Adenocarcinoma, Avastin, Carboplatin, Chemotherapy, Dyspnea, Taxol
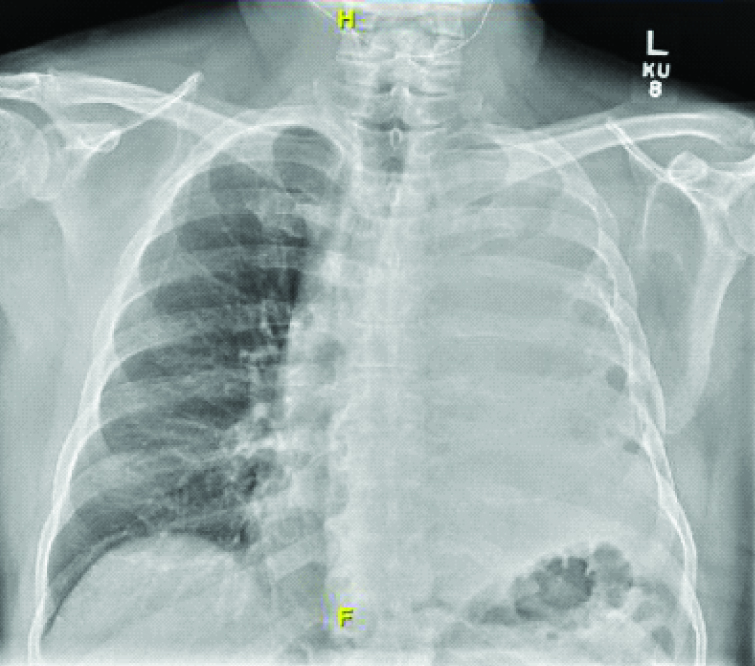
A 64-year-old man presented to our outpatient clinic with a four month history of dyspnea and cough with sputum. He was a non smoker and had no significant occupational exposures. He had been evaluated in a hospital in Peru one month ago with similar complaints and was given a short course of antibiotics for pneumonia. He had similar symptoms approximately 15 years ago when he was diagnosed of pleuritis and underwent a surgical procedure that he cannot remember. At the time of his visit to us, his examination was remarkable for absent breath sounds over the left lung field. A chest radiograph [Table/Fig-1] showed complete opacification of the left hemithorax. The differential diagnosis at this point included left lung collapse due to space occupying lesion. As he did not remember the surgical procedure done before we were of the opinion that he may have undergone a pneumonectomy. Also complete lung collapse was considered due to infection however, there was no shift towards the affected lung and he was not appearing septic.
Portable chest X-ray done on admission in emergency room showing complete opacification of the left hemithorax.
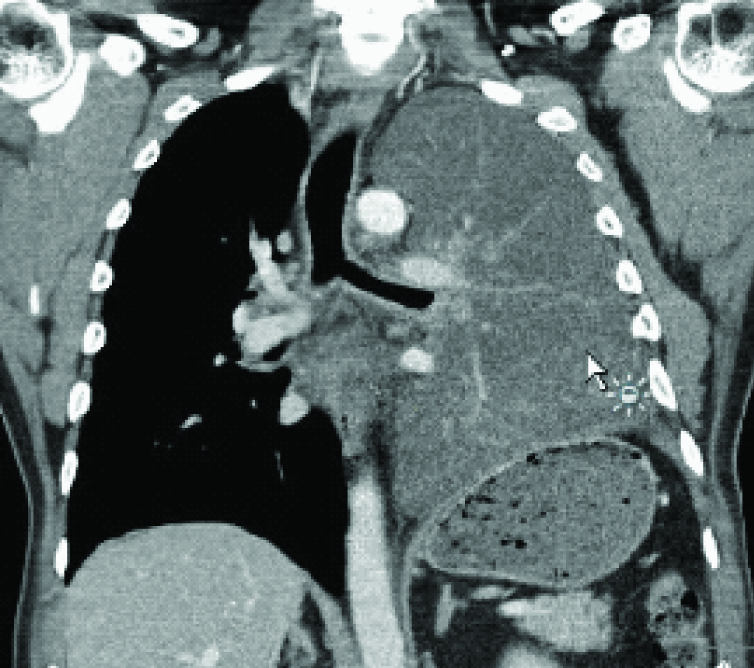
Computed tomography [Table/Fig-2] revealed an indeterminate diffuse infiltrative process with abrupt cutoff of the left mainstem bronchus and changes were consistent with a previous left thoracotomy. Elevation of the left hemidiaphragm was thought to be due to mild volume loss from expulsion of air and the airway filling process. But more importantly, there were no major structural changes or invasion of other organs or bones.
Computed tomography of the chest showing diffuse infiltrative process occupying the airspace of the left lung.
Bronchoscopy showed severe cobblestoning of the trachea and occlusion of the left mainstem bronchus with necrotic material. This was cleared and bronchial washings were obtained, however, due to excessive mucosal bleeding after bronchial alveolar lavage of the left mainstem, the procedure was terminated and the right side was not inspected. Cytology from the bronchial washings showed adenocarcinoma with positive markers for CK7 and MOC-31 which favored primary lung phenotype [1]. Genetic testing was performed and the tumor was found to be Anaplastic Lymphoma Kinase (ALK) and Epidermal Growth Factor Receptor (EGFR) negative. A staging Positron Emission Tomography Computed Tomography (PET/CT) showed uptake throughout the trachea, bilateral mediastinal lymph nodes, bilateral hilar lymph nodes, bilateral paratracheal as well as scalene and suprahyoid lymph nodes, corresponding with Stage IV disease. He was started on a carboplatin, taxol and avastin regimen for palliation and there was some symptomatic as well as radiographic improvement [Table/Fig-3].
Computed tomography of the chest showing some resolution after chemotherapy.
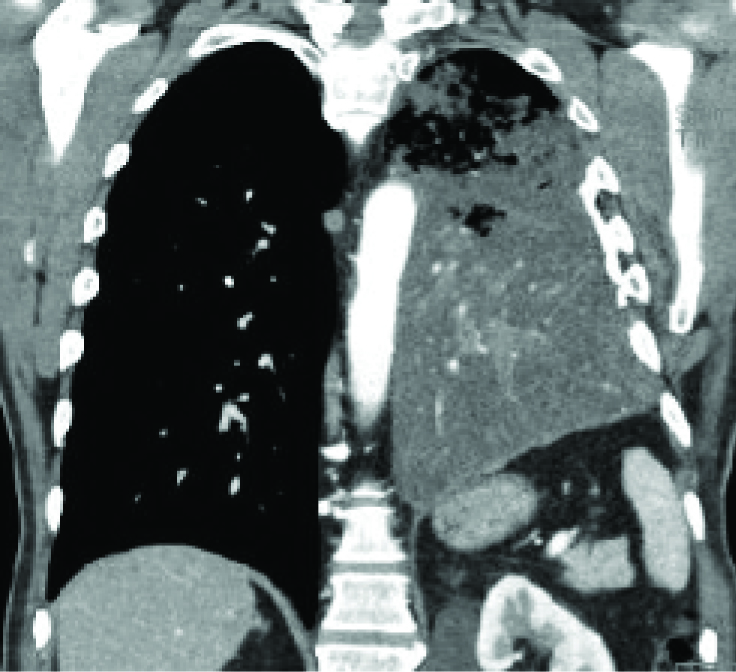
Though, right lung parenchymal involvement could not be completely ruled out, based on PET/CT if present it would be none to minimal. As such lung adenocarcinoma causing complete opacification of the hemithorax with none to minimal involvement of the contralateral lung parenchyma is rare [2] and to our knowledge, this is the first reported case. Based on the presentation, a mucinous lung adenocarcinoma with lepidic growth was suspected, representing synchronous tumor with a heterogenous population of tumor cells [3].
[1]. Ordonez NG, Value of the MOC-31 monoclonal antibody in differentiating epithelial pleural mesothelioma from lung adenocarcinomaHum Pathol 1998 29(2):166-69. [Google Scholar]
[2]. Travis WD, Garg K, Franklin WA, Wistuba II, Sabloff B, Noguchi M, Evolving concepts in the pathology and computed tomography imaging of lung adenocarcinoma and bronchioloalveolar carcinomaJ Clin Oncol 2005 23(14):3279-87. [Google Scholar]
[3]. Cadioli A, Rossi G, Costantini M, Cavazza A, Migaldi M, Colby TV, Lung cancer histologic and immunohistochemical heterogeneity in the era of molecular therapies: analysis of 172 consecutive surgically resected, entirely sampled pulmonary carcinomasAm J Surg Pathol 2014 38(4):502-09. [Google Scholar]