Intraosseous Neurofibroma of the Mandible: A Case Report and Review of Literature
Bindiya Ramesh Narang1, Sangeeta Jayant Palaskar2, Anirudha Ratnadeep Bartake3, Rasika Balkrishna Pawar4, Sumit Rongte5
1 Reader, Department of Oral Pathology, Sinhgad Dental College and Hospital, Pune, Maharashtra, India.
2 Head, Department of Oral Pathology, Sinhgad Dental College and Hospital, Pune, Maharashtra, India.
3 Reader, Department of Oral Pathology, Sinhgad Dental College and Hospital, Pune, Maharashtra, India.
4 Lecturer, Department of Oral Pathology, Sinhgad Dental College and Hospital, Pune, Maharashtra, India.
5 Postgraduate Student, Department of Oral Pathology and Microbiology, Sinhgad Dental College & Hospital, Pune, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Bindiya Ramesh Narang, Staff Quarters, North Block, Flat No 201, STES Society, Vadgaon Campus, Vadgaon Budruk, Off Sinhagad Road, Pune-411014, Maharashtra, India.
E-mail: drbindiya@yahoo.co.in
Neurofibroma (NF) is a benign tumor of the peripheral nervous system. Head and neck NF are generally located in the soft tissue. The tumour is rarely seen intraosseously and most commonly such tumours are seen as solitary lesions, rather than part of neurofibromatosis. The following report describes a case of an intraosseous neurofibroma in a 45-year-old male located in the left posterior mandible. The diagnosis was made based on the clinical findings, radio graphical features, histopathology, and immunohistochemistry. A literature review has been done on intraosseuos neurofibromas located in the jaws, with a discussion on the possible differential diagnosis.
Benign tumour, Immunohistochemistry, Nerve sheath, Peripheral nervous system
Case Report
A 45-year-old male patient presented with a swelling in the left posterior region of the mandible extending from tragus of the ear and crossing the midline towards the right side of the face [Table/Fig-1]. The swelling was first observed one to one and half years back which started as a small swelling and has reached to the present size. Extra orally, a diffuse swelling was seen on the left side of the face extending from the angle of the mandible to the mid symphysis. There were no lesions seen on the skin. On intraoral examination, the swelling was seen from the left third molar region to the central incisor of the opposite side crossing the midline. The swelling was irregular in shape, firm in consistency, with irregular borders and a rough texture [Table/Fig-2]. There was no associated pain or tenderness. The patient gave history of exfoliated teeth due to mobility in the same region of the jaw.
Photomicrograph showing diffuse swelling on the left side of the mandible.

Intraoral view of the tumour.

Orthopantomograph (OPG) showed irregular radiolucency in the area of lesion involving the mandibular canal with displacement of the anterior teeth and missing teeth #33-38 [Table/Fig-3].
Panoramic radiography showing a diffuse radiolucency on the left side of the mandible along with displaced teeth.

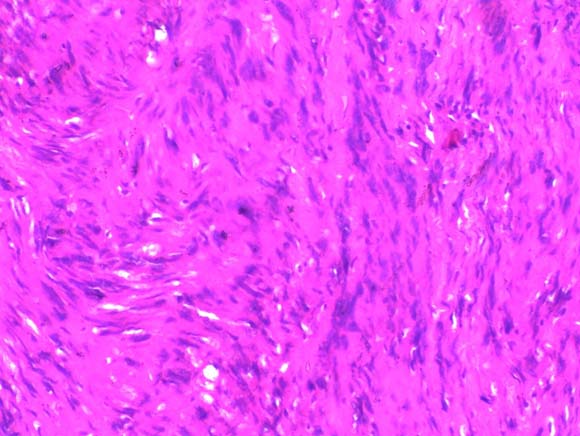
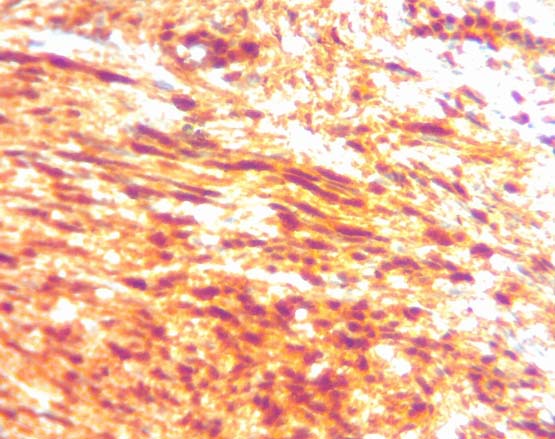
An incisional biopsy was done and the specimen was sent with a provisional diagnosis of ameloblastoma. The haematoxylin and eosin sections of the incisional biopsy tissue showed hyper cellular connective tissue stroma consisting of spindle shaped cells, with wavy nuclei arranged in fascicular and storiform patterns. Hence, the diagnosis of NF was given which was followed by left hemi-mandibulectomy along with the dissection of supraomohyoid lymph nodes [Table/Fig-4]. Similar histopathological picture was seen in excisional biopsy tissue [Table/Fig-5]. Immunohistochemistry staining with S-100 showed strong positivity signifying the neural origin of the tumour [Table/Fig-6]. Mind bomb E3 Ubiquitin Protein Ligase 1 (MIB-1), which was negative, revealed a low proliferative index of the tumor thus, excluding its malignant nature.

Photomicrograph showing spindle shaped cells with wavy nuclei (H&E x20).
Photomicrograph showing S-100 positive spindle shaped cells with wavy nuclei (x10).
Discussion
NF is a benign tumor of the peripheral nervous system. In most of cases, they are found as solitary tumors, though in few cases multiple lesions are seen in persons with neurofibromatosis, an autosomal dominant genetically inherited disease [1]. Bruce described solitary NF of the oral cavity in 1954. NFs are most commonly seen on the skin and only 6% of the cases have been reported in the oral cavity [2]. NFs can also occur intraosseously, the major location being the posterior region of mandible. A few cases have been reported in the maxilla as well. Literature search reveals very few cases of NF of oral cavity. Approximately 25% of the NFs are seen in the head and neck region, and 5.6% of them occur in the oral cavity. Among the craniofacial region, NF often involve 5th cranial nerve and upper cervical nerves, with common sites being, tongue, lip, palate, gingiva, major salivary glands and jaw bones [2]. A literature review has been done of reported cases of intraosseous NFs based on clinical examination, radiographic findings, histological features and immunohistochemical reactivity [Table/Fig-7].
A review on clinical, histopathological and immunohistochemical features of intraosseous neurofibroma of the oral cavity.
| Author | Age | Gender | Location | Symptomatology | Radiographic Features | Histological Features | Immunohistochemistry Features |
|---|
| Larsson et al., [3] | 46 Yr | M | Mandible | Intermittent pain | Bone destruction with slightly radio opaque areas | Spindle cells with elongate or oval nuclei forming cords | Not perfomed |
| Larsson et al., [3] | 25 Yr | F | Mandible | No | Extense bone resorption | Irregular nerve fiber strands intermigled with collagen fibers and abundant cells | Not perfomed |
| Skouteris et al., [4] | 16 Yr | F | Maxilla | No | Poorly-defined radiolucent lesion | Spindle cells and abundant myxomatous stroma | Not perfomed |
| Polak et al., [5] | 60 Yr | M | Mandible | No | Unilocular radiolucency | Cords of fusiform or ovoid cells intermixed with a fibrillary stroma | Anti S-100 Positive Anti- Lai 7 Positive |
| Mori et al., [6] | 18 Yr | F | Maxilla | Tooth mobility | Well circumscribed multilocular radiolucency | Wavy growth of tumor cells in a myxomatous matrix | Anti S-100 Positive |
| Poupard et al., [7] | 14 Yr | M | Maxilla | No | Poorly defined radiolucency | Spindle and stellate cells with a mucoid extracellular material with some condensation of fibrous tissue | Anti S-100 Positive |
| Apostolidis et al., [8] | 67 Yr | F | Mandible | Paresthesia and hyperesthesia | Circumscribed elliptical radiolucency with expansion of the mandibular canal | Numerous spindle cells in a myxoid matrix | Not perfomed |
| Vivek et al., [9] | 39 Yr | F | Mandible | No | Well circumscribed radiolucent area with continuity loss of the mandibular canal | Spindle cells with wavy nuclei arranged in the form of booklets | Anti S-100 Positive |
| Narwal A et al., [10] | 5 months | F | Maxilla | No | Radiolucent mass enclosed by radiopaque border | Densely arranged collagen fibers, plum fibroblasts, nerve bundles, wavy nuclei | S-100 positive, EMA negative |
| Depprich R et al., [11] | 64 Yr | M | Mandible | No | No | Proliferative spindle cells in myxoid stroma | S-100 Positive |
| Sharma et al., [12] | 5 months | F | Maxilla | No | No | Cords of dense collagen fibers intermixed with strands of nerve tissue with wavy nuclei | Anti S-100 Positive EMA Negative |
| Dalili Z and Adham GH [13] | 16 Yr | M | Maxilla | Hypoglobus and proptosis of left eye | Oval radiolucency, destruction of overlying bone | Spindle and ovoid cells, wavy nuclei in fairly lose matrix | S-100 Positive |
| Bharat TS et al., [14] | 30 Yr | F | Palate | Mild intermittent dull aching pain | No | Spindle shaped cells, wavy nuclei in Myxomatous areas | S-100, NSE, Vimentin Positive |
| Jain D et al., [15] | 65 Yr | F | Maxilla | Exfoliation of teeth, dysphagia | Slight haziness in maxillary sinus | Myxoid stroma, spindle cells, few areas of plexiform pattern | Not performed |
| Jangam SS et al., [1] | 62 Yr | F | Mandible | Occasional sharp pain, parasthesia, of lower lip | Well defined radiolucency | Admixture of nerve fibers and fibrous tissue | S-100 Positive |
| Gujjar PK et al., [2] | 28 Yr | F | Mandible | Intermittent pain | Homogeneous radio opacity surrounded by thin radiolucent border | Proliferation of spindle cell with wavy nuclei with in myxoid stroma | S-100 Positive |
NF is caused by a germline mutation in the NF1 gene, a tumor suppressor gene located at 17q11.2 chromosome. This gene encodes for a protein known as neurofibromin, which plays a role in neural cell signaling.
The mean age of occurrence is 27.5 years with a slight predilection towards females [2,16].
Most of the intra-osseous NFs do not show any symptoms in the initial stages. Later on pain and numbness of the affected side of the lip may occur [2]. On radiograph, it appears as a well circumscribed or poorly demarcated radiolucency which usually involves the mandibular canal as seen in our case [8].
As a rule, the gross appearance of the tumours is not encapsulated and has a softer consistency [8] though the presentation may vary from case to case.
Microscopically, these tumours are composed of all the elements of peripheral nerve. The Schwann cells usually represent the predominant cellular element which is seen as small round to spindle shaped cells with wavy nuclei showing a serpentine configuration and pointed ends. The stroma is composed of a rich network of collagen fibers which are arranged in a characteristic “shredded carrot pattern”. Few NFs, especially the cellular one’s show fascicular or storiform growth pattern of cells [8], myxoid areas and scattered mast cells are found in the connective tissue.
NFs may exhibit cells with large hyperchromatic nuclei. These NFs with atypia may also have increased cellularity but mitotic activity is scanty or absent and the MIB-1 index is very low. The immunoreactivity for MIB-1 was negative in the present case.
On immunohistochemistry, NFs show a strong positivity for S-100 protein, variable numbers of EMA positive perineural cells and CD34 positive fibroblasts may also be seen. Immunoreactivity for PGP 9.5 is often seen but its degree of specificity is very low [10].
NFs should be differentiated from other spindle cell lesions like schw-annoma, traumatic neuroma, desmoplastic melanotic melanoma, benign fibrous histiocytoma, spindle carcinoma and amelanotic melanoma [2]. Absence of verocay bodies, presence of mast cells, and fine fibrillar collagen matrix differentiates NF from Schwannoma [17]. A positive history of trauma in traumatic neuroma is necessary for its diagnosis. Desmoplastic melanoma demonstrates junctional melanocytic proliferation, neurotropic growth and the presence of lymphoid aggregate in the deep dermis and subcutis. The cells tend to grow together in small packets which is not seen in NF [18]. NFs need to be differentiated from other neural tumors as the malignant transformation rate is around 5% to 16% [8].
Radical surgery which includes hemimandibulectomy or enbloc resection of the mandible is often advocated for the treatment of intraosseous neurofibroma [9]. Local recurrence of NFs has been reported which is attributed to absence of complete capsule making complete surgical removal of the tumor difficult [1,8].
Conclusion
It is important to recognize and diagnose these tumors, as they could be the first manifestation of neurofibromatosis. These tumours are known to recur and thus, it is essential to conduct a thorough clinical and radiographical examination along with long term follow up. As the follow up information is not available in the literature search, the transformation into neurofibromatosis cannot be commented on.
[1]. Jangam SS, Ingole SN, Deshpande MD, Ranadive PA, Solitary intraosseous neurofibroma: Report of a unique caseContemp Clin Dent 2014 5(4):561-63. [Google Scholar]
[2]. Gujjar PK, Hallur JM, Patil ST, Dakshinamurthy SM, Chande M, Pereira T, The solitary variant of mandibular intraosseous neurofibroma: Report of a rare entityCase Rep Dent 2015 2015:520261 [Google Scholar]
[3]. Larsson A, Praetorius F, Hjorting- Hansen E, Intraosseous neurofibroma of jawInt J Oral Surg 1978 7:494-99. [Google Scholar]
[4]. Skouteris CA, Sotereanos GC, Solitary neurofibroma of the maxilla: Report of a caseJ Oral Maxillofac Surg 1988 46:701-05. [Google Scholar]
[5]. Polak M, Polak G, Brocheriou C, Vigneul J, Solitary neurofibroma of the mandible: Case report and review of the literatureJ Oral Maxillofac Surg 1989 47:65-68. [Google Scholar]
[6]. Mori H, Kakuta S, Yamaguchi A, Nagumo M, Solitary intraosseous neurofibroma of the maxilla: Report of a caseJ Oral Maxillofac Surg 1993 51:688-90. [Google Scholar]
[7]. Poupard RJ, Mintz S, Solitary intrabony neurofibroma of the maxillaJ Oral Maxillofac Surg 1997 55:768-72. [Google Scholar]
[8]. Apostolidis C, Anterriotis D, Rapidis AD, Angelopoulos AP, Solitary intraosseous neurofibroma of the inferior alveolar nerve: Report of a caseJ Oral Maxillofac Surg 2001 59:232-35. [Google Scholar]
[9]. Vivek N, Manikandhan R, James P C, Rajeev R, Solitary intraosseous neurofibroma of mandibleIndian J Dent Res 2006 17:135-38. [Google Scholar]
[10]. Narwal A, Saxena S, Rathod V, Bansal P, Intraoral solitary neurofibroma in an infantJ Oral Maxillofac Pathol 2008 12(2):75-78. [Google Scholar]
[11]. Depprich R, Singh DD, Reinecke P, Kübler NR, Handschel J, Solitary submucous neurofibroma of the mandible: Review of the literature and report of a rare caseHead & Face Medicine 2009 5:24 [Google Scholar]
[12]. Sharma P, Narwal A, Rana AS, Kumar S, Intraosseous neurofibroma of maxilla in a childJ Indian Soc Pedod Prevent Dent 2009 27(1):62-64. [Google Scholar]
[13]. Dalili Z, Adham GH, Intraooseous neurofibroma and concurrent involvement of the mandible, maxilla, orbit: Report of a caseIran J Radiol 2012 9(1):45-49. [Google Scholar]
[14]. Bharath TS, Krishna YR, Nalabolu GR, Pasupuleti S, Surapaneni S, Ganta SB, Neurofibroma of the PalateCase Rep Dent 2014 2014:898505 [Google Scholar]
[15]. Jain D, Chaudhary M, Patil S, Neurofibroma of the maxillary antrum: A rare caseContemp Clin Dent 2014 5:115-18. [Google Scholar]
[16]. Deichler J, Martínez R, Niklander S, Seguel H, Marshall M, Esguep A, Solitary intraosseous neurofibroma of the mandible. Apropos of a caseMed Oral Patol Oral Cir Bucal 2011 16(6):e704-07. [Google Scholar]
[17]. Roy P, Chakraborty S, Das S, Roy A, Solitary neurofibroma at the base of the tongue: A rare presentationIndian J Dermatol 2015 60:497-99. [Google Scholar]
[18]. Douglas R, Gnepp MD, Diagnostic surgical pathology of the head and neck 2009 2nd EdSaunders: Elsevier:1011-12. [Google Scholar]