Childhood obesity and overweight is a global epidemics and has been increasing in the developing countries [1]. In Indian subcontinents, undernutrition has been a public health problem for decades [2]. Recent studies have reported an increased prevalence of overweight and obesity in India [3–8]. Childhood obesity is associated with morbidities such as type 2 diabetes mellitus, atherosclerosis, hyperlipidemia, hypertension and metabolic syndrome [1,9].
Obesity in children is an antecedent of adult obesity. Atleast 30% of obesity begins in childhood [10] and 50-80% of obese children become obese adults [11]. Childhood obesity is linked with increased mortality and morbidity independent of adult obesity [12]. Increased prevalence of obesity among children may be due to various factors like sedentary activity, spending time on internet, video games and television and easy accessibility to fast food with growing prosperity [13]. Studies have concluded the need for well designed interventions to reduce the risk of obesity and the burden of mortality and morbidity associated with non- communicable diseases [14]. During adult life weight reduction interventions yield poor outcome, which highlights the importance of prevention of obesity in early life. In India, only few studies have focused on intervention to prevent and control obesity [15,16]. A Cochrane review concluded that interventions combining physical activity, dietary and other behaviour factors appear to be more effective in obesity management [17]. The studies conducted in India has focused on either nutrition education or combination of nutrition education and physical activity or on health promotion program [15,16]. Parents and teachers play a significant role in shaping the future of children. Involving the parents and teachers in the lifestyle modification intervention for prevention and control of childhood obesity has not been explored in India. School based interventions can reach large population of school children in a cost effective manner.
Thus, present study aimed at developing and evaluating the effectiveness of multicomponent intervention and also involving physical instructors and the parents as the means of intervention, there by reducing the body fat, improving the lifestyle practices and there by improving the self esteem of obese children.
Materials and Methods
School based randomized controlled trial was conducted over a period of six months between August 2009 and February 2010 at selected secondary and higher seconadary schools of Udupi district, Karnataka, South India. The participants of the study were obese children between the ages of ten and sixteen years with BMI above 85th percentile for age and sex. Initially a list of secondary and higher secondary English medium schools was obtained from school registration office of the District. Depending on the location, the schools were clustered into five zones. Three zones were selected randomly. Eleven English medium schools were randomly selected from these zones proportionately according to number of schools present in each of these zones. Height and weight of 2,938 children was measured using standard procedure and BMI was calculated based on WHO standards [18]. Based on BMI for age and sex, children were classified as underweight (679), normal (1904), overweight (214) and obese (141). All overweight and obese children (355) were considered eligible for intervention.
Out of 11 schools, six schools were randomly assigned for intervention group and five schools for control group. Out of six schools from the intervention, majority of the parents of one school did not consent for the intevention and thus the children from this school were dropped from the study. Finally out of 355 eligible sample only 251 children were included in the study. Cluster of obese children (BMI >85th percentile for age and sex) from the schools assigned to intervention were considered as sample for intervention group. Similarly cluster of obese children from the schools assigned to control group were considered as sample for control group. Thus sample of 120 obese children enrolled for intervention. There was an attrition of 30 (25%) sample in the experimental group. Thus the final sample in the intervention group was 90. Total sample of 131 obese children were enrolled as controls. There was an attrition of 27 (20.61%) sample in the control group. The final sample in the control group was 104.
Since the cluster of children were assigned to intervention and control group, researcher could not ensure the equal number of samples in intervention and control group [Table/Fig-1].
Flow diagram of the study.
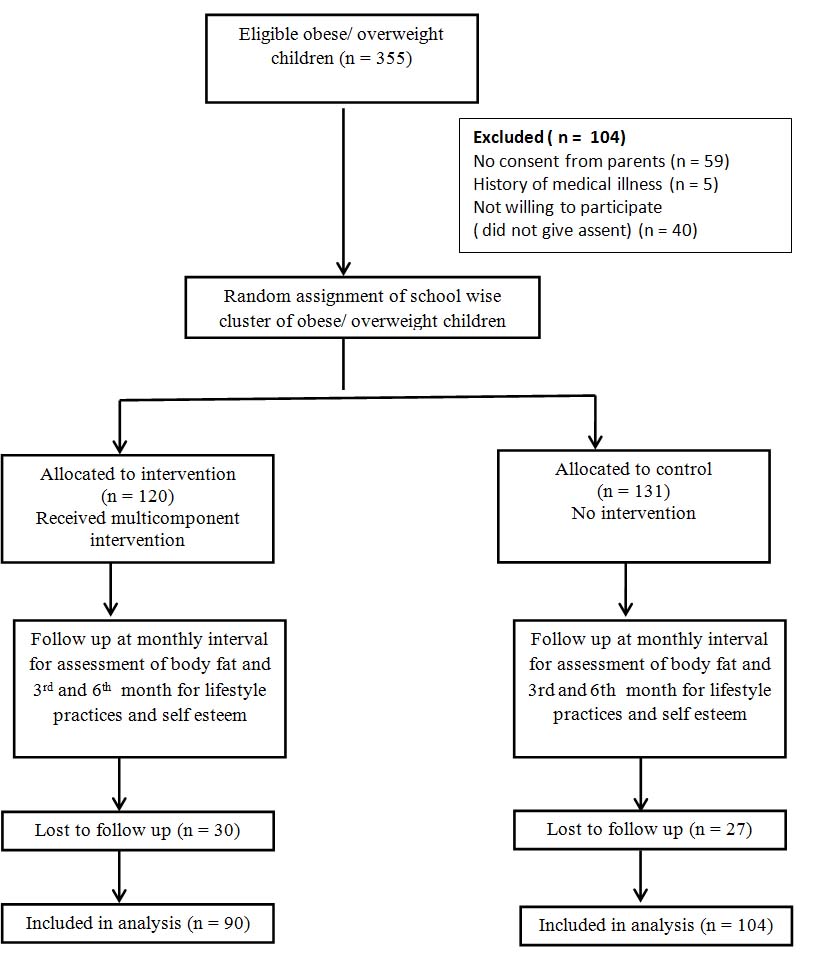
The reasons for attrition in the intervention group was, started practicing for team sports for state level competition (n=2), no time to practice aerobics in school (n=1), had fall at home & suffered fracture (n=3), change of means of transportation to school and not able to reach school during aerobics sessions (n=7), enrolled for tuition class and not able to attend aerobics at school (n=17). However, in the control group the chidren who were absent during assessment (n=27) were excluded from the analysis as investigator did not have any control over this group.
Anthropometric measures
Height of the child was recorded to the nearest 0.5 cm using the calibrated wall mounted measuring tape. Weight was recorded using the calibrated beam balanced type of weighing scale to the nearest 0.1kg. BMI was computed using the formula, BMI=weight (Kg)/ height (m)2. Triceps, biceps and sub scapular skin fold thickness was measured using calibrated skin fold caliper manufactured by Sayanis Surgicals, Hyderabad. Standard procedures were followed for measuring height, weight, and skin fold thickness.
Assessment of lifestyle practices
A five point Lifestyle practice scale for adolescents developed by the investigator was used to measure the lifestyle practices of the children. There were 38 items in the questionnaire stated both positively and negatively, where each item ranged from “never” (0) to “almost always” (4). For positively stated items almost always response carried a score of 4 and ‘never’ response carried zero score. For negatively stated items ‘never’ response carried a score of 4 and ‘almost always’ carried zero score. Instrument’s items were summated to derive a total lifestyle practice score (range 0 – 152). Higher the score indicate good lifestyle practices. The content validity and reliability of the scale was established. To establish content validity, the tools were submitted to seven experts. The selection of experts was done based on their experience and clinical expertise. Validation was obtained in terms of appropriateness and relevance of items in the tool. There was 100% agreement on 37 items. One item had 86% of agreement. Suggestion was to specify the fatty food items. The item was modified by giving examples for fatty food. There was a suggestion to include the habits like smoking, chewing tobacco and alcohol. Though it was not included as it was not relevant for this group of sample. To assess reliability, the English version of the tool was administered to 20 children. Reliability (stability) was established by test retest method and reliability coefficient was calculated by pearson product moment correlation. Reliability coefficient was 0.94 and considered to be reliable.
Assessment of self esteem
Self-esteem of obese children was assessed using standardized children’s self concept scale [19]. The scale contained 80 items in all with ‘Yes’ or ‘no’ responses. There are six subscales which are considered to be important in the psychological world of childhood and adolescence, which are behaviour, intellectual and social status, physical appearance and attributes, anxiety, popularity and happiness and satisfaction. The scale items are scored in a positive or negative direction to reflect the evaluation dimension. A high score on the scale is presumed to indicate a favourable self concept.
The items were scored in the direction of high self concept according to the scoring stencil. One score was awarded to each statement either for ‘Yes’ or ‘No’ as per the directions in the manual. The sum of scores for each subscale of self concept scale was obtained by adding the scores. The total self concept scores of all the six areas was considered as self concept score. The maximum score for the total self concept can be 80 and minimum score can be zero. Higher the score on the scale indicates favourable self esteem. Since this was a standardized scale and applicable to Indian set up, content validity and reliability was not established.
Ethical consideration
Administrative permission was obtained from school authorities and ethical clearance was obtained from institutional ethical committee. For children in the intervention group informed consent was obtained from their parents. The informed consent form was sent to the parents through school authorities and assent was obtained from the children. For the control group no consent was taken, from the parents as intervention was not given to them. From children assent was taken only for assessment of anthropometric measurements and for administering questionnaire. However, they were unaware of the experiment administered to intervention group.
Multicomponent Intervention
Pre-intervention assessment was done on both the groups. The multicomponent intervention was administered to intervention group which included education provided to the obese children on lifestyle modification, education of the parents and increasing the physical education activity of these children in the form of aerobics under the supervision of physical education teacher.
After the pretest, circular was sent by the school principal to parents of intervention group, to attend an awareness programme at school premises and awareness was given to the parents. After the discussion, parents were given an informational booklet. The informational booklet was prepared by the investigator. The areas covered in the informational booklet were meaning and causes, assessment, consequence and weight reduction strategies and lifestyle modification. The sub-areas included weight reduction strategies and lifestyle modification, importance of physical activity, healthy dietary practices, advise to reduce television viewing, to participate in recreational and other physical activities. The content validity of the booklet was established by submitting the booklet to five experts along with criteria checklist. The areas covered in the checklist was: 1) content – adequacy, appropriateness and relevancy; 2) Language – clear and simple; 3) Logical organization. The experts were asked to put (√) mark in terms of agreement or disagreement. To ensure content validity, percentage of agreement was obtained and there was 100% agreementin all areas. The booklet was translated to local language by the language experts and language validity was established by translating back into English. Only one session of 1.5 -2 hours duration was conducted for parents.
Education of the children was done in the sequence of quiz; snake and ladder games and group discussion. Eligible children from each class were called at a time during their free hours or after school hours with parents’ permission. A Quiz was administered first, which was the point for discussion and small group discussion was conducted, with number of children ranging from 8-10. The quiz questions focused mainly on modification of lifestyle practices and increasing the physical activity. On the next day children were motivated with the help of snake and ladder games developed by the investigator – a journey to healthy lifestyle. This led to the second session of group discussion, during which all the doubts of children were cleared. All the children were given the content validated informational booklet prepared for them.
A video on aerobics was developed by the researcher in consulataion with expert of aerobics. The video was recorded in the DVD format in CD - ROM. This was displayed in the television available in the school with the help of DVD player and children were trained to perform aerobic exercise. Exercise was performed by all the children either in the morning or after school hours according to the convenience of the parents and children on all working days of the schools except on special occasions and examination time. Aerobics sessions were performed in their respective school under the supervision of physical education teacher of that school. The aerobics sessions were held in recreation room of the selected schools. Daily attendance was maintained by the teacher and if a student was absent for more than four days a week, he/she was contacted to identify the reason and was considered as a drop out. Anthropometric measurement was carried out at the end of every month in both the group. For the control group after the post test (after 6 months) teaching and informational booklet was given.
Statistical Analysis
The collected data was analysed using SPSS statistical package version 16. To describe the demographic characteristics, frequency and percentage was calculated. To compare the baseline parameters between the group t-test was applied. Mixed method repeated measures ANOVA was applied to find the effectiveness of intervention.
Results
The demographic characteristics of children showed that in intervention group, 51.7% and in control group 56.5% of chidren were belonged to the age group of 14-16 years. In intervention group 53.3% were boys whereas in control group 50.4% were girls.
Comparison of data at baseline
Independent t-test was used to compare the baseline parameters between the groups. The mean BMI, biceps, triceps and subscapular skin fold thickness were similar at baseline in both the groups (p>0.05) [Table/Fig-2], indicating comparable anthropometric parameter, lifestyle and self esteem scores at the commencement of intervention.
Antropometric parameters and assessment scores of intervention and control group at baseline and at 6 months.
| Parameters | Intervention group (n= 90) | Control group (n=104) | p- value |
|---|
| BaselineMean±SD | Post-interventionMean±SD | BaselineMean±SD | End of 6 monthMean±SD |
|---|
| BMI | 24.9±3.5 | 22.8±3.5 | 24.2±3.3 | 25.1±3.5 | .034 |
| Triceps SFT | 21.4±4.4 | 16.0±3.7 | 21.4±3.9 | 22.9±4.2 | .001 |
| Biceps SFT | 17.3±4.7 | 12.5±3.4 | 17.4±4.0 | 19.6±3.8 | <.001 |
| Subscapular SFT | 21.0±4.5 | 15.4±4.1 | 21.2±4.7 | 22.8±4.5 | <.001 |
| Lifestyle Practices | 97.7±14.1 | 109.1±12.6 | 98.9±13.4 | 100.5±14.4 | .009 |
| Self Esteem | 56.4±9.9 | 64.4±6.6 | 56.2±10.5 | 48.2±11.1 | < .001 |
Effect of intervention on body fat measures
To find the effectiveness of multicomponent intervention mixed method repeated measures ANOVA was computed. Findings shows that in the intervention group, the mean BMI has reduced from 24.9 to 22.8 and in the control group mean BMI has increased from 24.2 to 25.1 [Table/Fig-2]. It is very clear that the BMI of intervention group has reduced significantly. However, the increase in the BMI of control group was within the normal range of their development. When compared to control group, intervention group had significant decrease in the BMI (p = 0.034). Therefore, it is concluded that multicomponent intervention was effective in reducing the BMI of obese children.
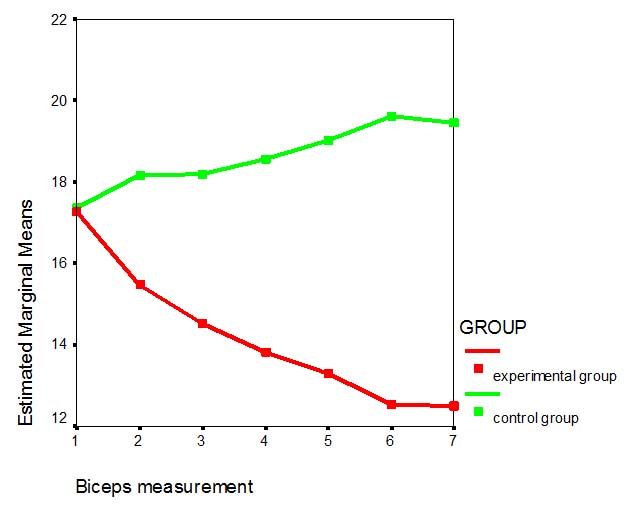
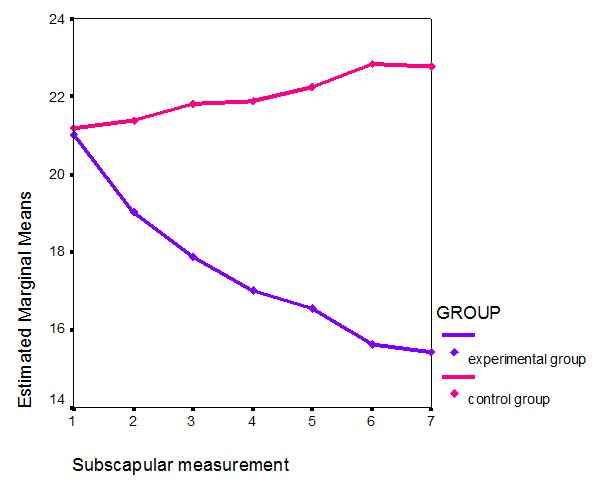
At baseline the mean triceps skin fold thickness of intervention group was almost equal to the control group. At the end of six months, the mean triceps skin fold thickness of control group was higher than the intervention group which is statistically significant (p = .001). Significant reduction in mean biceps and subscapular skin fold thickness was observed in the intervention group. A statistically significant difference in the mean biceps (p< 0. 001) and subscapular skinfold thickness (p < 0. 001) was observed between intervention and control group, which is depicted in [Table/Fig-3,4].
Mean difference in the biceps SFT of intervention and control group.
Mean difference in the SFT of intervention and control group.
Effects of intervention on lifestyle practices and self esteem
Repeated measures ANOVA showed a significant difference between the lifestyle practice scores (p= 0.009) and self esteem scores (p = <0.001) of intervention and control group. To find the significant difference in the mean lifestyle practice score, pairwise comparison was made using Bonferroni Comparison showed that aerobic exercise for three months along with education of parents and children significantly improved the lifestyle practice scores of obese children (p < 0.05).
Discussion
To date, the evidence base for interventions for childhood obesity is limited and a very few studies have been published in India. Reduced incidence of obesity due to school based intervention has been reported earlier in the western countries [20–22]. A school based literature in India also reported a significant effect of school based intervention in reducing the prevalence of childhood obesity [15,16,23]. In the present study statistically significant difference was seen in the BMI, triceps, biceps and subscapular skin fold thickness of intervention and control group.
Study findings are in consistent with the findings of a cluster randomized trial to assess the effectiveness of a multicomponent school based physical activity programme during one school year on physical and psychological health in young school children which was carried out in two provinces of Switzerland. The study reported that compared with controls, children in the intervention group showed smaller increases in the sum of four skinfolds by 0.12 score units, corresponding to about 2mm [21].
A school based Dutch Obesity Intervention in Teenagers program also resulted in beneficial effects on the sum of skinfold thickness measurements in girls [20]. A school-based, multicomponent intervention for reducing percentage body fat in American-Indian school children showed no significant reduction in percentage body fat. However, a significant reduction in the percentage of energy from fat was observed in the intervention schools [22].
In India very few studies have been reported in the literature. Multi-vitamin-zinc supplementation with lifestyle intervention was conducted in Pune, India showed a positive effect of on the cardiometabolic status, significant reduction in inactivity, energy and fat intakes and increase in micronutrient density of diets and physical activity in overweight children [23]. A study on effectiveness of a multi-component intervention model of nutrition and lifestyle education on behaviour modification, anthropometry and metabolic risk profile of urban Asian-Indian adolescents in North India reported beneficial changes in anthropometric and biochemical profiles of the Asian Indian adolescents [24]. However these studies targeted at the lifestyle style modification or increasing the physical activity in the school curriculum. None of these studies involved parents as means of intervention.
The achievement of statistically significant reduction in the Body Mass Index, skin fold thickness of obese children in the present study was extremely encouraging. The study received strong support from children, parents, principals and physical education teachers who had to be actively involved in delivering and supporting the programme. The study also showed that if physical education teachers are properly trained and motivated they can promote significant change in the physical activity of the children. Schools are the ideal ways of comunication as they are central to children’s lives and information can be quickly passed through this channel. With available resources health promotional activities can be easily implemented at the school level.
Limitation
The intervention was limited to six months and long term effects were not measured. The aerobics was performed by the children only on working days of the school and researcher could not have any control during holidays. The relationship between the intervention and BMI adjusted for covariates could not be measured statistically because of small sample size. Effect of lifestyle practices measured was limited to the response of the children to the questionnaire.
Conclusion
Long-term aerobic exercise along with education of parents and children can significantly improve the lifestyle practices of children there by reducing the body fat of obese children. Obese children need to control diet and perform vigorous exercise at least for 20 minutes a day to reduce the excess fat and maintain their body fat level.