Case Report
A 40-year-old non-diabetic Indian female visited the outpatient department as a referred case from the Department of Orthopaedics of a private hospital. She presented with complaints of pain in right hip for two months. The pain was aggravated on walking, climbing stairs and was associated with a limp. There was no fever, cough or any history of weight loss. Courses of painkillers and physiotherapy had made no difference to her pain. There was an alleged history of the fall from stairs about four months back, for which she had taken treatment at a local hospital, details of the same were not available, but she was given some painkillers and bed-rest for a week after which she had recovered completely. However, there was no history of infectious or any joint diseases to the patient or any close contacts.
On examination, the right hip joint was warm and tender with slight adduction and fixed flexion deformity at 30o with further flexion possible till 90o. Lumbar lordosis was present and Thomas test was positive. There were no sinuses or crepitus associated with the right hip joint. But there was an apparent shortening of the right limb. On measuring the same from anterior superior iliac spine to medial malleolus the shortening was missing. There was no associated lymphadenopathy. Besides, the rest of the physical and local examinations including that of spine and knee were normal. Also, the neurological and peripheral vascular examination of lower limbs was normal.
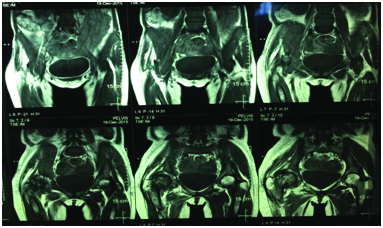
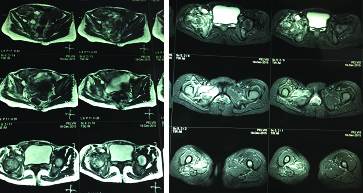
The patient underwent anteroposterior radiograph of pelvis with both hips, which was suggestive of flattening of the right head of femur with sclerosis of right femur head and right acetabulum roof along with reduced joint space in the right hip joint thus giving an impression of degenerative changes in the right hip joint [Table/Fig-1]. Ultrasonogram (USG) of the pelvis was suggestive of a solid cystic lesion about 4.8x3.7 cm in the right adnexa with few cystic changes. A thick septa was noted along with vascularity within it. Also, a mild amount of fluid was seen in the pouch of Douglas. The chest radiograph (P-A view) was normal. Routine blood investigations including HIV and HBsAg were within normal limits except Erythrocyte Sedimentation Rate (ESR) of 75 mm in the first hour and Total Leucocyte Count (TLC)-12000/cumm, C-Reactive Protein (CRP) was positive (89.7mg/l). She was advised Magnetic Resonance Imaging (MRI)-pelvis with both hip joints which was suggestive of an osseous destruction with altered (oedematous) marrow signal intensity involving the right femoral head and neck, acetabular cup and iliac bone appearing hyperintense on STIR and T2W images and iso-hypointense on T1W images with irregularity of the articular margins, cortical erosions, along with decreased superior-medial joint space and significant periosteal reaction. Also, variable sized loculated collections were seen in right iliacus, gluteal and obturator muscles. The altered signal intensity of the surrounding muscles with myofascial oedema in right obturator internus muscle was noted [Table/Fig-2,3]. Besides, a complex right adnexal cystic lesion of about 3.6x2.5 cm was also noted. The rest of the pelvis was normal with no degenerative changes. The patient underwent a biopsy and the tissue samples were sent for staining for acid-fast bacilli, microscopy, culture, and sensitivities from an accredited National Reference Laboratory (NRL). After 15 days, under standard conditions at the NRL cultures were confirmed to have grown Mycobacterium tuberculosis on Lowenstein Jensen medium. In-line probe assay (GenoType MTBDR plus, Hain Life Science, Nehren, Germany), the isolate, was identified as Mycobacterium tuberculosis and was sensitive to all standard antitubercular medications except isoniazid and rifampicin by Bactec MGIT (Mycobacteria Growth Indicator Tube) 960 system. Further on second line Drug Susceptibility Testing (DST) resistance to kanamycin and ofloxacin were also reported. Thus, a diagnosis of primary extensively drug resistant TB of the right hip joint was made and the patient was started on the standard Category V Antitubercular Therapy (ATT) as per the Programmatic Management of Drug Resistant TB (PMDT) guidelines involving the capreomycin, moxifloxacin, pyrazinamide, ethambutol, linezolid, clofazimine, PAS, amoxicillin-clavulanate (augmentin) and pyridoxine.
Anteroposterior radiograph of pelvis with both hips, suggestive of degenerative changes in the right hip joint.

MRI of the pelvis: T1-weighted, coronal view suggestive of an osseous destruction.
MRI of the pelvis: T1-weighted, axial view- suggestive of an osseous destruction with altered (oedematous) marrow signal intensity involving the right femoral head and neck, acetabular cup and iliac bone with irregularity of the articular margins, cortical erosions, along with decreased superior-medial joint space and significant periosteal reaction.
Presently, the patient has been on Category V ATT since last six months with regular follow ups in the orthopaedics and TB clinics and has been transferred-out to her native place at her request. Besides, the patient was also referred to a gynaecologist for the management of the right adnexal mass. A written informed consent was obtained from the patient for the publication of the case details and any accompanying images.
Discussion
TB is a major cause of death due to infectious diseases and is caused by an airborne infection by Mycobacterium tuberculosis. TB has become a major public health problem in developing countries [1]. The situation is grave in these countries due to rapidly multiplying population, poor health expenditure, poverty and corruption. The issue of drug resistant TB (DR-TB) came to limelight since the year 1990 [2].
The DR-TB can be multidrug resistant (MDR-TB), extensively drug resistant (XDR-TB) or totally drug resistant TB [3]. XDR-TB, is defined as resistance to isoniazid and rifampin (i.e., MDR-TB) plus additional resistance to a fluoroquinolone and a second-line injectable agent (kanamycin, amikacin or capreomycin) [3]. Usually the DR-TB cases are commonly seen in the previously treated cases of TB [4]. However, reports of primary MDR-TB and XDR-TB are also available, but these are only sparse [4–6].
Till date report of primary extensively drug resistant TB of the hip joint in an immunocompetent female has not been reported in literature. We herein present the first case of primary XDR-TB of the right hip joint in an HIV-negative Indian female.
The skeletal TB constitutes less than 10% of the total TB cases [7]. The cases of TB of the hip are second only to the spine and constitute 15-20% of the total musculoskeletal TB cases [8]. The infection ordinarily begins amid initial three decades; however, no age is resistant [8]. The reports of DR-TB of the hip joints are sparse and are available mainly as case reports [6]. However, primary XDR-TB of the hip joint in an immunocompetent female has never been reported earlier. The present case is unique as there is no history of TB to the patient or any close contacts. Also, the patient was well nourished, belonged to a well to do family and thus a high index of suspicion was required to diagnose such a case. Saraf SK et al., 2015, reported that the diagnosis is often delayed in the TB hip cases [8]. The endemicity of TB in India could well be a major contributor to such primary extrapulmonary XDR-TB case. The present case will serve as a tool to the clinicians to suspect a DR-TB in endemic countries, even in the absence of prior history or contact of TB, especially when the number of DR-TB cases is rising.
TB of the hip commonly presents as pain in the hip, limp, and restriction of joint movements [8]. On the basis of the extent of involvement there can be deformity, sinuses, shortening of the limb, pathological dislocations, and swelling [8]. The detailed clinical manifestations are described elsewhere by Saraf SK et al., [8]. The differential diagnosis includes transient synovitis of the hip, rheumatoid arthritis, Legg-Calve-Perthes disease, injury hip, osteomyelitis of the upper end of the femur, acute infective arthritis of infancy and childhood, osteoid osteoma of the neck of the femur with synovial involvement, Avascular Necrosis (AVN) of the head of the femur, villonodular synovitis, giant cell variants of upper femur, etc., [8]. The plain radiographs have been considered as the primary investigation of choice and the basis to start the treatment, especially in the resource poor endemic countries [8,9]. However, the radiographs in the early stages of the disease are inconclusive [8]. Thus, the role of biopsy and when possible the advanced diagnostic modalities like MRI are imperative [8]. The MRI is a sensitive, but not a specific diagnostic technique for the TB hip [8]. In short, the best diagnostic modality in endemic countries is a plain radiograph of the hip [8]. However, in countries where TB is not endemic the MRI of the hip with or without biopsy is indicated [8]. The tissue obtained from the afflicted site must be sent for histology, AFB staining, PCR and also for culture and sensitivity. Singhal O et al., opined that arthroscopic synovial biopsy gives a definitive diagnosis of various joint ailments, especially where clinical diagnosis is ambiguous [10,11].
The treatment in extrapulmonary DR-TB cases like XDR-TB basically involves the use of antitubercular drugs based on the sensitivity of the organism. Regular follow-ups in the orthopaedics OPD are advised [8]. Sandhu HS et al., 1983, reported recuperating from illness in 98% of cases by advocating ATT and traction [8,12]. The role of Total Hip Arthroplasty (THA) in the hip with active TB is a dubious issue because of the potential danger of reactivation of TB and has been detailed elsewhere [8,13]. Saraf SK et al., suggested ATT and traction alone, with or without an arthrotomy and surgical debridement that could result in early resolution of the disease [8]. The duration of XDR-TB treatment is around 24-30 months and is associated with high pill burden, daily drug intake, highly toxic anti-TB drugs having multiple adverse drug reactions, etc., [14]. Thus, regular counselling of the patients to adhere to the treatment till completion is important [14]. The role of creating awareness about TB in endemic countries is also very important and the efforts targeted at the population at-risk should be increased. The agencies involved in the dissemination of the healthcare information to the masses should play an active and important role, especially in resource constrained settings [15].
Conclusion
The case emphasizes the importance of a thorough clinical evaluation with high index of suspicion in the endemic countries as most of such cases are often late in presentation and are difficult to diagnose on the commonly available cheaper investigation modalities like radiographs. The management relies on the phase of clinical presentation and the seriousness of destruction as evident radiologically. From a conservative therapy with ATT and traction to debridement and joint replacement, a number of surgical procedures have been detailed.
[1]. Mohajan HK, Tuberculosis is a fatal disease among some developing countries of the worldAmerican Journal of Infectious Diseases and Microbiology 2015 3(1):18-31. [Google Scholar]
[2]. Pablos-Méndez A, Raviglione MC, Laszlo A, Binkin N, Rieder HL, Bustreo F, Global surveillance for antituberculosis-drug resistance, 1994-1997. World Health Organization-International Union against Tuberculosis and Lung Disease Working Group on Anti-Tuberculosis Drug Resistance SurveillanceN Engl J Med 1998 338(23):1641-49. [Google Scholar]
[3]. Types of Drug Resistant TB – MDR and XDR TB. Available from: http://www.tbfacts.org/types-of-drug-resistant-tb/. Accessed 2016 on June 21 [Google Scholar]
[4]. Yadav S, Rawal G, Primary extrapulmonary multidrug-resistant tuberculosis of the sternum without HIV infectionJ Clin Diagn Res 2016 10(1):RD01-RD03. [Google Scholar]
[5]. Yadav S, Rawal G, Primary extrapulmonary multidrug-resistant tuberculosis in an immunocompetent child presenting with pleural effusionTransl Pediatr 2016 doi: 10.21037/tp.2016.07.01 (Ahead of print) [Google Scholar]
[6]. Dorjee K, Dierberg KL, Sadutshang TD, Reingold AL, First report of multi-drug resistant tuberculosis in a systemic lupus erythematosus patientBMC Res Notes 2015 8:337 [Google Scholar]
[7]. Talbot JC, Bismil Q, Saralaya D, Newton DA, Frizzel RM, Shaw DL, Musculoskeletal tuberculosis in Bradford - A 6-year reviewAnn R Coll Surg Engl 2007 89(4):405-09. [Google Scholar]
[8]. Saraf SK, Tuli SM, Tuberculosis of hip: A current concept reviewIndian J Orthop 2015 49(1):1-9. [Google Scholar]
[9]. Tuli SM, General principles of osteoarticular tuberculosisClin Orthop Relat Res 2002 398:11-19. [Google Scholar]
[10]. Midiri M, Filosto L, Lo Casto A, Masciocchi C, Magnetic resonance in the study of tubercular coxitisRadiol Med 1992 83:38-42. [Google Scholar]
[11]. Singhal O, Kaur V, Kalhan S, Singhal MK, Gupta A, Machave Y, Arthroscopic synovial biopsy in definitive diagnosis of joint diseases: An evaluation of efficacy and precisionInt J Appl Basic Med Res 2012 2(2):102-06. [Google Scholar]
[12]. Sandhu HS, Kalhan BM, Dogra S, Shanmughasundaram TK, Management of tuberculosis of the hip jointCurrent Concepts in Bone and Joint Tuberculosis 1983 147EVR Periyar Road, Madras, India [Google Scholar]
[13]. Kim SJ, Postigo R, Koo S, Kim JH, Total hip replacement for patients with active tuberculosis of the hip: A systematic review and pooled analysisBone Joint J 2013 95-B(5):578-82. [Google Scholar]
[14]. Vasisht AK, Yadav S, Role of a counselor in the management of multidrug-resistant TBIndian Journal of Immunology and Respiratory Medicine 2016 1(1):23-24. [Google Scholar]
[15]. Yadav S, Rawal G, Healthcare information for all-Is it achievable?Int J Sci Res Rev 2015 4(1):101-05. [Google Scholar]