Absence of Posterior Triangle: Clinical and Embryological Perspective
Shikha Singh1, Puja Chauhan2, Hitendra Kumar Loh3, Vandana Mehta4, Rajesh Kumar Suri5
1 Senior Resident, Department of Anatomy, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India.
2 Assistant Professor, Department of Anatomy, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India.
3 Professor, Department of Anatomy, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India.
4 Professor and Head, Department of Anatomy, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India.
5 Director and Professor, Department of Anatomy, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Puja Chauhan, Department of Anatomy, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi -110029, India.
E-mail: drpujachauhan@gmail.com
Sternocleidomastoid (SCM) and Trapezius (TM) muscle present in the cervical region serves as an important landmark in forming boundaries of posterior triangle of neck. This case reports a continuous muscle sheet obscuring the left posterior triangle in the neck of a 60-year-old Indian male cadaver. An unfamiliar oval gap was observed in its posterosuperior portion. Description of such a variant in anatomical literature is rare and is scarcely reported. An attempt has been made to portray its embryological and phylogenetic basis. In addition authors have endeavoured to discuss its clinical implications. Awareness of such anatomical variations is relevant for the operating surgeons in their endeavour to perform various reconstruction surgeries of head and neck, radiologists while concluding various levels in Computed Tomography (CT) and Magnetic Resonance Images (MRI) of the region and to the anaesthetists in their search for nerves and vessels while attempting various anaesthetic procedures.
Fusion, Partial degeneration, Sternocleidomastoid, Trapezius
Case Report
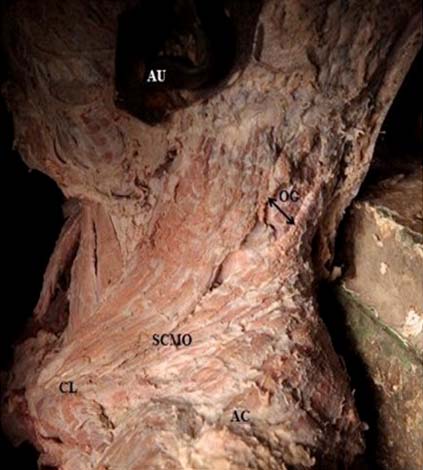
During routine dissection of head and neck region in a 60-year-old Indian male cadaver, surprisingly no anatomical posterior triangle was found on the left side of the neck. SCM and TM enclosed in investing layer of deep cervical fascia were seen as a continuous sheet encircling the neck like a fasciomuscular collar. This muscular sheet arose in continuity from manubrium, whole extent of clavicle (superior surface of medial two third and posterior border of lateral one third), medial surface of acromion process and upper lip of spine of the scapula. The fibers were directed posterosuperiorly and could be traced up to the mastoid process, whole extent of superior nuchal line, external occipital protuberance, ligamentum nuchae, C 7 spine and thoracic spines. Length of this sheet along the anterior border measured 14cm. Neurovascular contents of posterior triangle were placed deep to this fused muscular lamina. In the region, below the medial one third of superior nuchal line, an oval deficiency oriented obliquely along the direction of fibres of muscle was also observed. The anterior and posterior margins of the deficiency measured 6cm and 8cm respectively, and its maximum width was 2cm. Splenius capitis and Levator scapulae occupied the floor of this gap [Table/Fig-1,2]. The right posterior triangle exhibited usual anatomical profile.
Schematic illustration depicting fused SCM and trapezius.
AC- acromion process, AU – auricle, CL – clavicle, OG – oval gap
SCMO – sternocleio-mastoido-occipitalis

Superficial dissection of the left side of neck.
AC- acromion process, AU – auricle, CL – clavicle
OG – oval gap, SCMO – sternocleio-mastoido-occipitalis
Discussion
The SCM and TM muscles are considered to be important landmarks for the cervical region, the former dividing the neck into anterior and posterior triangles and the latter constituting the posterior limit of posterior triangle. Both these muscles are innervated by the spinal accessory nerve. SCM when acting individually tilts the head towards same side and turns the face to opposite side whereas, simultaneous action of the muscles on both sides causes flexion of the head during routine activities. TM is an important muscle of the back which serves an important role in movements of spine and is also chiefly implicated in overhead abduction [1].
Studies in the past have commonly reported variant attachments of SCM [2,3] and TM [4,5]. The current investigation reports an extremely rare variant muscle formed as a result of fusion of SCM and TM. The authors strive to report this unusual case in order to augment the anatomical literature pertaining to cervical musculature and their variations, thereby helping in updating knowledge of surgeons.
The TM and SCM muscles are derived partly from the neural crest and partly from somites and are innervated by the accessory nerve, which can neither be categorized as true cranial nerve nor as true spinal nerve [6].
They share a common origin from the occipital region just caudal to the last branchial arch and develop as a thick columnar mass which then separates into a ventral part, forming the SCM, and a dorsal part, forming TM [7]. Fusion of the two muscles can be attributed to inability of the sixth arch mesoderm to separate into two independent masses
Some of the investigators have reported the extended attachment of SCM and TM to the extent that edges of the two muscles were in contact [1]. In most of the cases, the additional muscle has been reported to divide into multiple slips [2]. In one of the studies, SCM muscle was found to extend laterally without division into multiple slips [3] but muscle variant exhibiting fusion of sternal head, clavicular head, and the posterior border of SCM with TM as seen in the current study has not been documented yet.
Since, the muscle sheet observed in the current study represents anatomical unification of SCM and TM. Therefore, in view of its chief attachments, this muscle variant can justifiably be designated as Sternocleido-mastoido-occipitalis (the nomenclature has been designated by the authors themselves based on the anatomy of the variant muscle and to the best of our knowledge has not been found any anatomy literature available till date).
Phylogenetically, SCM and TM originated from single muscle cucullaris, which split into two parts during mammalian evolution [8]. Considering the view ‘ontogeny reiterates phylogeny’ fusion of the two muscles can thus be credited to flaw in phylogenetic development as well.
A study reported, bilateral presence of anomalous muscle with a separate descending portion and a partially deficient cervical portion [4]. They reserved the term cleidooccipitalis for this variant and suggested that, it might be the result of partial degeneration than partial agenesis of TM.
The gap in the superior part of muscle observed in the current study is an interesting finding and may be ascribed to degeneration in fibres of a portion of TM rather than to a deficiency in the development of the fibres. This can happen secondary to lack of blood supply, disruption of normal innervation or can be congenital primary agenesis [9].
In recent times, radiological parameters have been defined to identify boundaries amid various neck levels, out of which the posterior border of SCM muscle is an important landmark [10]. Hence, possibility of fusion of SCM and TM should be kept in mind while deciding various levels in Computed Tomography (CT) and Magnetic Resonance Images (MRI). Posterior border of SCM is also commonly needed as reference point in search for nerves during neural blockade in surgical practices.
SCM and TM muscles also form the mechanical basis of various head movements and are deliberated as accessory muscles in respiration [11]. Authors wish to speculate that unilateral fusion of both the muscles encountered in the current investigation can presumably lead to functional imbalance between two sides. The altered anatomical profile of the musculature could also possibly be responsible for compression neurovasculopathy and exaggerated clinical picture of wry neck. Admittedly, clinical history of the patient was not available for corroborating the findings.
The additional muscle mass formed as a result of fusion can be used by surgeons as myocutaneous flap for reconstruction of head and neck defects as well as for restoration of oral cavity. Moreover, along with part of clavicle it can be used for mandibular reconstruction. Strengthening the suture line thereby, protecting the carotid and innominate artery is also done using these flaps [12].
SCM flaps have an edge over other flaps in providing soft tissue contour, coverage of facial nerves, nerve grafts and also act as healthy graft bed for skin grafts [13]. They are very efficient for preventing Frey’s syndrome following parotidectomy and closure of parotid fistulas [14]. Role of SCM graft for facial animation in order to rehabilitate the paralysed face is well established [12].
Furthermore, complete fusion of SCM and TM as in the present case with consequent absence of lesser supraclavicular fossa (preferred approach) could pose problems during internal jugular vein catheterization. It can cause fortuitous puncture of the adjoining neurovascular structures leading to haemorrhage or even neural deficits [1].
Radiotherapy induced spasm of SCM can be relieved by botulinum injections in the muscle. Fusion of SCM and TM leading to formation of large muscle mass may require additional dosage of the same [15].
Conclusion
Muscle variant found in the present study can be embryologically explained by inability of the sixth arch mesoderm to separate into two independent masses whereas in view of its presence in lower animals can also be attributed to an erroneous phylogenetic development. We as anatomists, submit that awareness of such anatomical variations is relevant for the operating surgeons in their endeavour to perform various reconstruction surgeries of head and neck, radiologists while concluding various levels in CT and MR images of the region and also is of tremendous significance to the anaesthetists in their search for nerves and vessels while attempting various anaesthetic procedures.
[1]. Standring S, Borley NR, Collins P, Crossman AR, Gatzoulis MA, Healy JC, Gray’s AnatomyThe Anatomical basis of clinical practice 2008 40th editionNew YorkChurchill Livingstone:437:803:441 [Google Scholar]
[2]. Mehta V, Arora J, Kumar A, Nayar AK, Loh HK, Gupta V, Bipartite clavicular attachment of sternocleidomastoid muscleAnat Cell Biol 2012 45:66-69. [Google Scholar]
[3]. Amorim JR AA, Lins CCSA, Cardoso APS, Damascena CG, Variation in clavicular origin of sternocleidomastoid muscleInternational Journal of Morphology 2010 28(1):97-98. [Google Scholar]
[4]. Rahman HA, Yamadori T, Anomalous cleidooccipitalis muscleActaAnat (Basel) 1994 150(2):156-58. [Google Scholar]
[5]. Kwak HH, Kim HJ, Youn KH, Park HD, Chung IH, An anatomic variation of the trapezius muscle in a Korean: the cleido-occipitalis cervicalisYonsei Med J 2003 44(6):1098-100. [Google Scholar]
[6]. Benninger B, McNeil J, Transitional Nerve: A new and original classification of a peripheral nerve supported by the nature of the accessory nerve (CN XI)Neurology Research International 2010 2010:476018 [Google Scholar]
[7]. McKenzie J, The development of the sternomastoid and trapezius musclesCarnegie Institution of Washington, Publication No. 621: Contributions to Embryology 1962 37(258):121-29. [Google Scholar]
[8]. Edgewort FH, The cranial muscles of vertebrates 1935 LondonCambridge university press [Google Scholar]
[9]. Durham University, The effects of ischaemia and denervation on mammalian muscle spindles [Internet] c1983 [15 May 2013] Hassan DFDurham UniversityAvailable from: http://etheses.dur.ac.uk/7198/ [Google Scholar]
[10]. Hamoir M, Desuter G, Gregoire V, Reychler H, Rombaux P, Lengele B, A proposal for redefining the boundaries of level V in the neck: is the dissection of the apex level V necessary in mucosal squamous cell carcinoma of the head and neck?Arch Otolaryngol Head Neck Surg 2002 128:1381-83. [Google Scholar]
[11]. Costa D, Vitti M, Oliveira DT, Costa RP, Participation of the sternocleidomastoid muscle on deep inspiration in man: An electromyographic studyElectromyogr. Clin. Neurophysiol 1994 34:315-20. [Google Scholar]
[12]. Conley J, Gullane PJ, The sternocleidomastoid muscle flapHead Neck Surg 1980 2:308-11. [Google Scholar]
[13]. Bugis SP, Young JE, Archibald SD, Sternocleidomastoid flap following parotidectomyHead Neck 1990 12(5):430-35. [Google Scholar]
[14]. Filho WQ, Dedivitis RA, Rapoport A, Guimarães AV, Sternocleidomastoid muscle flap preventing Frey syndrome following parotidectomyWorld journal of surgery 2004 28(4):361-64. [Google Scholar]
[15]. Van Daele DJ, Finnegan EM, Rodnitzky RL, Zhen W, McCulloch TM, Hoffman HT, Head and neck muscle spasm after radiotherapy: management with botulinum toxin a injectionArch Otolaryngol Head Neck Surg 2002 128(8):956-59. [Google Scholar]