Eosinophilic granuloma is basically a disorder of reticuloendothelial system and is one of the variants of langerhans cell histiocytosis. Multifocal eosinophilic granuloma affecting jaws and skull is relatively a rare disorder. We hereby report a case of multifocal eosinophilic granuloma involving mandible, maxilla and several skull bones. The present case has mixture of classical floating teeth appearance and an unusual radiographic/imaging finding of periosteal remodeling, which is rarely seen in adult patients of eosinophilic granuloma and pseudo-multilocular appearance in anterior mandibular region in coronal sections and moth-eaten appearance of skull was appreciated in axial slices of Computed Tomography (CT).
Computed tomography, Langerhans cell histiocytosis, Multilocular
Case Report
A 37-year-old male patient reported with a chief complaint of loosening of teeth in lower front teeth region since three years. Patient gave a history of trauma to the left skull and left mandibular body region five years back in a road traffic accident. Following the trauma patient did not observe any changes related to his medical and dental health. Patient underwent extraction of teeth no #36,37 due to mobility four months back. The rest of the missing teeth i.e., teeth no #25,26,35,43,45,46 got exfoliated a year back. Patient’s past medical history was non-contributory. Extraoral examination revealed no abnormality. Intraoral examination revealed flattening of mandibular left and right posterior alveolar ridges with unhealed sockets in mandibular left posterior region. The gingiva and other mucosal areas did not exhibit any abnormalities. The mucosa covering the residual ridges of mandible appeared as if it was ulcerated due to unhealed sockets in the missing teeth in mandibular left posterior region [Table/Fig-1a]. On palpating the lingual aspect of mandibular left posterior region a bony hard swelling was appreciable, which corresponded to the periosteal reaction in the occlusal radiograph. The residual ridge of mandibular right posterior region appeared to be flattened. However, the mucosa covering the same appeared normal [Table/Fig-1b]. The teeth in mandible and maxillary left posterior region were grade II mobile.
Intraoral photograph showing unhealed sockets in the mandibular left posterior region (black arrow).

Intraoral photograph showing atrophied right mandibular posterior edentulous ridge covered with normal mucosa (black arrow).

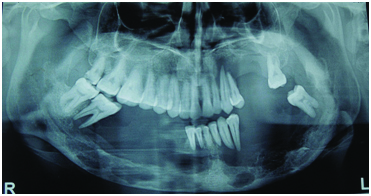
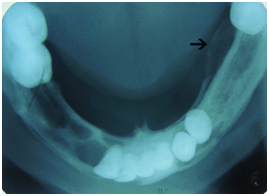
Panoramic radiograph [Table/Fig-1c] revealed extensive well defined osteolytic lesions involving complete mandibular arch (except for the mid-symphyseal region) and left maxillary posterior region. The maxillary sinuses appeared normal except for thinning of inferior border of left maxillary sinus. Complete dissolution of alveolar bone in these regions with no trace of lamina dura gave floating teeth appearance. Osteolytic lesions not only involved alveolar regions but also extended to basal bone region of mandible involving the inferior border of mandible in few areas. The lesion on the left mandible extended 1 cm posteriorly and superiorly into the ascending ramus of mandible. True mandibular occlusal radiograph [Table/Fig-1d] revealed periosteal new bone formation involving lingual cortex of left mandibular posterior region along with multiple osteolytic lesions involving the entire length of mandible.
Panoramic radiograph showing multiple lytic lesions affecting the whole mandibular arch and maxillary left posterior region. Floating teeth appearance is clearly evident.
Occlusal mandibular radiograph showing periosteal remodeling (black arrow) involving left mandibular lingual cortex. (left to right)
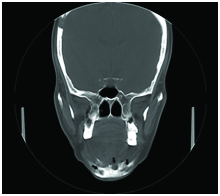
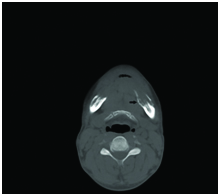
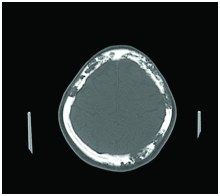
Coronal [Table/Fig-2a,b] and axial [Table/Fig-2c,d and e] sections of CT revealed multiple osteolytic lesions involving mandible, maxilla and several skull bones. The osteolytic lesions of mandible involved the entire body region which were well defined, presenting with pseudo-multilocular appearance in the anterior region of the mandible appreciated in coronal sections of CT. The lingual cortex of left mandibular region revealed periosteal bone remodeling. Bone destruction in maxilla was restricted to the left quadrant involving the region from left maxillary canine to left second molar. The right quadrant of maxilla was spared from any involvement. Sections of skull revealed bilateral involvement of parietal, temporal and occipital bones revealing a moth-eaten appearance in certain sections.
Coronal sections of CT showing multiple osteolytic lesions of skull. [Table/Fig-2b]: Pseudo multilocular appearance observed in the mandibular anterior region (black arrows).
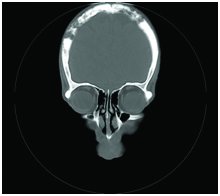
Pseudo multilocular appearance observed in the mandibular anterior region (black arrows).
Axial section of mandible showing periosteal reaction involving the lingual cortex of left mandibular posterior region (black arrow).
Destruction of left maxillary alveolus is evident.
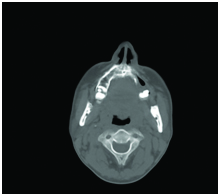
Moth-eaten appearance of skull is appreciated. (left to right)
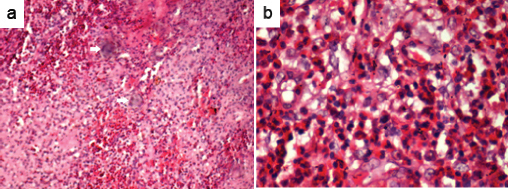
A skeletal radiographic survey was done to rule out involvement of other bones and was found to be negative. Based on the clinical and radiographic findings a provisional diagnosis of eosinophilic granuloma was considered. Differential diagnosis of vanishing bone disease was considered. Patient’s serum calcium and alkaline phosphatase levels were within normal limits. Patient was subjected to incisional biopsy in the mandibular anterior region after extracting 33 and 34 through their socket regions. Tissue sections were stained with Hematoxylin and Eosin (H&E) stains. Histopathological examination of the biopsied specimen revealed proliferation of histiocytes like cells in sheets with multinucleated giant cells. Focal collections of eosinophils were seen in the loosely arranged fibrous connective tissue with numerous blood vessels. The lesion was covered by stratified squamous epithelium with pseudo- epitheliomatous hyperplasia [Table/Fig 3a,b]. These histopathological findings were suggestive of eosinophilic granuloma.
Hematoxylin and eosin stained histopathological sections (10x and 40x) showing presence of histiocytes, eosinophils and multi-nucleated giant cells (white arrows).
A final diagnosis of multifocal eosinophilic granuloma was considered for the present case on the basis of correlation of clinical, radiological and histopathological findings.
Discussion
Langerhans cells are bone marrow precursors of myeloid series [1]. The pathological proliferation of these cells is referred to as langerhans cell histiocytosis [2,3]. Aetiology remains unknown although recent evidence suggests that it could be a manifestation of immunological aberrations [2]. Lieberman and his group in 1969 had proposed eosinophilic granuloma to be regarded as a separate and distinct entity which could present either as a unifocal lesion or as a multifocal process. Eosinophilic granuloma is characterized by focal proliferation of abnormal histiocytes plus collection of eosinophils with resultant tissue destruction [4]. We hereby report a case of multifocal eosinophilic granuloma affecting the jaws and several skull bones with a mixture of classical and some unusual radiographic/imaging findings. Our case is unique since it exhibited some unusual imaging findings like pseudo-multilocularity involving mandibular anterior region and moth eaten appearance involving various skull bones. Moreover, though periosteal reaction is not an uncommon finding in eosinophilic granuloma, radiographic demonstration in the jaw bones is not readily available in the previous literature, which is clearly demonstrated in the occlusal radiograph of the present case.
Eosinophilic granuloma is characterized by single or multiple skeletal lesions occurring mainly in children and young adults with predominance in males [5]. However, our case was a middle aged adult. Aetiopathogenesis of eosinophilic granuloma is poorly understood.
Pain, mobile teeth, facial asymmetry, sensory disturbances, cervical lymphadenopathy, swelling are some of the features of clinical presentation [6,7]. Various organs such as lungs, spleen, lymph nodes, liver and bone marrow could be involved [7]. Mobile teeth and occasional tooth pain were the only findings in our patient. However, we could also clinically appreciate the atrophied ridges involving mandibular posterior regions, which were considered to be secondary to extensive osteolytic process of eosinophilic granuloma.
Based on site of involvement and extent, radiographically, eosinophilic granuloma of jaws are categorized into alveolar, intraosseous and mixed types [5]. The present case belonged to the mixed category as the osteolysis extended from the alveolar crest till the inferior border of mandible. Apart from extensive osteolytic lesions involving jaws and skull, various other radiographic patterns/appearances were observed in the present case, such as floating teeth appearance, periosteal remodeling, pseudo-multilocular appearance and moth- eaten appearance. Radiographic features of eosinophilic granuloma could be at times non specific mimicking odontogenic cysts, osteomyelitis, periodontal disease, malignancy etc., [2].
Floating teeth appearance is a common radiographic finding in eosinophilic granuloma, which was observed in the present case associated with multiple regions of the jaws. Conditions with such similar appearance are seen in malignancies, severe periodontal disease, papillon-lefevre syndrome etc., [8].
Periosteal reactions provide an indication of Biologic activity, usually observed in young children and young adults [9]. A periosteal reaction was observed in the present case in lingual aspect of left mandibular posterior region which is an unusual finding in eosinophilic granuloma for a middle-aged adult.
Coronal sections of mandibular anterior region revealed a multilocular appearance, which was considered to be a conglomerate of multiple osteolytic lesions placed adjacent to each other leading to a pseudo-multilocular appearance. Multilocularity in the present case does not appear to be due to septa or new bone formation separating the locules.
Various skull bone involvement was observed in axial sections of CT, that lead to the description of moth-eaten appearance, that is multiple areas of bone destruction separated by normal islands of skull bone.
Histologically, our case demonstrated all the classical features of eosinophilic granuloma reported in the literature [9] like histiocyte proliferation, presence of multi-nucleated giant cells and eosinophils in loosely arranged fibrous connective tissue.
Treatment of eosinophilic granuloma depends on the severity of the disease. Surgery, curettage, local irradiation and chemotherapy have all been used alone or in combination with favorable results [6,10]. Intraosseous corticoid therapy can be administered for recalcitrant cases [11]. Spontaneous healing is also observed in some multifocal cases. Prognosis of eosinophilic granuloma is poor with extraosseous involvement such as lungs [10]. Our patient did not undergo any treatment due to personal reasons.
Conclusion
Combination of various radiographic patterns described in our case has not been reported earlier. Our case exhibits complete clinical, radiological and histopathological illustrations with emphasis on CT findings. The unusual clinical and radiographic/imaging findings of the present case could provide a clue for oral radiologists to include multifocal eosinophilic granuloma as one of the differential diagnosis when rendezvoused with features similar to this case.
[1]. Hicks J, Flaitz CM, Langerhans cell histiocytosis: Current insights in a molecular age with emphasis on clinical oral and maxillofacial pathology practiceOral Surg Oral Med Oral Pathol Oral Radiol Endod 2005 100(2):S42-66. [Google Scholar]
[2]. Schepman KP, Radden BG, Van der Waal I, Langerhans’ cell histiocytosis of the jaw bones. Report of 11 casesAustr Dent J 1998 43(4):238-41. [Google Scholar]
[3]. Roychoudhury A, Shah N, Parkash H, Mukhopadhyay S, Chopra P, Eosinophilic granuloma of the jawsBr J Oral Maxillofac Surg 1998 36(5):380-3. [Google Scholar]
[4]. Krutchkoff DJ, Jones CR, Multifocal eosinophilic granuloma: clinical pathologic conferenceJ Oral Pathol 1984 13:472-88. [Google Scholar]
[5]. Li Z, Li ZB, Zhang W, Li JR, Wang SP, Cheng Y, Eosinophilic granuloma of the jaws: An analysis of clinical and radiographic presentationOral Oncol 2006 42:574-80. [Google Scholar]
[6]. Ardekian L, Peled M, Rosen D, Rachmiel A, Abu el-Naaj I, Laufer D, Clinical and radiographic features of eosinophilic granuloma in the jaws: A review of 41 lesions treated by surgery and low-dose radiotherapyOral Surg Oral Med Oral Pathol Oral Radiol Endod 1999 87:238-42. [Google Scholar]
[7]. Shi S, Liu Y, Fu T, Li X, Zhao S, Multifocal langerhans cell histiocytosis in an adult with a pathological fracture of the mandible and spontaneous malunion: A case reportOnco Lett 2014 8(3):1075-9. [Google Scholar]
[8]. Muppa R, Prameela B, Duddu M, Dandempally A, Papillon-lefevre syndrome: A combined approach from the dermatologist and dentist - A clinical presentationIndian J Dermatol 2011 56:740-43. [Google Scholar]
[9]. Yu Q, Wang PZ, Shi HM, Wang L, Sun DX, Radiographic findings in Langerhans’ cell disease affecting the mandibleOral Surg Oral Med Oral Pathol Oral Radiol Endod 1995 79:251-54. [Google Scholar]
[10]. Kessler P, Wiltfang J, Schultze-Mosgau S, Neuman FW, Langerhans cell granulomatosis: A case report of polyostotic manifestation in the jawInt J Oral Maxillofac Surg 2001 30(4):359-61. [Google Scholar]
[11]. Watzke IM, Millesi W, Kermer C, Gisslinger H, Multifocal eosinophilic granuloma of the jaw: Long-term follow-up of a novel intraosseous corticoid treatment for recalcitrant lesionsOral Surg Oral Med Oral Pathol Oral Radiol Endod 2000 90(3):317-22. [Google Scholar]