A full veneer crown or full veneer fixed partial dentures are important restorations in the armamentarium of restorative dentist. These restorations not only reinforce endodontically treated teeth or replace missing teeth but also maintain sound integrity of stomatognathic system in terms of aesthetics, function and health. Marginal fit/marginal accuracy plays a crucial role in long term success of these restorations because an inadequate adaptation of the prosthesis in relation to its abutment internally or at the finish lines lead to vertical and horizontal discrepancies that are not only detrimental to underlying tooth but also to the surrounding periodontium culminating into promotion of bacterial and plaque deposition leading to secondary caries, bone loss and complete failure of the prosthesis. Intimate adaptation at margins is influenced by multiple parameters such as geometry of tooth preparation, finish line characteristics, fabrication procedures, underlying cementing medium etc. Even with profound use and acceptance of Computer aided Design and Computer Aided Manufacturing CAD/CAM, traditional methods of fabrication of metal substructure/copings prior to ceramic build up with lost wax process has not been completely eliminated, this procedure is routinely used and is a cheaper alternative to machined milled copings. One of the potential sources of error in the fabrication of a fixed prosthesis is the die material used during the lost wax process. Glossary of Prosthodontic terms (Edition-8) defines a die as “The positive reproduction of the form of a prepared tooth in any suitable substance”. A number of materials are currently available, yet none of these satisfy all desirable qualities of a die system [1]. International Organisation for standardization (ISO) recognised Type IV [high strength] and V [high strength, high expansion] improved stones are most commonly used die materials, due to their perceived dimensional accuracy, low cost and ease of use. On the other hand, rough surfaces at the margins are difficult to clean subgingivally and chronically inflamed gingivae is susceptible to long-term periodontal breakdown [2]. The design of tooth preparations can affect the success of individual restorations, tooth preparation for porcelain fused metal crowns is of interest due to its wide application. The porcelain fused to metal restoration presents some unique problems in its fabrication because of the possibility of an interaction between the two materials when porcelain is added to the metal coping. Preparation design can play a role in the stabilization of this process [3]. Fusayama et al., cemented full cast crowns onto extracted teeth prepared with the 900 shoulder, the 450 shoulder, and feather edge margins concluded that feather edge margin provided the best sealing effect followed by the 450 shoulder and 900 shoulder, respectively [4]. This research intended to determine influence of various finish lines and die materials on vertical marginal adaptation of porcelain fused to metal copings with an aid of a three dimensional stereomicroscope.
Materials and Method
Preparation of Standard Metal Model through CAD/CAM :
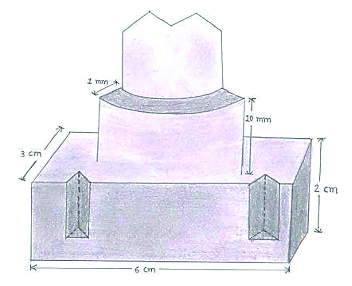
The study was conducted in Post-graduate Department of Prosthodontics, School of Dental Sciences, KIMSDU, Karad, Satara, Maharashtra, India. Two Ivorine mandibular first molars were prepared using friction grip standard diamond points medium grit (Pivo-Swiss Technology) having a diameter of 1.3mm to receive a circumferential shoulder and deep chamfer margin. The width of both the finish lines from the axial wall to the cavosurface margin was 1mm each with 60 taper. Prepared teeth were scanned using 3M Lava Optical Scanner and Contra Spray. EOS Plastic Laser Sintering System was utilised for milling of chrome cobalt (SP2:BEGO) blocks to fabricate master models of shoulder and deep chamfer margins such that distance from the base to the finish line for each of the model was 10mm. The models were welded to a rectangular base (6*3*2) fabricated from mild steel, four orientation groves were milled on the opposing walls such that two were semicircular in design and remaining two were triangular [Table/Fig-1].
1Schematic representation CAD/CAM master model with orientation grooves on mild steel base.
Preparation of Custom tray :
Two custom trays were designed using Magics software and exported to ProJet 7000 SLA 3D printer series, photosensitive light curable resin was the material of choice for fabrication of resin trays that was cured using UV light. These trays had projections corresponding to the grooves of the metal base to ensure accurate orientation and precise fit of the trays over the CAD/CAM models during impression making. The surface of the tray facing the standard metal model was perforated in order to provide a vent for excess impression material.
Fabrication of Multiple Die Models in Three Different Die Materials :
A tray adhesive (Dentsply Caulk) was applied to both custom trays, medium bodied elastomeric impression material (Aquasil Monophase, DenstplyTM was manipulated and loaded into the custom tray to make impressions for both the models guided by the orientation grooves. A total of 60 impressions were made to fabricate 60 specimens of dies [Table/Fig-2, 3 and 4] 30 samples having shoulder and 30 having deep chamfer margin goemetry.
Dies made in Type IV Gypsum.
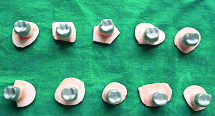
Dies made in Resin modified Gypsum.

Dies made in Epoxy resin.

Each group of 30 impressions consisted of 10 impressions poured in Type IV Gypsum (Kalrock-Kalabhai Karson Mumbai Pvt Ltd.), having a water powder ratio of 0.23 manipulated according to manufacture’s instructions, 10 impressions poured in Resin modified Gypsum (Synarock, XR, DFS, Germany), water powder ratio for the same was 0.20 and remaining 10 packed in Epoxy resin (Epoxy Compound-Pidilite Industries Ltd.) supplied with two roles of resin and hardener each, depending upon the quantity required for making a die, a small quantity of both the roles was manupilated in 1:1 ratio and condensed into the custom tray in small increments until the impression space was completely filled. Dies so confected were coated with a single layer of die spacer (Bredent-Germany). Wax patterns for the copings were carved in type II inlay wax (DFS-Germany). For its standardization, a putty index of a wax pattern measuring 0.4mm in overall thickness was fabricated [Table/Fig-5].
Putty index of standard wax pattern
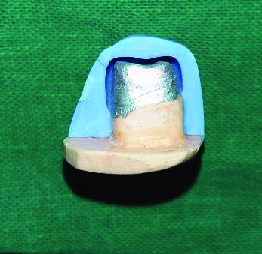
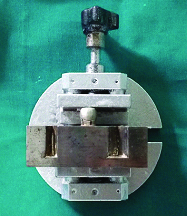
All the wax patterns were evaluated using the putty index as a guide and finally to re-adapt, the wax was reflown completely at the margins, and when the pattern had cooled the marginal excess was carved and the margin was burnished. Wax patterns were invested in phosphate bonded investment material (Wirovest) and castings were obtained through traditional lost wax process in the Centrifugal Induction Casting Machine (BEGO-Germany). Certain technical modifications must be made to ensure a proper fit with nonprecious alloys, as they are less dense and have increased shrinkage during casting. Increased investment expansion can be obtained by using concentrated silica gel solution. Castings procured were evaluated for nodules at its undersurface and fitted over their respective dies. Four points were marked on CAD/CAM model, two buccal and two lingual, castings were fitted onto their respective CAD/CAM models stabilized under a constant pressure using a vice [Table/Fig-6].
Copings stabilized under constant pressure vice
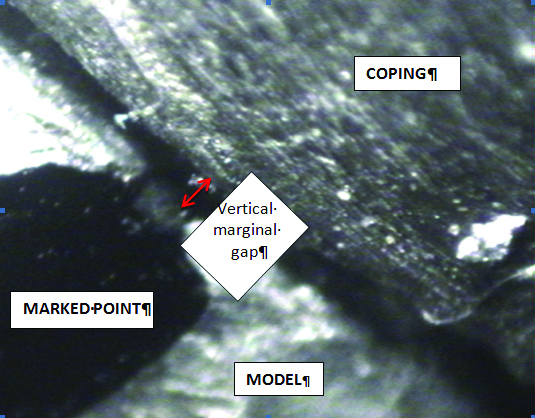
The entire assembly was set under a 3 dimensional stereomicroscope, copings were evaluated for vertical marginal discrepancy. [Table/Fig-7] is a stereomicroscopic image (10X magnification) of a coping evaluated for vertical marginal discrepancy (microns- μm) at marked point on CAD/CAM model. An average value of vertical marginal discrepancy was estimated from four points marked on each coping corresponding to that on master model. The statistical calculations were performed using the software SPSS for windows (Statistical Presentation System Software, SPSS Inc, 1999, New York) version 10.0. The following statistical methods were employed in the present study 1) Two way ANOVA test. 2) Tukeys multiple Post Hoc test.
Stereomicroscopic image representative of vertical marginal gap (10X magnification).
Results
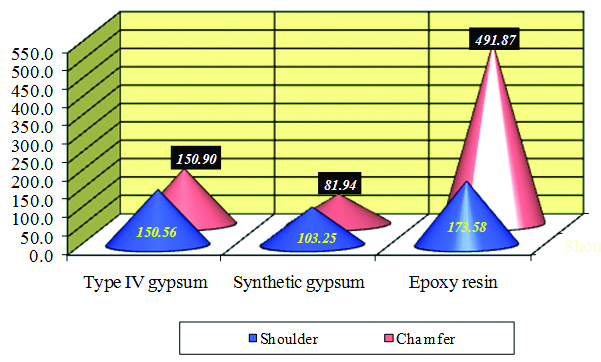
[Table/Fig-8] is tabular presentation comparing two designs (shoulder and chamfer) and three die materials (Type IV Gypsum, synthetic gypsum and Epoxy resin) with marginal gap analysed by Two way ANOVA with no significant difference between the designs. [Table/Fig-9,10] is the presentation comparing two designs (shoulder and chamfer) and three die materials (Type IV Gypsum, synthetic gypsum and Epoxy resin) with marginal gap analyzed by Tukey’s multiple Post Hoc test. The mean values of vertical gaps for copings fabricated in epoxy resin for both the finish lines was found to be beyond the normal limits (120μm) exhibiting a range of 275-534 μm.
Tabular presentation comparing two designs (shoulder and chamfer) and three die materials (Type IV Gypsum, synthetic gypsum and Epoxy resin) with marginal gap analysed by Two way ANOVA.
| Sources of Variation | Degrees of Freedom | Sum of Squares | Mean sμm of Squares | F-value | p=value |
|---|
| Main effects |
| Designs | 1 | 146989.75 | 146989.75 | 31.3870 | 0.075 |
| Materials | 2 | 595602.75 | 297801.38 | 63.5901 | 0.00001* |
| 2-way interactions |
| Designs × Materials | 2 | 394288.25 | 197144.13 | 42.0966 | 0.00001* |
| Error | 54 | 252889.54 | 4683.14 | | |
| Total | 59 | 1389770.29 | | | |
* p<0.05
Tabular presentation comparing two designs (shoulder and chamfer) and three die materials (Type IV Gypsum, synthetic gypsum and Epoxy resin) with marginal gap analysed by Tukey’s Post Hoc analysis.
| Designs × Materials | Shoulder with Synthetic Gypsum | Shoulder with Type IV Gypsum | Shoulder with Epoxy Resin | Chamfer with Type IV Gyp sum | Chamfer with Synthetic Gypsum | Chamfer with Epoxy Resin |
|---|
| Mean | 150.56 | 103.25 | 173.58 | 150.90 | 81.94 | 491.87 |
| SD | 45.24 | 45.94 | 50.22 | 45.94 | 39.50 | 133.22 |
| Shoulder with Type IV gypsum | | | | | | |
| Shoulder with synthetic gypsum | p=0.6369 | | | | | |
| Shoulder with Epoxy resin | p=0.2129 | p=0.9742 | | | | |
| Chamfer with type IV gypsum | p=0.6369 | p=0.9999 | p=0.9742 | | | |
| Chamfer with Synthetic Gypsum | p=0.9816 | p=0.2361 | p=0.0453* | p=0.2361 | | |
| Chamfer with Epoxy Resin | p=0.0001* | p=0.0001* | p=0.0001* | p=0.0001* | p=0.0001* | |
* p<0.05
10 Graphical representation of test samplesfabricated on three groups of die shaving shoulder and chamfer finish line plotted against their mean values of vertical marginal gap.
Discussion
Long term success of full veneer crowns and bridges is multifactorial, most important criterion to evaluate clinical acceptability of cast restorations is marginal fit. Both vertical and horizontal discrepancies promote plaque accumulation detrimental to adjoining periodontium. Horizontal discrepancy affects hygiene maintenance, vertical discrepancy is associated with cement dissolution, microleakage and concomitant tooth and periodontal damage. Therefore the aim of afore described study was to evaluate vertical misfit only. Horizontal discrepancy in indirect microscopic assessment cannot be evaluated. Also, to measure the internal gap, cementation and sectioning of specimens is inevitable. With wide range of commercially available die materials, such as type IV and V Gypsum products, synthetic gypsum, Epoxy resin, and metallic resins, Amalgam dies, Metal sprayed dies, copper and silver plated dies, most commonly used is Type IV dental stone because of its low expansion, high resistance to compression, satisfactory hardness and excellent ability to reproduce details, although some concerns have been observed during handling. One of these concerns is gypsum is a water-based material [5,6]. The water-powder ratio is an important factor because its alteration can increase the porosity and decrease the strength of the stone [7,8]. Alternatives to gypsum include resin-impregnated gypsum, Epoxy resin, and polyurethane resin exhibit superior abrasion and rupture resistance with superior detail reproduction [9]. Conversely, volumetric shrinkage of resin die materials that occurs during polymerization has reduced their widespread recognition [10]. Although, Type IV resin-impregnated die materials are dimensionally more stable than conventional Type V dental stone, a research study found no significant differences between conventional gypsum and Type IV resin-impregnated stone [11]. Volumetric shrinkage in Epoxy resin die materials is in range of 0.1–0.4%, and a study relates this material has improved dimensional accuracy over Type IV and V resin-impregnated gypsum materials [12]. The null hypothesis tested was that, epoxy resins would behave in similar manner to Type IV dental stone and resin modified synthetic gypsum in terms of dimensional accuracy at the margins when utilized to fabricate metal ceramic copings of varied margin designs. The two finish lines opted were shoulder and deep chamfer which exhibit edequal influence on margin accuracy, either of these finish lines can be used to fabricate metal ceramic restoration. The mean values of vertical gaps in dies fabricated in epoxy resin for both the finish lines was found to be beyond the normal limits exhibiting a range of 275-534μm. On the other hand, mean value of vertical marginal gaps with respect to Type IV Gypsum and synthetic gypsum were comparable to the average value (80-200μm). Gulker et al., stated that even good castings often exhibit discrepancies of 200 μm, but others have reported much smaller discrepancies [13]. Dedmon discovered that prior to cementation only 9% of castings had sealing discrepancies greater than 39μm [14]. However, according to Christensen, the least acceptable visually accessible marginal discrepancy is 39 μm [15,16]. Palomo and Peden have emphasized that the mean opening for gingival margins in Christensen’s study was 74 μm, and that this was a more realistic dimension to evaluate gingival margin acceptability [17]. Ostlund considered that subgingivally openings less than 50 μm might be acceptable [18], while others felt that discrepancies exceeding 100 μm were unacceptable [19,20].
Although some maintain that sharp explorers detect marginal gaps as small as 25μm [21], McLean and Von Fraunhofer reported that discrepancies less than 80μm were difficult to detect under clinical conditions [15]. For various reasons, they considered that successful restorations possessed marginal gaps less than 120μm whatever baseline [Table/Fig-10] is used for assessing marginal discrepancies, cervical margins remain the most difficult to restore and finish. Bjorn et al discovered that 83% of gold and 74% of porcelain crown margins exhibited approximal defects, with over half of these defects greater than 0.2mm [21]. Schwartz et al., cited defective margins as a frequent cause (11.3%) of unserviceable crowns and Fixed Partial Dentures (FPD) [22], while Grasso et al., reported that 30 % to 40 % of crown margins were inadequate, often because of poor marginal integrity. Recent studies continue to demonstrate high rates of marginal deficiencies, and indicate that defective margins are responsible for over 10% of failed units. The effect of inadequate margins to influence periodontal tissues is widely accepted, although some question the clinical significance of this interaction in terms of attachment loss [23]. Fit at the margins is expressed, as a measurement of the opening that exists between the casting and finish line, desired opening gap is expected to be in the range of 25-40μm [24]. [Table/Fig-10] is a graphical representation of six groups of copings having two finish line designs fabricated on three different die materials (n=60) on X-axis plotted against mean vertical marginal gap values on Y-axis which showed that copings fabricated on dies poured in synthetic gypsum exhibited least marginal gap followed by copings fabricated on dies poured in Type IV Gypsum. The highest value was obtained for copings fabricated on Epoxy resin dies. The reason for higher vertical discrepancy found in copings fabricated on epoxy resin dies can be attributed to the fact that dies made from epoxy resin are not dimensionally accurate, since dimensional accuracy affects the marginal adaptation. The greater vertical discrepancy has been noted in copings fabricated from epoxy resin dies irrespective of margin design. The polymerization shrinkage in resin dies is related to reactive monomers that are linked initially by Van der Waals forces with a mean distance of 4 Å in a state of minimal potential energy. After polymerization, the molecular linkages changes to covalent bond accompanied by reduction in mean distance between the molecules by 20%, contributing to significant volumetric shrinkage [26]. Thus, dies obtained from epoxy resins generally presented lower mean values, compared with those for the master model. Conversely, dies confected using Type IV stone (Dental stone group) had the tendency to expand. The process of Gypsum crystallization essentially is expansive growth of crystals from the core [25]. Interlacing of dihydrate core crystals and their growth can block the growth of adjacent crystals. If this process persists then thousands of crystals create an external tension during their growth that leads to expansion of the mass. The resultant product is larger in external volume however it is smaller in crystalline volume [26]. These characteristics of gypsum, restoration adjustments are more easily performed on account of slight expansion to the die. The contraction of the epoxy resin die material may be of clinical significance. Casting fabricated by indirect technique are accurately adapting on Type IV Gypsum dies, an epoxy die is 0.16% smaller leading to clinically unacceptable casting that would not seat on the prepared tooth. Although the percentage of contraction exhibited by Epoxy resin is less than percentage of expansion exhibited by gypsum-based die materials, transverse strength of epoxy resin is far superior to Type IV Gypsum and resin-modified gypsum. Resin admix gives additional strength to gypsum-based die materials. Epoxy resin with shrinkage of 0.1% that occurs during hardening, is more resistant to abrasion and stronger than a high-strength die stone. High-strength stone dies may be from 0.35% larger to 0.25% smaller than the prepared tooth, on contrary epoxy dies all exhibit some polymerization shrinkage, with values ranging from 0.1% to 0.3% [26], leading to undersized dies. Synarock is resin modified gypsum with higher gypsum content compared to conventional Type IV Gypsum and has lower water powder ratio. It’s a thixotropic superstone with ultimate synthetic blend gives optimum fit, stability, edge strength. With setting expansion after 24 hours is 0.08. Although both conventional gypsum and resin modified gypsum undergo expansion, this expansion in synthetic gypsum is less. With the advent of digitization in dental field, efforts are made to reduce laboratory steps and deliver single visit restoration. Comparative study determing the accuracy of marginal fit and marginal micro leakage of copings fabricated using laser metal sintering technique and conventional casting technique concluded that marginal misfit values were similar for both groups and so the result was not statistically significant. Copings fabricated via the lost wax technique showed higher marginal microleakage values than those in the laser sintered technique [27]. On contrary in-vivo evaluation of fit of zirconium-oxide based ceramic single crowns generated with two CAD/CAM systems, when compared to conventional metal ceramic single crowns demonstrated that the two groups of zirconium-oxide crowns exhibited similar and acceptable marginal fit when compared to traditional metal ceramic crowns [28]. A systematic review on studies compiling articles published before April, 2012 evaluated a total of 17 ceramic systems, 48 in-vitro and 6 in-vivo studies with three different fabrication method that is CAD/CAM, hot pressing and slip casting concluded that marginal gaps measured, 94.9% were in the range of clinical acceptability also selection of system is not based on marginal accuracy as ceramic crowns from these systems is generally clinically acceptable, but rather on a system’s ability to produce the type of ceramics best adapted to existing clinical conditions and esthetic expectations [29]. A systematic review comparing marginal and internal fit of fixed dental prosthesis fabricated with digital techniques to those fabricated using conventional impression concluded that the digital impression technique provided better marginal and internal fit of fixed restorations than conventional techniques [30]. Additionally, a study assessing the marginal fit reported that vertical gap in crowns made digitally after digital impressions was 48±25 mm which was significantly less than the crowns made using the convectional technique (74±47 mm) [31].
Limitation
This study exhibits limitations of smaller sample size, horizontal discrepancies are not estimated that require sectioning of copings along with the standard models, future studies can be undertaken to evaluate the horizontal discrepancies with a larger sample size.
Conclusion
Within the limitations of this in-vitro investigation, it can be concluded that both preparation designs (shoulder and deep chamfer) did not exhibit significant statistical difference in terms of marginal accuracy and either of them can be used to fabricate metal ceramic restorations. Mean vertical marginal gaps were beyond the clinically acceptable range for copings fabricated on epoxy resin as a die material, exhibiting highly significant statistical difference when compared with other two groups of die material. Copings fabricated on Resin modified gypsum exhibited least vertical marginal gaps (within a clinically acceptable range), presented accurate adaptation over the CAD/CAM models.
* p<0.05
* p<0.05