The special sensory organs play significant role in our daily lives. Until one of them is totally or partially lost, its real value is not fully appreciated. The most tragic, yet common loss of sensory organ is that of an eye. Restoration of unilateral ocular defects is very challenging for a maxillofacial prosthodontist and requires great skill to mimic bilateral eye. Restoration of bilateral defects using customized eye prosthesis presents even more difficult task for clinician especially in communication with patient, impression procedures, and patient education regarding insertion, removal and maintenance of prosthesis. Such loss of eyes may have a tremendous emotional and psychological impact on the patient. This article presents a technique for fabrication of bilateral ocular prosthesis of completely blind patient.
Case Report
A 23-year-old male patient reported to Department of Prosthodontics, with a chief complaint of vision loss in both eyes. Patient gave history of typhoid fever nine years back following which he gradually lost his vision. On ophthalmologic examination, it was found that the patient was having bilateral retinal atrophy [Table/Fig-1(a)]. On inspection, it was found that volume of right eye was completely lost whereas, the left eye still retained some of its volume. The patient was motivated for the treatment and an ocular prosthesis for right eye and thin scleral shell prosthesis for the left eye was planned for the patient.
Technique:
Impressions: A custom tray with stem was fabricated by making the impression of the closed eye with help of irreversible hydrocolloid material (Neocolloid, Zhermack) which was then adjusted according to the patient’s socket and relief holes were prepared [Table/Fig-1(b)]. To this custom tray stem, a syringe was attached to act as a medium to carry the impression material into the atrophied socket of the patient [Table/Fig-1(c)].
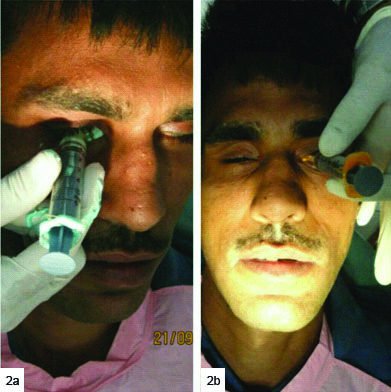
Irreversible hydrocolloid material (Neocolloid, Zhermack) was used for making impression of the right atrophied socket. The material was mixed in thin consistency and was loaded into the syringe to which custom tray was attached. The custom tray was inserted into the right socket of the patient and the material was injected from the syringe which flowed into the socket of the patient. Patient was asked to make the movements like looking up, down, right and left so as to record all the borders of the socket. After the material was set, custom tray along with the syringe was carefully taken out of the socket and the impression was inspected for any irregularity. Patient complained of slight irritation with alginate so the impression of the left socket was made with help of light body vinyl polysiloxane material (Aquasil, Dentsply) after which patient did not complain of any discomfort [Table/Fig-2].
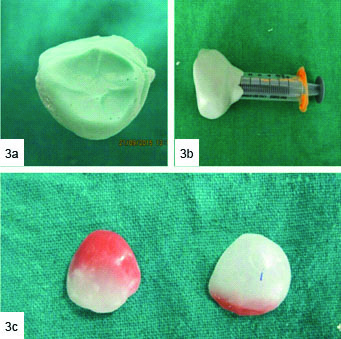
Wax Pattern Fabrication: After the impressions of both the sockets were completed [Table/Fig-3(a)], a mould using putty consistency vinyl polysiloxane material (Aquasil, Dentsply) was made around the impressions into which the molten white carving wax was flowed so as to make the wax patterns [Table/Fig-3(b)]. After the wax was completely set, the wax patterns were retrieved from the putty mould, modified and tried on patient. Addition and removal of wax was done until the desired bulge and contours were obtained in both the open and closed positions of the eyelids [Table/Fig-3(c)].
Wax Pattern Trial: The smoothened and finished patterns were tried for proper fit, contour, orientation and adaptation. Three lines were marked on the patient’s face. One in centre of forehead between the eyebrows, second on the outer canthus and third on the middle of the two lines. Same lines were marked on the contralateral side also. These lines helped to mark the middle of the pupil of the eye which helped in iris orientation. During this marking, patient was asked to look straight. Patient was then asked to close the eyes passively and any discomfort on closing the eyelids was noted and corrected and bilateral symmetry was checked [Table/Fig-4a,b].
a) Showing preoperative view of the patient showing atrophied eye sockets; b) Showing the custom tray; c) Showing the stem of custom tray to which syringe is attached.

Showing impression of right and left eye.
a) Showing the impression of the socket; b) Showing the putty mould for fabrication of wax pattern and; c) Showing the fabricated wax patterns.
a) Showing the wax pattern trial; b) Showing the bilateral symmetry.

a) Showing the wax patterns with iris buttons; b) Showing iris orientation.

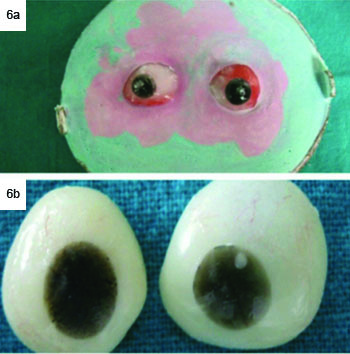
a) Shows flasking of wax patterns; b) Shows cured eye shells.
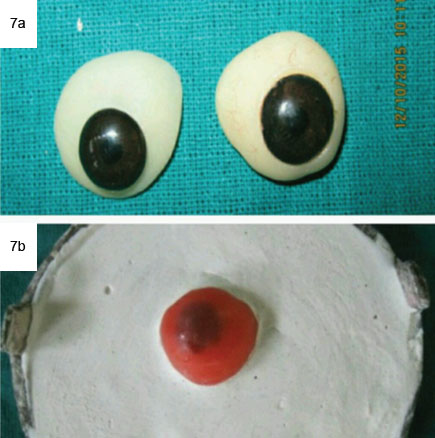
a) Shows iris selected from prefabricated eye shells; b) Shows single thickness wax adapted for uniform thickness clear acrylic resin.
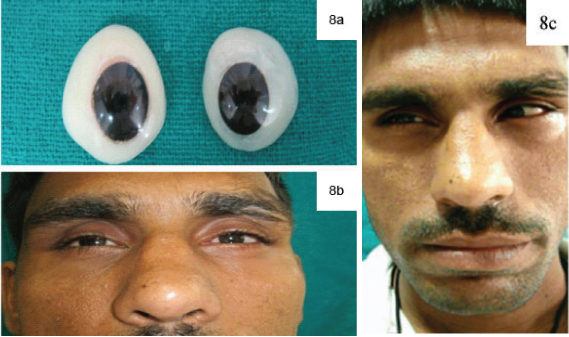
a) Shows final finished prosthesis; b) Shows postoperative view of the patient; c) Patient showing movements of eyes.
Iris Orientation: It was done by attaching the Iris buttons to wax pattern In desired position [Table/Fig-5(a)]. These Iris buttons were fabricated using the clear autopolymerising resin (DPI, India) to which black paint was added to give it black colour. Iris orientation was done such that the stem of the buttons should point 1000 medio-inferiorly to the middle of the eye while patient tried to look straight In upright position [Table/Fig-5(b)].
Flasking and Packing of Wax Patterns: The finished wax pattern after Iris orientation with the iris buttons in place was invested In flask using dental stone (Kalstone type III, Kalabhai) after applying appropriate separating media between the two pours [Table/Fig-6(a)]. Dewaxing was performed In usual manner as done for complete denture fabrication. Heat cure tooth coloured polymethymethacrylate material (DPI, India) was mixed according to manufacturer’s Instructions and packed In the flask and left for bench curing overnight to enable complete polymerization and prevention of any excess unreacted monomer. Long curing cycle (10000C for 8 hours) was used so as to prevent the presence of any residual monomer in the prosthesis which is very essential. It prevents any untoward irritation or sensitivity to tissues and thereby rejection of the prosthesis by the patient.
Characterization: The cured ocular shells were retrieved from the flask, finished and polished. Then characterization was done on these finished shells using the coloured fibres from high strength heat cure acrylic material (Lucitone, Dentsply), which mimicked the blood vessels of the eye. These fibres were retained using a thin layer of clear autopolymerising resin monomer liquid, (DPI, India) which was applied over these fibres and was left to dry [Table/ Fig-6(b)].
Iris Placement: Two prefabricated eye prosthesis were selected with uniform Iris colour and diameter. Iris portion was cut carefully and was adjusted over the cured shell. It was tried In the patient’s eye to check for proper orientation and complete passive eyelid closure. Single thickness wax was adapted over the cured shell and was flasked using dental plaster (Kalstone type II Kalabhai) [Table/Fig-7(a,b)]. After the plaster was set, the flask was opened and the single thickness wax was removed and clear heat cure acrylic polymer and monomer (DPI, India) was mixed following manufacturer’s Instructions and was packed In dough consistency, followed by standard processing procedures. Deflasking was done and eye prosthesis was retrieved.
Finishing and Polishing: Eyes are very sensitive to Irritation. Any irregularity In eye prosthesis would lead to discomfort and can affect the patient compliance. So, finishing and polishing was done giving It a glass like finish and taking care no Irregularity exists on Intaglio and polished surface [Table/Fig-8(a)]. It was Inserted in the eye socket carefully by reflecting the eyelids and all the contours were verified and analyzed for any areas that required any adjustment [Table/Fig-8(b)].
Patient was able to make left to right and up down movements with the prosthesis without any discomfort [Table/Fig-8(c)]. Periodic recall appointments on second and fifth day after Insertion and once In every month for six months were scheduled. Patient was trained to Insert and remove the prosthesis. As the patient was bilaterally blind, so he was Instructed to read the contours of the prosthesis with his fingers and differentiate between the right and left as the left prosthesis was just a thin scleral shell.
Post Insertion Instructions were given to the patient as well as the care taker regarding the wearing, removal and care of prosthesis at home:
Prosthesis should be handled with care and with clean hands.
The prosthesis should be removed during night.
For surface disinfection, the prosthesis should be dipped in antibacterial solution.
To prevent protein and bacterial deposition, routine polishing of the prosthesis should be done.
Discussion
Eyes are the most characteristic and noticeable feature of face. Loss of an eye Is not only physical but also emotional, social and psychological loss to the patient. Ocular defects may be congenital, associated with tumours, or acquired lesions and may affect the tissues within the orbital cavity or the surrounding facial structures [1,2]. Replacing the lost eye as soon as possible is necessary for physical and psychological healing of the patient [3].
With help of surgical means such as evisceration (removal of intraocular contents of globe), enucleation (removal of globe and parts of optic nerve), exenteration (removal of entire orbital contents) the loss of an eye can be managed [4]. Prosthetic rehabilitation of such defect is done by using ocular prosthesis which can be retained either by natural undercuts of the lids or by adhesive methods or Implants.
Most unilateral eye loss patients are satisfied, depending on how well the prosthetic components resemble the true opposing natural site [4]. However, when the patient Is having bilateral loss of eyes, there is no point of reference for clinician and patient to determine and assess colour of prosthesis.
Since unilateral defects are most commonly seen in majority of cases, bilateral defects are rarely treated [5]. It was a challenge to achieve the harmony between prosthesis and surrounding structures In this case, since the underlying damage had created two different treatment sites [4]. Individual Impressions of both the eyes were made separately as separate prosthesis was planned for both the eyes. While stock eyes are cheap, and readily available In identical sets, custom made ocular prosthesis based on two separate Impressions offer better adaptation to the tissues, mobility, enhanced aesthetics and facial contours [2]. Differentiation between the right and the left prosthesis Is of utmost importance for the patient. Some mechanical marking can help the patient to locate their eye units. In this case, prosthesis for left eye socket was thin as compared to the right, so the patient could easily differentiate between the two. As the prosthesis maintained its orientation during function, patient could perform the eye movements comfortably.
Prosthetic rehabilitation of lost eye can be done with use of prefabricated and custom made eye prosthesis. In this case report, custom made eye prosthesis was chosen over prefabricated one as it has better fit, adaptation and patient comfort [6].
Customised eye prosthesis have become a predictable mode of treatment with advent of newer impression materials and processing techniques which can be fabricated with exact fit and aesthetics. Although, retention of eye prosthesis can be enhanced with the use of implants, but they are not always possible or feasible due to surgical and financial constraints [6]. In this case report, successful prosthetic rehabilitation of completely blind patient was done using customized eye prosthesis.
The literature reviewed regarding prosthetic rehabilitation of completely blind patients with eye prosthesis concluded that the unilateral rehabilitation with prosthetic eye is quite common but rehabilitation of eyes bilaterally is rarely seen and only a few reports and series have been published in literature [4,5,7,8].
Conclusion
It is a great challenge for the clinician to rehabilitate the patient with bilateral loss of eyes. To achieve the desired results, it is important for the clinician to give clear verbal commands to the patient, so as to carry out the clinical procedure successfully and to make the patient understand about insertion, removal and maintenance of prosthesis. Customized ocular prosthesis were fabricated in this case, as they are better option than prefabricated stock eyes in terms of aesthetics, comfort and provide a better fit, which definitely gives the patient a psychological elevation and higher self confidence.
[1]. Goiato MC, Mancuso DN, Marcal Mazza Sundefeld ML, Da Motta Gabriel MB, Murakawa AC, Guiotti AM, Aesthetic and functional ocular rehabilitationOral Oncology EXTRA 2005 41:162-64. [Google Scholar]
[2]. Aeran H, Kumar V, Dhami R, The characterized occular prosthesis-An innovative approachClinical Dentistry 2015 6(9):20-26. [Google Scholar]
[3]. Aggarwal A, Sharma A, Singh K, Gupta A, Scleral prosthesis: An eye for an eye: A case reportIndian Journal of Dental Sciences 2013 5(5):63-65. [Google Scholar]
[4]. Hatemleh M, Haylock C, Hollows P, Richmond A, Watson J, Prosthetic eye rehabilitation and management of completely blind patientInt J Prosthodont 2012 25:631-35. [Google Scholar]
[5]. Blaylock W, Johnston S, Hughes M, Bilateral evisceration: A case reportJournal of Ophthalmic Prosthetics 2005 10(1):1-5. [Google Scholar]
[6]. Somkuwar K, Mathai R, Jose P, Ocular prosthesis: Patient rehabilitationPeople’s Journal of Scientific Research 2009 21(2):21-26. [Google Scholar]
[7]. Pruthi G, Jain V, Light weight prosthesis for a patient with bilateral orbital exenterationJ Prosthodont Res 2013 57(2):135-39. [Google Scholar]
[8]. Pruthi G Jain V, Rajendiran S, Jha R, Prosthetic rehabilitation after orbital exenteration: A case seriesIndian J Ophthalmol 2014 62(5):629-32. [Google Scholar]