Intracoronal Radiolucency in An Unerupted Premolar: A Rare Occurrence
Neil De Souza1, Anna Vaz2, Paul Chalakkal3
1 Lecturer, Department of Paedodontics and Preventive Dentistry, Goa Dental College and Hospital, Bambolim, Goa, India.
2 General Practitioner, Charisma Dental Centre, Panjim, Goa, India.
3 Assistant Professor, Department of Paedodontics and Preventive Dentistry, Goa Dental College and Hospital, Panjim, Goa, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Paul Chalakkal, Assistant Professor, Department of Paedodontics and Preventive Dentistry, Goa Dental College and Hospital, Panjim-403202, Goa, India.
E-mail: atomheartpaul@yahoo.com
Pre-eruptive Intracoronal Resorption (PIR) is a lesion that mostly occurs within the dentin in the occlusal part of the crown, next to the dentin-enamel junction. Such lesions are usually detected accidentally, on routine intraoral radiographs. This case report highlights a case of PIR detected in the mandibular second premolar of a 10 year old boy. The radiographic finding, size, position and restoration of the defect have been mentioned.
Caries, Defect, Pre-eruptive, Radiograph
Case Report
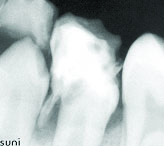
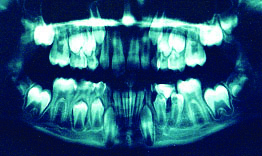
A 10-year-old male patient reported to the Department of Paedodontics and Preventive Dentistry, with a chief complaint of fracture in a tooth. Clinically, a coronal fracture was observed in tooth #75 (primary mandibular left second molar). Radiographic examination revealed completion of mesial root resorption and partial crown resorption in relation to tooth #75. It also revealed a well circumscribed radiolucent lesion; involving the coronal aspect of tooth #35 (mandibular left second premolar) [Table/Fig-1]. A provisional diagnosis of PIR was made after the lesion was observed on the Orthopantomograph (OPG) as well [Table/Fig-2]. Since, there was no associated discomfort or pain in relation to tooth #75, no treatment was carried out and physiological exfoliation of tooth #75 was expected to take place. After three months, ectopic eruption of tooth #35 was observed intra-orally [Table/Fig-3], following which tooth #75 was extracted under local anaesthesia. A brownish defect without pulpal exposure, measuring 0.5cm in diameter, was observed in the mesial coronal region of tooth #35, involving the marginal ridge [Table/Fig-4]. The defect was restored using posterior composite (P-30™, 3M Company, St Paul, MN) restoration [Table/Fig-5]. Twelve months post operatively, the patient was asymptomatic and tooth #34 (mandibular left first premolar) had erupted intra-orally without any visible defect [Table/Fig-6,7].
IOPA radiograph showing resorbed tooth #75, overlying tooth #35 with PIR.
OPG showing resorbed tooth #75 and tooth #35 with PIR.
Ectopically erupted tooth #35 due to over retained tooth #75.

Brownish defect in tooth #35.

Composite restoration in tooth #35.

After eruption of tooth #34.

OPG showing tooth #34 and tooth #35 after completion of eruption at tooth 12 months follow up.

Discussion
PIR often occurs within the dentin, adjacent to the dentin-enamel junction, in the occlusal aspect of the crown [1–4]. Since PIR resembles caries, it is often referred to as “pre-eruptive caries” [3]. Various prevalence rates such as 3% [5], 3-6% [6], 6% [7], 8.1% [8], 15.1% [9] and 27.3% [10] have been reported based on subject, and 0.5% [5], 0.5-2% [6], 0.62% [8], 2% [7], 2.1% [10], 3.5% [9] and 3.9% [11] have been reported based on teeth. Most cases of PIR have been discovered during the mixed dentition [7,8], although, Umansky et al., found none in the age group between 6-8 years [11]. The condition was found to be more common in males (57%) than in females (43%) [9]. However, some studies found no significant gender differences [7,8,10] PIR was found to be more common in teeth in the lower arch [8,9] and the descending order of occurrence is as follows; mandibular first molars (4%) > mandibular first premolar (2%) > then the mandibular second molar (1%) > mandibular second premolar (1%) > maxillary first molar (1%) > maxillary first premolar (1%) > maxillary second premolar (0.2%) [7]. Two studies had found PIR to occur most frequently in the third molar [9,11]. Seow WK et al., Al-Batayneh OB et al., Nik NN and Abul Rahman R found PIR to mostly occur in first permanent molars, mandibular first premolars and maxillary first premolars, respectively [5,8,10]. It has also been found to occur in teeth succedaneous to decayed or filled primary teeth [8]. Mostly PIR was found to occur in a single location in any tooth [5,10], similar to the PIR in this case report. The mesial location of the PIR in this case is similar to the finding by Al-Batayneh et al., who found most of the lesions to occur mesially [8]. Half or more of the PIR in two studies were found to extend till less than one-third the width of dentin thickness [8,10]. However, Seow et al., had found half of all the lesions to extend beyond two-third the width of dentin thickness [5], similar to the finding in this case report. In any patient, a single tooth was found to be most commonly affected by PIR (74% or 88.7%), followed by two (10.9% or 25%) or three teeth (0.7% or 2%) [7,10]. Internal resorption has been suggested as the cause for PIR [6]. Osteoclasts, multinucleated giant cells, macrophages and scalloped borders have been found in PIR, that probably enter the developing tooth from the surrounding bone or through breaks in the dental follicle or enamel epithelium [7,12]. However, Moskovitz and Holan had questioned the sole involvement of internal resorption, since they had discovered a lesion that had not increased in size even after seven years [4]. Other aetiologies such as ectopic positioning [5,7], external resorption [12] and origin from developmental pits on the occlusal surface [12], have also been suggested. Many have suggested that the aetiology and pathogenesis of the lesion remains unclear [1,4,6]. However, in this case, ectopic eruption of tooth #35 had occurred. Small, pre-eruptive lesions can be radiographically monitored until the tooth erupts, followed by its restoration [4,13,14]. Large lesions approaching the pulp may be restored as soon as possible with indirect pulp capping [3]. However, for very large progressive lesions, the tooth may be restored in its unerupted state after removal of the overlying primary tooth [7,13,14]. For these reasons, all permanent teeth must be analyzed for PIR radiographically, prior to their eruption [15], since their prognosis depends on early detection and treatment [1]. Various forms of treatment have been carried out for PIR by authors, based on the permanent tooth involved [Table/Fig-8].
Treatment of PIR by authors.
| Authors | Tooth | Treatment undertaken |
|---|
| Lenzi et al., [15] | Third molar | Extraction |
| Brunet-Llobet et al., [2] | Second molar | Pulp-like tissue under the crown was retrieved and analyzed. The tooth was extracted due to extensive resorption. |
| Wong and Khan [16] | Second molar | Extraction |
| Davidovich et al., [3] | Second molar | Initial restoration with glass-ionomer cement. After 3 months, amalgam restoration was done following partial pulpotomy. |
| Czarnecki et al., [17] | First molar | Restored with glass ionomer sealant. |
| McNamara et al., [12] | Molar | Extracted |
Conclusion
Among all PIR occurrences, the prevalence of its occurrence in a mandibular second premolar is about 1%. This makes our finding a rare one. Paediatric dentists are often the first to detect such lesions on intraoral radiographs; therefore, awareness of PIR amongst them is important.
[1]. Omar S, Choi J, Nelson B, Shin M, Chen JW, Pre-eruptive intracoronal resorption (PEIR): Literature review and case reportJ Calif Dent Assoc 2015 43(5):255-60. [Google Scholar]
[2]. Brunet-Llobet L, Lahor-Soler E, Miranda-Rius J, Oral pain due to severe preeruptive intracoronalresorption in permanent toothEur J Paediatr Dent 2014 15(3):332-4. [Google Scholar]
[3]. Davidovich E, Kreiner B, Peretz B, Treatment of severe pre-eruptive intracoronal resorption of a permanent second molarPediatr Dent 2005 27(1):74-7. [Google Scholar]
[4]. Moskovitz M, Holan G, Pre-eruptive intracoronal radiolucent defect: A case of a nonprogressive lesionJ Dent Child (Chic) 2004 71(2):175-8. [Google Scholar]
[5]. Seow WK, Lu PC, McAllan LH, Prevalence of pre-eruptive intracoronal dentin defects from panoramic radiographsPediatr Dent 1999 21(6):332-9. [Google Scholar]
[6]. Seow WK, Pre-eruptive intracoronal resorption as an entity of occult cariesPediatr Dent 2000 22(5):370-6. [Google Scholar]
[7]. Seow WK, Wan A, McAllan LH, The prevalence of pre-eruptive dentin radiolucencies in the permanent dentitionPediatr Dent 1999 21(1):26-33. [Google Scholar]
[8]. Al-Batayneh OB, Al Jamal GA, Al Tawashi EK, Pre-eruptive intracoronal dentine radiolucencies in the permanent dentition of Jordanian childrenEur Arch Paediatr Dent 2014 15(4):229-36. [Google Scholar]
[9]. Demirtas O, TarimErtas E, Dane A, Kalabalik F, Sozen E, Evaluation of pre-eruptive intracoronal resorption on cone-beam computed tomography: A retrospective studyScanning 2016 [Google Scholar]
[10]. Nik NN, Abul Rahman R, Pre-eruptive intracoronal dentin defects of permanent teethJ ClinPediatr Dent 2003 27(4):371-5. [Google Scholar]
[11]. Umansky M, Tickotsky N, Friedlander-Barenboim S, Faibis S, Moskovitz M, Age related prevalence of pre-eruptive intra-coronal radiolucent defects in the permanent dentitionJ Clin Pediatr Dent 2016 40(2):103-6. [Google Scholar]
[12]. McNamara CM, Foley T, O’Sullivan VR, Crowley N, McConnell RJ, External resorption presenting as an intracoronal radiolucent lesion in a pre-eruptive toothOral Dis 1997 3(3):199-201. [Google Scholar]
[13]. McEntire JF, Hermesch CB, Wall BS, Leonard DL, Case report–pre-eruptive intracoronalresorptionOper Dent 2005 30(4):553-6. [Google Scholar]
[14]. Holan G, Eidelman E, Mass E, Pre-eruptive coronal resorption of permanent teeth: Report of three cases and their treatmentsPediatr Dent 1994 16(5):373-7. [Google Scholar]
[15]. Lenzi R, Marceliano-Alves MF, Alves FR, Pires FR, Fidel S, Pre-eruptive intracoronal resorption in a third upper molar: Clinical, tomographic, and histological analysisAust Dent J 2016 Jul 29 doi10.1111/adj.12444 [Google Scholar] [CrossRef]
[16]. Wong L, Khan S, Occult caries or pre-eruptive intracoronal resorption? A chance finding on a radiographPediatr Dent 2014 36(5):429-32. [Google Scholar]
[17]. Czarnecki G, Morrow M, Peters M, Hu J, Pre-eruptive intracoronal resorption of a permanent first molarJ Dent Child (Chic) 2014 81(3):151-55. [Google Scholar]