naku3, Debobratta Hajong4, K Lenish Singh5
1 Resident Doctor, Department of Surgery, NEIGRIHMS, Shillong, Meghalaya, India.
2 Associate Professor, Department of Surgery, NEIGRIHMS, Shillong, Meghalaya, India.
3 Resident Doctor, Department of Surgery, NEIGRIHMS, Shillong, Meghalaya, India.
4 Resident Doctor, Department of Surgery, NEIGRIHMS, Shillong, Meghalaya, India.
5 Resident Doctor, Department of Surgery, NEIGRIHMS, Shillong, Meghalaya, India.
6 Resident Doctor, Department of Surgery, NEIGRIHMS, Shillong, Meghalaya, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ranendra Hajong, Department of Surgery, NEIGRIHMS, Shillong-793018, Meghalaya. India.
E-mail: ranenhajong@gmail.com
Giant inguinal hernia are usually found in developing countries due to delay in seeking medical attention. The management of such hernias may sometimes require procedures to increase the intra-peritoneal capacity prior to the repair of the giant hernia. Otherwise patients may develop abdominal compartment syndrome leading to various unwanted complications. Primary repair of giant hernias are possible in some cases without having significant post-operative complications. In this present case series, we have managed a total of four patients of giant inguinal hernia by primary repair without much post-operative complications.
Groin hernias, Mesh repair, Type I giant hernia
Case Series
An inguinal hernia is often labelled as giant hernia when it surpasses the mid-thigh level in an upright position in the absence of any reduction manoeuvre [1]. Although repair of such cases lacks any standardized procedure [2], the management of these cases needs enlargement of the abdominal cavity and it is seldom possible to repair these defects primarily owing to the size and the distorted anatomy of the inguinal canal. In the present series, we present 4 cases of giant inguinal hernia which were repaired primarily, without complications.
Between June 2014 and June 2015 [Table/Fig-1], a total 4 cases of giant inguinal hernia [Table/Fig-2,3,4 and 5] were operated at our hospital. The mean age was 57.25±10.78 years (range: 49-73 years). An overview of patient characteristics included in our series is depicted in [Table/Fig-1]. None of the patient had any concurrent urinary complaints. One patient had a remarkable cardiac co-morbidity for coronary artery disease, as well was hypertensive and obese, requiring a pre-operative temporary pacemaker implantation. All patients were post-operatively managed in high dependency unit for cardiopulmonary and intra-abdominal pressure monitoring, received antibiotics for first 72 hours and fully mobilized by post-operative day 1. Remarkable complications included bleeding, scrotal haematoma and wound dehiscence; all of which were managed effectively with prompt measures [Table/Fig-1]. All patients were followed up for at least one year and showed no signs of recurrence or any long-term complication.
Table showing patient characteristics.
| Case 1 [Table/Fig-3] | Case 2 [Table/Fig-5] | Case 3 [Table/Fig-2] | Case4 [Table/Fig-4] |
|---|
| Age (in years &) gender | 73, M | 52, M | 49, M | 55, M |
|---|
| Co-morbidities | 1.Coronary artery disease on aspirin-clopidogrel therapy2.Hypertensive3.Obesity (BMI 31kg/m2) | No known comorbid condition. | No known comorbid condition. | No known comorbid condition. |
| ASA grade | ASA III | ASA I | ASA I | ASA I |
| Giant hernia type, laterality | Type I, right | Type I, right | Type I, left | Type I, left |
| Type of hernia | Indirect | Indirect | Indirect | Indirect |
| Contents | Small intestine | Small intestine | Small intestine | Small intestine |
| Repair | Simple hernioplasty with polypropylene mesh 7.5x15 cm2 size | Simple hernioplasty with polypr-opylene mesh 7.5x15 cm2 size with scrotal skin excision | Simple hernioplasty with polypropylene mesh 7.5x15 cm2 size | Simple hernioplasty with polypr-opylene mesh 7.5x15 cm2 size |
| Post-operative complications | Bleeding at local site due to continued antiplatelet therapy in view of the comorbidity. Managed with pressure bandages | None recorded. | 1. Raised intraabdominal pressure (measured through foley’s catheter in bladder) with raised creatinine (2.9mg/dl)2. Superficial wound breakdown | Scrotal hematoma due to non-placement of drain |
| Course of the complications | Managed conservatively with pressure bandages, controlled within 24 hours | -- | 1. Managed conservatively in view of no cardiorespiratory compromise and good urine output (>0.5ml/kg/day). Improved within 72 h post-operatively2. Wound managed with removal of stitches and aseptic dressings at regular intervals during inpatient stay. | Managed conservatively with bed foot end elevation, pressure, anti-inflammatory agents and analgesics. |
| Post-operative stay | 5 days | 4 days | 7 days | 4 days |
| Follow up | No recurrence at one year of follow up | No recurrence at over 1 year of follow up | No recurrence at over 1 year of follow up | No recurrence at over 1 year of follow up |
Showing the left sided hernia in patient 3.

Showing right sided hernia in patient 1.

Showing left sided hernia in patient 4.
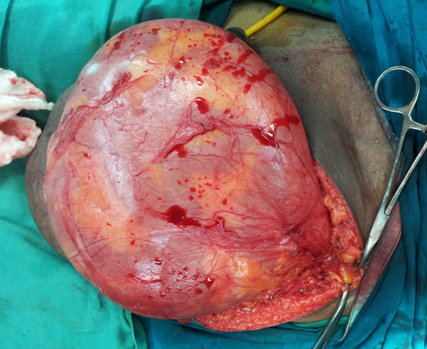
Showing bowel loops in patient 2.

Discussion
Pre-disposing factors contributing to the development of an inguinal hernia include: male sex, old age, chronic cough, chronic constipation, multiparity, premature birth or low birth weight, previous inguinal hernia or hernia repair, etc. In contrast to low income countries, occurrence of giant inguinoscrotal hernia is relatively uncommon in developed countries due to the early detection and prompt management. Giant inguinal hernia restrict patient’s mobility and often cause urinary issues owing to herniation of bladder as sac content [3]. Based upon the extent of herniation, giant inguinal hernia are broadly classified as: (a) Type I extending upto mid-thigh; (b) Type II extending midway between mid-thigh level and the suprapatellar line; and (c) Type III extending below the suprapatellar line [2]. Forceful reduction of a giant hernia into the abdominal cavity may lead to intra-abdominal hypertension and resultant abdominal compartment syndrome, intestinal obstruction, hernia recurrence and wound complications [3]. An important issue to be addressed while managing patients with giant inguinal hernia is the loss of abdominal domain. The techniques described to avoid abdominal compartment syndrome post-operatively included progressive creation of pneumoperitoneum pre-operatively, lengthening of the abdominal wall, using hernia sac as peritoneal flaps and even elective resection of the hernia contents sometimes [3]. These techniques have their own benefits and complications. Patients with type I hernia can be managed by forceful reduction in most cases while those with type II or III require meticulous resection of its content or expansion of intra-abdominal volume [2]. In our series, fortunately none of these surgical manoeuvres were needed for the management. A primary repair was able to achieve satisfactory outcome. Similar to our series, Trakarnsagna et al., Tarchouli et al., Coetzee et al., Tsutsumi et al., and Dinesh et al., report fair outcomes in type I and II giant hernia [2–6]. A series comprising of 15 patients, described primary Lichtenstein repair of giant inguinal hernia without any adverse long term outcome albeit early post-operative complications were reported in 73% of the cases [7]. Sahsamanis et al., treated a chronic, neglected giant inguinal hernia of 50-year-old duration via a ‘V shaped’ incision extending from the right inguinal region and lower mid-line. The contents of the hernia were forcefully reduced into the peritoneal cavity without any debulking [8]. Meticulous surgical technique remains the cornerstone of management [9–12]. Primary repair in all our patients was performed with standard polypropylene mesh 7.5x15 cm2 size by Lichtenstein tension free technique, currently regarded as the standard of care for large hernias. Post-surgical management including superficial wound dehiscence, transient intra-abdominal hypertension and hematoma were managed successfully with no evidence of any recurrence at one year follow up.
Conclusion
Giant inguinal hernia are less frequently seen variant of inguinal hernia. Its evaluation mandates a detailed local as well as systemic clinical assessment taking into account overall health co-morbidity status to predict satisfactory outcomes post-operatively. Giant inguinal hernias extending upto mid-thigh level can be managed via primary repair. Post-operative course requires monitoring of the cardiorespiratory status and intra-abdominal pressure. Appropriate patient selection for surgical management is critical in limiting complications and satisfactory prognosis.
[1]. Hodgkinson DJ, McIlrath DC, Scrotal reconstruction for giant inguinal herniasSurg Clin North Am 1984 64:307-13. [Google Scholar]
[2]. Trakarnsagna A, Chinswangwatanakul V, Methasate A, Swangsri J, Phalanusitthepha C, Parakonthun T, Giant inguinal hernia: report of a case and reviews of surgical techniquesInt J Surg Case Rep 2014 5(11):868-72. [Google Scholar]
[3]. Tarchouli M, Ratbi MB, Bouzroud M, Aitidir B, Ait-Ali A, Bounaim A, Giant inguinoscrotal hernia containing intestinal segments and urinary bladder successfully repaired by simple hernioplasty technique: a case reportJ Med Case Repo 2015 9:276 [Google Scholar]
[4]. Coetzee E, Price C, Boutall A, Simple repair of a giant inguinoscrotal herniaInt J Surg Case Rep 2011 2(3):32-35. [Google Scholar]
[5]. Tsutsumi N, Guntani A, Rikimaru T, Watanabe A, Kohnoe S, Giant inguinal her-nia containing right colon repaired using the prolene hernia systemANZ J Surg 2008 78(3):219 [Google Scholar]
[6]. Dinesh HN, Kumar CDJ, Shreyas N, Giant inguinoscrotal hernia repaired by Lichtenstein’s technique without loss of domain - a case reportJ Clin Diagn Res 2014 8:ND07-08. [Google Scholar]
[7]. Bierca J, Kosim A, Kołodziejczak M, Zmora J, Kultys E, Effectiveness of Lichtenstein repairs in planned treatment of giant inguinal hernia – own experienceVideosurgery and Other Miniinvasive Techniques 2013 1:36-42. [Google Scholar]
[8]. Sahsamanis G, Samaras S, Basios A, Katis K, Dimitrakopoulos G, Treatment of half century year old giant inguinoscrotal hernia. A case reportInt J Surg Case Rep 2016 25:51-54. [Google Scholar]
[9]. Kurzer M, Belsham PA, Kark AE, The Lichtenstein repairSurg Clin North Am 1998 78:1025-46. [Google Scholar]
[10]. Aufenacker TJ, van Geldere D, van Mesdag T, Bossers AN, Dekker B, Scheijde E, The role of antibiotic prophylaxis in prevention of wound infection after Lichtenstein open mesh repair of primary inguinal hernia: a multicenter double-blind randomized controlled trialAnn Surg 2004 240:955-60. [Google Scholar]
[11]. Terzi C, Antimicrobial prophylaxis in clean surgery with special focus on inguinal hernia repair with meshJ Hosp Infect 2006 62:427-36. [Google Scholar]
[12]. Shankar VG, Srinivasan K, Sistla SC, Jagdish S, Prophylactic antibiotics in open mesh repair of inguinal hernia – A randomized controlled trialInt J Surg 2010 8(6):444-47. [Google Scholar]