Fuchs Heterochromic Iridocylitis (FHI) is a distinct form of anterior uveitis that is responsible for approximately 2% to 11% of all anterior uveitis [1,2]. FHI consists of chronic low grade anterior uveitis and is associated with complications such as cataract, glaucoma and vitreous opacities. However, typical features of anterior uveitis like pain, redness, posterior synechia and photophobia are characteristically absent [2].
The classic description of FHI includes diffuse stellate keratic precipitates with iris heterochromia [2,3]. However, various clinical signs are not always present at the same time making FHI difficult to diagnose [2,3]. Incorrect diagnoses may lead to unnecessary corticosteroid therapy.
Ernest Fuchs’s was the first to describe the disease in 1906, he assumed that, the syndrome was caused by a noxious factor of unknown origin [4]. More than 100 years have passed since then, but the aetiology of FHI is still obscure. Many theories have been put forward like the sympathetic theory [5] introduced the idea that some tropic defect in the sympathetic system inhibited the normal process of uveal pigmentation. According to hereditary theory [5], it was thought that, all types of heterochromia including FHI are hereditary in nature. Ocular toxoplasmosis [6] and rubella virus [7] infection have been implicated. Increased level of gamma globulins in the aqueous humour suggests the possibility of an intra ocular immune reaction [8].
Thus, FHI is probably a secondary phenomenon to a variety of insults, till date there is no laboratory test to diagnose FHI. The diagnosis of FHI is made on clinical grounds taking in to consideration the spectrum of signs and symptoms of the disease.
The present study was conducted to study the clinical characteristic and outcome of cataract surgery in patients with FHI. To our knowledge, no study on FHI has been conducted among Kashmiri population and no such data involving Kashmiri population has been reported in literature.
Materials and Methods
The present prospective study was carried out in the Postgraduate Department of Ophthalmology, Sher-i-Kashmir Institute of Medical Sciences (SKIMS), Bemina from March 2012 to January 2015. The study included 33 eyes of 32 patients; with an alpha error of 5% and power of 80%. We estimated that, 29 patients would be required in our study. In order to detect potential variations and avoid potential errors, 32 eyes were included in our study with diagnosis of FHI who underwent cataract surgery with IOL implantation and were followed-up for upto twelve months postoperatively. The study was undertaken after obtaining approval from the Ethical Committee. Informed consent was taken from all patients before enrolling them in our study. The study was carried out in accordance with the code of ethics of the world medical association (Declaration of Helsinki) for experiments involving humans.
After obtaining a comprehensive history from the patients, a thorough clinical examination was done which included slit lamp biomicroscopy, fundus examination in patients with immature cataract, B scan was done in patients with mature cataract to rule out any posterior segment anomaly, visual field analysis and gonioscopy was done as and when required, Intra Ocular Pressure (IOP) was measured by using goldman applanation tonometer. FHI was diagnosed using Kimura diagnostic criteria which included diffuse iris stromal atrophy with or without heterochromia [9], small white keratic precipitates scattered diffusely over the corneal endothelium, minimal aqueous flare and cells, cells and opacities in the anterior vitreous and absence of iris synechia. All other forms of uveitis and retinal vasculitis were excluded.
Pre-operative data included age, sex, Best Corrected Visual Acuitiy (BCVA), inflammatory findings in the anterior chamber, type of cataract, presence of vitreous opacities, fundoscopic findings and IOP. In our study, we used LOCS III (Lens Opacities Classification System) to help differentiate various types of cataracts. Intra-operatively, the type of surgical technique used was noted as well as occurrence of any intra-operative complications. Presence or absence of Amslers sign (paracentesis of the anterior chamber in FHI may produce a filiform anterior chamber hemorrhage from the angle 180 degrees from the site of puncture) was recorded
All patients were operated by the same surgeon. Phacoemulsification and small incision cataract surgeries were performed on patients based on their age and condition of the lens. The IOL type used was either Poly Methyl Metha Acrylate (PMMA), or acrylic lenses.
Pre-operatively, all patients were put on topical antibiotics 24 hours before surgery. None of the patients received systemic steroids pre or post-operatively. Post-operatively, patients were put on topical antibiotic steroid combination eye drops 6 times/day which was then tapered over a period of 6 to 8 weeks. Post-operative follow -up was done on 1st day, one week, one month, and two month, six month and at twelve months. Post-operative data included BCVA, IOP, inflammatory condition, presence of vitreous opacity, posterior capsular opacification and fundus examination findings.
Statistical Analysis
Data obtained was saved in Microsoft Excel and analysed using statistical package for social sciences (SPSS Ver. 20). Statistical test used was Mcnemars test. A p-value of < 0.05 was considered as statistically significant.
Results
Mean age of our study group was 33.9 years (Range 18 to 65 years). Thirty three eyes of 32 patients were examined. The number of male patients was 15 (46.8%) and the number of female patients was 17 (53.2%). There was bilateral involvement of eyes in only one patient.
Most common presenting complaint of patients was decrease in vision (78%) followed by floaters in 20% and heterochromia in 2% of cases. Cataract was present in all the cases and was the principle cause of decreased vision. About 32% of patients had a history of steroid use (topical/oral) before presenting to us. Lens opacities were posterior sub capsular in nature in 24 (72.73%) eyes and mature cataract was found in nine (27.27%) eyes. Phacoemulsification was done in 20 (60.6%) eyes, rest 13 (39.3%) eyes underwent Small Incision Cataract Surgery (SICS). Cataract surgery was combined with trabeculectomy in two eyes as they had co-existing glaucoma which could not be controlled by medical therapy alone. The IOLs were inserted in the bag in 28 (84.84%) eye and in the sulcus in five (15.15%) eyes. We used Poly Methyl Metha Acrylate (PMMA) and acrylic lenses in our study.
BCVA showed significant improvement following cataract surgery (p< 0.001) at all stages of follow-up i.e., one week, one month, two months, six months and twelve months. There was an improvement of four lines in 78.78% of cases, twelve months following cataract surgery (BCVA > 6/12). There was no significant difference between post-operative vision of patients based on surgical technique employed for cataract surgery (p= 0.28) or the type of IOL used (p=0. 34).
Intra-operatively, we encountered transient hyphema (amslers sign) during paracentesis in six cases (18.18%). Hyphema was transient and did not affect the surgical procedure. Posterior capsular rent occurred in two cases (6.6%) whereas, one case was associated with posterior capsular plaque. Post-operative the cause of decreased vision was vitreous opacities in nine eyes (27.27%), glaucoma in eight eyes (24.24%) and posterior capsular opacification developed in six eyes (18.18%) during the follow-up period of twelve months. Posterior capsular opacification developed six months after surgery. Fundus examination revealed chorioretinal scar in one case However, it was not associated with decreased vision as it did not involve the fovea.
Four patients were diagnosed to have open angle glaucoma pre-operatively. Out of which, two patients had IOP >30mmHg requiring trabeculectomy with mitomycin C. During our follow-up period of twelve months, four more patients developed open angle glaucoma after one month of surgery which was controlled on anti-glaucoma medication alone. The mean IOP in these four cases after one month of surgery was 28mmHg. Mean IOP reduced to 16mmHg following antiglaucoma medication at six month of follow-up. Visual field analysis using humphrey perimeter revealed mild to moderate visual field loss in all cases having glaucoma.
Discussion
The mean age in our study was 33.9 years (Range 18 to 65 years). There was no gender preponderance found in our study. Most of the cases presented in the 3rd or 4th decade of life. There was bilateral involvement in only one case. This is comparable to existing literature on FHI [10,11].
The most common presenting complaint of patients was a decrease in vision (78%) followed by floaters in 20% and heterochromia in 2% of cases. Redness, pain, photophobia, ciliary injection and posterior synechia which are typical features of anterior uveitis were not seen in any of our cases. Patients were unaware of the condition until there was decrease in their vision due to cataract formation this can be attributed to the asymptomatic and insidious nature of FHI. All these findings are in agreement with earlier data on FHI [10,12].
In our study, cataract was present in all cases at the time of diagnosis. Incidence rates have been reported to vary from 15% to 80.2% [13]. The high incidence in our study could be attributed to patients presenting late in the course of the disease [12]. The most common type of cataract in our study was posterior sub capsular in 24 eyes (72.73%) which is similar to other chronic uveitis cases or to corticosteroid treatment [14]. Cataract formation could be attributed to long standing anterior and posterior chamber inflammation and unnecessary corticosteroid treatment. About 32% of our patients had history of steroid use before presenting to us.
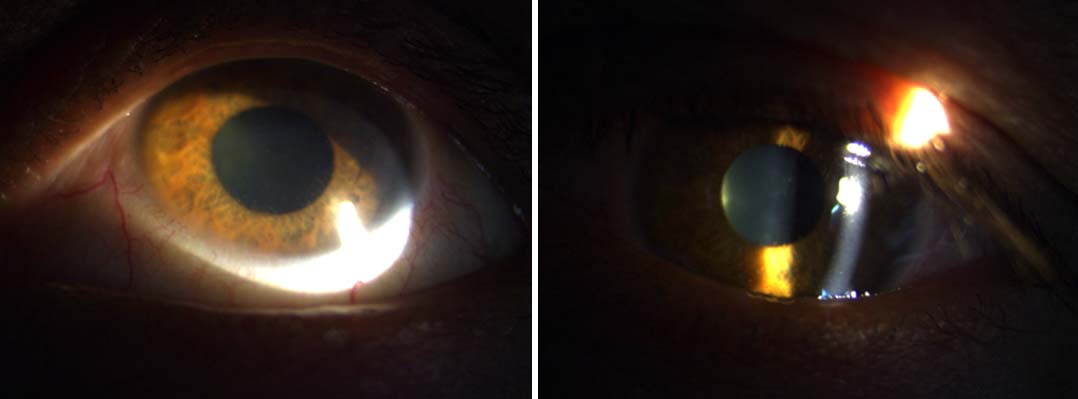
Stellate keratic precipitates were present on the corneal endothelium in all of our cases [Table/Fig-1,2]. They were translucent and scattered all over the endothelium. These precipitates did not affect vision which explain the patient’s unawareness of the condition [15]. The presence of these stellate keratic precipitates should be looked for in every patient suspected of FHI, as they are one of the most reliable sings of FHI [16].
Pre-operative images showing iris hypochromia and stellate KPs on corneal endothelium.
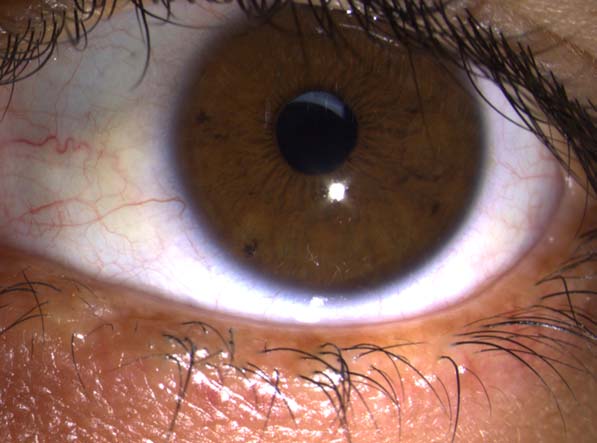
Six month post-operative image showing pseudophakia with capsular opacification.
In our study, heterochromia [Table/Fig-1] was present in only six eyes (18.75%). Majority of the patients had dark brown iris. In regions with predominantly brown eyes such as China and Mexico, heterochromia was only reported in 14% and 25.3% respectively [17,18]. Thus, heterochromia is not present in all cases and this should be kept in mind while diagnosing a case of FHI. However, on careful slit lamp examination, we were able to appreciate subtle iris changes in all of our cases which included loss of iris details, radial markings becoming less prominent and iris surface become smoother due to loss of crypts. All these findings should be kept in mind to avoid misdiagnosing a case of FHI, which may lead to potentially harmful treatment in the form of corticosteroids [19].
In our study there was an acceptable visual outcome in patients undergoing cataract surgery. BCVA showed significant improvement following cataract surgery (p< 0.001). Postoperatively 26 eyes (78.78%) showed an improvement of four lines or more (BCVA of > 6/12). These findings are in agreement with other studies [20,21]. Milazzo et al., showed visual acuity > 6/12 in 76% of their cases which is again comparable to our study [22]. In a similar study by Soheilian M et al., 78 % of the patients obtained BCVA < 6/12 which is same as that found in our study [23]. Similiar studies done by other authors like Javadi et al., Tejwani et al., Ram et al., kosker et al., and Bhargava et al., have shown BCVA better than or equal to 6/12 in 100%, 88.3%, 100%, 94.5% and 92.5% respectively [20,21,24-26]. A comparison of these studies is shown in [Table/Fig-3]. Thus, we can say that, cataract extraction with IOL implantation in patients with FHI is a safe procedure.
Showing outcome of cataract surgery in Fuchs Heterochromic Iridocylitis (FHI) as reported by different studies [20,22-26].
| Author (Year) | Reference No. | No. of Cases | Follow-Up(Months) | BCVA ≥ 6/12 (%) |
|---|
| Javadi et al., 2005 | [20] | 41 | 17.8 | 100 |
| Milazo et al., 1996 | [22] | 94 | 41 | 76 |
| Soheilian M et al., 1997 | [23] | 32 | 14.4 | 78 |
| Ram et al., 2002 | [24] | 20 | 24.2 | 100 |
| Kosker et al., 2013 | [25] | 55 | 6 | 94.5 |
| Bhargava et al., 2014 | [26] | 54 | 11.53 | 92.5 |
| Present Study 2015 | | 33 | 12 | 78.78 |
Amsler’s sign was encountered in six eyes (18.18%) during paracentesis. Thus, the absence of this feature does not exclude FHI, but the occurrence dose makes the diagnosis more likely [27]. Moreover, studies have shown that, amsler’s sign is not exclusive to FHI as it occurs in other ocular conditions like ocular sarcoidosis [28].
Most common cause of decreased vision postoperatively was vitreous opacity in nine eyes (27.27%). Other studies [20,29] have also reposted vitreous opacity as the most common cause of decreased vision [11,12] postoperatively. Vitreous involvement in Fuchs has been underrated even though it can cause visual problems. Vitreous inflammation associated with cells and strands can be more marked than anterior chamber activity [30]. Moreover, in our study all patients had developed cataract making proper examination of vitreous difficult. The possibility of post-operative floaters was explained to the patients especially those with dense cataract, and the need for additional surgical procedures like vitrectomy was explained. Post-operative floaters can be very annoying to the patients so proper counseling should be done before operating the patients.
In our study, glaucoma was one of the main causes of visual loss in patients with FHI. A total of eight patients (24.24%) developed open angle glaucoma in our study. Out of the eight patients, four were diagnosed post-operatively during the follow-up period. Given the irreversible nature of visual loss in glaucoma all patients of FHI should be evaluated for glaucoma both pre and postoperatively. Other studies have reported incidence to vary between 3% to 35% [21]. This difference can be attributed to different diagnostic criteria and length of follow-up of the study. Several possible causes have been reported including neovascularisation of the anterior chamber, angle, trabeculitis, trabecular sclerosis, collapse of canal of schlemm and corticosteroid treatment but usually no apparent cause can be found [27,31,32]. In conclusion, glaucoma should be considered as one of the main causes of visual loss in FHI.
In our study posterior capsular opacification [Table/Fig-4] developed in 6 eyes (18.18%) after six months of follow-up, requiring ND:YAG laser capsulotomy. Capsular opacification has been reported to be 14.6%, 22% and 30% in other studies [20,22]. This could be attributed to intra ocular inflammation or younger age group of the patients [33].
Six month postoperative image showing stellate KPs.

Limitation
One of the main limitations of our study was a lack of aqueous fluid analysis which would have given us more insight in to aetiology of FHI. This could not be done due to financial constraints and lack of proper resources. Moreover, fundus flourescein angiography was not done in our patients which could have revealed more about posterior segment associations of FHI.
Conclusion
Cataract extraction with IOL implantation in FHI is associated with good visual prognosis and few complications. However, glaucoma is one of the main concerns and should be closely monitored both pre and postoperatively.
Till date, there is no single laboratory investigation which can lead to diagnosis of FHI. This is the reason why in our study we laid emphasis on thorough clinical examinations as the cornerstone for diagnosis of FHI. The principle of “primum non nocere” should always be kept in mind while treating FHI, as treatment may be more harmful than the disease itself. Treatment should be reserved for the complications of FHI and not for the inflammation associated with the disease.