Paraquat (1,1’-dimethyl-4,4’-bipyridium dichloride) ingestion is a major cause of fatal poisoning in many parts of Asia and Pacific nations [1]. Death in paraquat poisoning is either due to significant lung injury or multiorgan failure [2]. The commonest mode of poisoning with paraquat is oral intake of poison. Toxicological analysis of plasma and urine samples is used to establish the diagnosis. Mortality rate of paraquat poisoning is directly related to plasma and urine paraquat concentrations. In the initial stages of paraquat poisoning, haemoperfusion is the preferred mode of therapy in treating these patients as it is primarily excreted by the kidneys [3]. Paraquat clearance is more effective with haemoperfusion than with haemodialysis [4]. As per a study done by Pond and Tominack et al., using a canine model of paraquat poisoning, it was recommended that, charcoal haemoperfusion was effective only if it could be initiated within two hours of paraquat injection or within four hours of paraquat ingestion [5,6]. As per a study done by Hsu et al., which included 207 severely paraquat poisoned patients, it was found that, early haemoperfusion in these patients reduced the mortality [7]. In a multicentric study done by Li et al., it was found that, early haemoperfusion decreased the paraquat blood levels and also increased survival in these patients [8]. Antioxidants with N-acetyl cysteine were found to be less effective in the treatment of paraquat poisoning. This study was chosen to know the effectiveness of early haemoperfusion therapy and also to know the survival outcomes in severe paraquat poisoning.
Materials and Methods
We conducted a retrospective study in the Department of Internal medicine, Kasturba Medical College, Manipal, between January 2012 to December 2015 after taking approval from the Institutional Ethics Committee. The case sheets and treatment charts of all the patients who were hospitalized with paraquat poisoning were reviewed. All the data were analysed anonymously. Paraquat poisoned patients who were more than 18 years of age and who arrived at the emergency triage within 24 hours after ingestion and had urine paraquat test to be positive were included in this study. Patients with paraquat poisoning were excluded from this study if they had pre-existing renal or liver disease or if they had left against medical advice. All the patients who were hospitalized underwent the following tests: renal function test, liver function test, prothrombin time, arterial blood gas analysis, chest X-ray and urine paraquat. Reagents used for urine paraquat testing were 0.5 ml of strong ammonia and 20 mg of sodium dithionite powder. If the mixture of these reagents to urine turned blue, urine paraquat was considered to be positive. In all the patients, the time duration between the time of ingestion of poison and commencement of therapy was noted. All the paraquat poisoned patients received treatment with 1g/kg of activated charcoal through the nasogastric tube following gastric lavage with normal saline in the emergency triage. Haemoperfusion was initiated in all these patients soon after the arrival of urine paraquat result. We defined early haemoperfusion therapy as initial haemoperfusion ≤ 6 hours after paraquat ingestion and late haemoperfusion therapy as initial haemoperfusion > 6 hours after paraquat ingestion. There were few patients who did not undergo haemoperfusion therapy due to financial constraints. They were only treated with activated charcoal, N-acetyl cysteine and anti-oxidants. These patients were included in this study to know the efficacy of haemoperfusion therapy in paraquat-poisoned patients. Renal function test and liver function test were repeated every alternate day after starting therapy. Patients who had abnormal renal function test i.e., serum creatinine> 2 mg/dl, abnormal liver function test i.e., alanine transaminase (ALT) > 80U/L and/or International Normalized Ratio (INR) > 1.5 were defined as having multiorgan failure. Patients who had PaO2 < 70 mmHg by arterial blood gas analysis at room air were defined as having acute lung injury secondary to paraquat poisoning.
Haemoperfusion is a method of filtering the blood outside the body to remove a toxin. As with other methods, such as haemodialysis, peritoneal dialysis, haemofiltration and haemodiafiltration, the blood travels from the patient into a machine, gets filtered, and then travels back into the patient typically by venovenous access (out of a vein and back into a vein). In haemoperfusion, the blood perfuses a filter composed of artificial cells filled with activated carbon or another microporous material. Small molecules in solution within the serum (such as the toxin) cross the membranes into the microporous material and get trapped there in, but formed elements (the blood cells) brush past the artificial cells just as they brush past each other. In this way, the microporous material’s filtering ability can be used without destroying the blood cells. Two types of haemoperfusion is commonly used:
1) Charcoal haemoperfusion: which has been used to treat liver failure, various types of poisoning and certain autoimmune diseases when coated with antigens or antibodies.
2) Certain resins (such as polystyrene) are frequently more efficient at clearing lipidsoluble drugs than charcoal haemoperfusion.
Outcome Measurement
We assessed the survival of paraquat-poisoned patients and stratified the patients according to the timing of haemoperfusion/gastric lavage with activated charcoal therapy. The outcome measurement was patient mortality. Each surviving patient was followed for at least 60 days at the Inpatient Wards or Outpatient Departments.
Statistical Analysis
Data was summarized in frequency and percentages. Continuous variables were expressed using mean, median and standard deviation. Associations were studied using paired sample t-test and chi-square test. A p-value of < 0.05 was considered significant. Data was analysed using SPSS software version15.
Results
A total of 101 patients with paraquat poisoning were included in the study. All of them were suicidal cases who had ingested a 24% liquid paraquat concentrate. As shown in [Table/Fig-1], the mean age of the paraquat poisoned patients was 26±7.679 years with a median age of 26 years. Approximately, 65% of the paraquat poisoned patients were males and 35% were females. Approximately, 62% of the patients underwent haemoperfusion therapy and 38% of the patients received treatment in the form of only gastric lavage. The latter group could not afford haemoperfusion therapy due to financial constraints. Mortality was seen in 61.4% of the paraquat-poisoned patients after treatment (including both haemoperfusion group and gastric lavage only group).
Baseline characteristics of the subjects.
| Baseline characteristics (n=101) |
|---|
| Variable | Result |
|---|
| Age (Mean±SD) | 26.97±7.679 |
| Gender | |
| Male | 66 (65.3%) |
| Female | 35 (34.7%) |
| Mode of treatment | |
| Haemoperfusion | 63 (62.4%) |
| Gastric lavage | 38 (37.6%) |
| Outcome | |
| Survived | 39 (38.6%) |
| Expired | 62 (61.4%) |
As shown in [Table/Fig-2], the clinical outcome of the patient was compared with the mode of treatment i.e., gastric lavage only or haemoperfusion. We found that, survival rate was higher in patients who underwent haemoperfusion compared to those who received gastric lavage only as a therapy i.e., 57.1% vs. 7.9% respectively. This was statistically significant, indicating that, haemoperfusion can improve survival outcome in these patients.
Comparison of the outcome with the mode of treatment.
| Mode of Treatment | Outcome | Total | p-value |
|---|
| Survived | Expired |
|---|
| Gastric lavage | 3 (7.9%) | 35 (92.1%) | 38 (100%) | < 0.0001 |
| Haemoperfusion | 36 (57.1%) | 27 (42.9%) | 63 (100%) |
| Total | 39 (38.6%) | 62 (61.4%) | 101 (100%) |
Chi-square test applied
As shown in [Table/Fig-3], the clinical outcome was compared with time elapsed to haemoperfusion. Here we found that, the survival rate was higher in patients who underwent haemoperfusion in ≤ 6 hours compared to those who received haemoperfusion therapy after 6 hours i.e., 93.9% vs. 13.8% respectively. This was statistically significant, suggesting that, early haemoperfusion therapy could improve the chances of survival in severely paraquat-poisoned patients.
Comparison of the outcome with the time elapsed to haemoperfusion.
| Time elapsed tohaemoperfusion | Outcome | Total | p-value |
|---|
| Survived | Expired |
|---|
| ≤ 6 hrs | 31(93.9%) | 2(6.1%) | 33(100%) | < 0.0001 |
| > 6 hrs | 4(13.8%) | 25(86.2%) | 29(100%) |
| Total | 35(56.5%) | 27(43.5%) | 62(100%) |
Chi-square test applied
Paired Sample t-test was used to compare the change in the means of parameters {serum creatinine in mg/dl, ALT in IU/ml and INR} on day 1 and day 3, separately among patients who received gastric lavage and haemoperfusion. The difference in the mean value on day 1 and day 3 was higher in patients who received gastric lavage when compared to those who received haemoperfusion with all the parameters i.e. serum creatinine, ALT and INR as shown in [Table/Fig-4].
Comparison of means of parameters on day 1 and day 3 in both groups.
| Mode of Treatment | Parameters | Mean | Standard Deviation | Mean Difference |
|---|
| Gastric lavage | Serum creatinine day 1 | 0.85 | 0.22 | -2.5 |
| Serum creatinine day 3 | 3.35 | 1.86 |
| ALT day 1 | 25.95 | 9.6 | -216.79 |
| ALT day 3 | 242.74 | 246.1 |
| INR day 1 | 1.06 | 0.06 | -0.65 |
| INR day 3 | 1.71 | 0.59 |
| Haemoperfusion | Serum creatinine day 1 | 0.84 | 0.19 | -1.6 |
| Serum creatinine day 3 | 2.44 | 2.22 |
| ALT day 1 | 20.17 | 8.11 | -142.83 |
| ALT day 3 | 163.0 | 231.44 |
| INR day 1 | 1.03 | 0.05 | -0.46 |
| INR day 3 | 1.49 | 0.64 |
* Paired Sample t-test applied
** The mean was statistically significant with p-value <0.0001
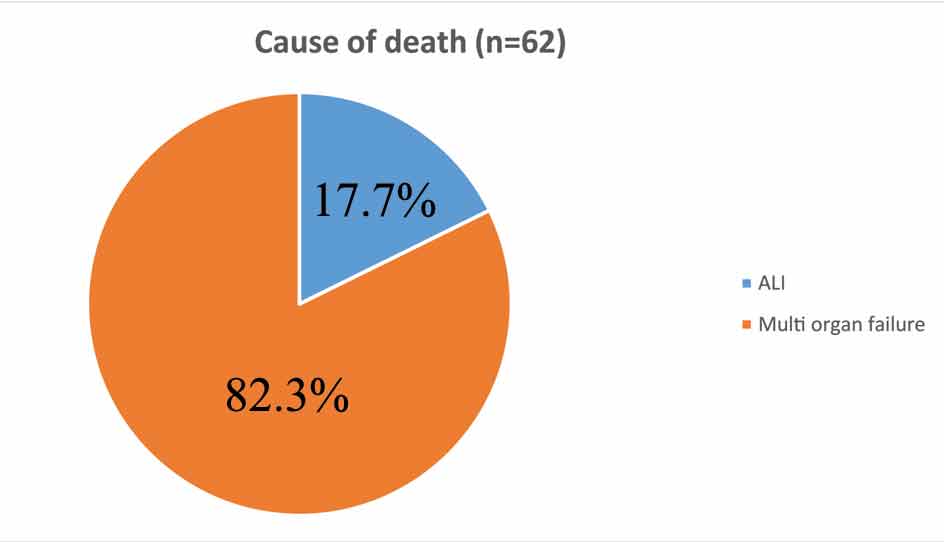
As shown in [Table/Fig-5], out of 62 patients who died, 51(82.3%) died due to multiorgan failure and 11(17.7%) patients died due to Acute Lung Injury (ALI). This shows that multiorgan failure is the most common cause of death in patients with severe paraquat poisoning.
Pie chart showing the cause of death in paraquat poisoned patients.
ALI- Acute Lung Injury
Discussion
Paraquat poisoning is of greater toxicological importance in Southern India as it is widely used as an herbicide here. The fatality rate of paraquat poisoning in our hospital was found to be approximately 61%. In hospital case, fatality rate ranges between 35-62% in the world which is consistent with our study [9,10]. The mean age of paraquat poisoned patients was found to be approximately 26 years in our study which was comparable to a study done by Tanuj Kanchan et al., where the mean age was found to be approximately 30 years [11]. The reason for suicidal intent with paraquat poison among the youth may be due to its easy availability and its wide use as an herbicide. In our study, paraquat poisoning was more commonly associated with males. Haemoperfusion is the most effective modality for clearing paraquat and detoxifying the poison [12,13]. The survival rate was approximately 8% in the group which did not receive haemoperfusion compared to 57% in the haemoperfusion group, indicating that haemoperfusion improves the survival rate in paraquat poisoned patients. It was quoted by Cavalli RD et al., that the survival rate in patients without active treatment was only 13% even with non fatal dose ingestion of paraquat poison and it increased to more than 50% with active treatment modality like haemoperfusion, in patients with fatal dose consumption [13]. Combined therapy with haemoperfusion and Continuous VenoVenous Haemofiltration (CVVH) increased the survival duration in patients with acute paraquat poisoning, as per a study [14]. CVVH as alone therapy was found to be beneficial in reducing the mortality as per a study done recently [15]. In our study, we found that, early haemoperfusion (≤ 6 hours) improved the survival rates compared to those who received late haemoperfusion (>6 hours). In a study done recently by Hsu CW et al., it was found that, early haemoperfusion improved the survival outcomes in paraquat poisoned patients [7]. The mortality exceeds 50% in paraquat poisoned patients even with immunosuppressive therapy suggesting that it is inadequate [16]. Haemoperfusion doubled the systemic clearance of paraquat suggesting that it could be implemented as a treatment strategy in patients with paraquat poisoning [17]. Some studies found that, haemoperfusion was not useful which might have been due to potentially lethal concentration of paraquat getting accumulated in highly vascular tissues of the vital organs and pneumocytes before the initiation of haemoperfusion [6]. The peak time of plasma paraquat is 1-3 hour, that of lung cells is 4-5 hour and nearly 9% of the paraquat disappears in the plasma 5-6 hour after ingestion [4]. Hence, the patients who receive early haemoperfusion are likely to be benefited due to significant removal of the amount of paraquat from the blood. This indirectly reduces the amount of paraquat getting accumulated in the lung cells also, thereby, improving the outcome.
Limitation
This study was not a placebo controlled trial. The amount of paraquat poison consumed was not always available from the case sheet. The mortality in paraquat poisoning is directly proportional to plasma and urine paraquat concentrations. It couldn’t be done due to non availability. The severity of paraquat poisoning was only based on sodium dithionite test on urine (change of colour to blue). The clinical and kinetic effect of haemoperfusion is better determined by prospective studies which may help in clearly defining the indications for this intervention.
Conclusion
The results showed that early haemoperfusion after paraquat ingestion was effective in reducing mortality in severely poisoned patients. Hence, it should be considered as a therapy and also initiated immediately especially when the patient arrives early with history of paraquat poisoning.
Chi-square test applied
Chi-square test applied
* Paired Sample t-test applied
** The mean was statistically significant with p-value <0.0001