The optimal timing for discharging preterm infants home is a difficult issue for clinicians, especially those in resource poor set-ups. Duration of hospital stay and post-menstrual age at discharge is inversely proportional to birth weight and gestation [1,2]. Morbidities such as sepsis, chronic lung disease, necrotizing enterocolitis, retinopathy of pre-maturity are associated with longer hospital stay [2]. The importance of ensuring a smooth transition from the protected environment of the Neonatal Intensive Care Unit (NICU) to home for safe care after discharge cannot be overemphasized considering the higher rates of re-admissions with decreasing gestational age at birth [3]. The variation in home discharge policies for preterm infants relates to many factors including their need for access to health care after discharge, geographic location and importantly, the parent’s socio-economic status. In the past preterm infants were commonly discharged only after achieving a weight of 2000 grams. However, recent studies have shown that early safe discharge is possible when preterm infants are discharged on the basis of physiological criteria (e.g., ability to feed to support growth, maintaining temperature, mature respiratory control) rather than discharge weight [4-9]. Interventions such as oromotor stimulation, Kangaroo Mother Care (KMC), massage, gavage feeding and non-nutritional sucking may help in earlier discharge [10-13]. Ours is a busy NICU in a resource poor set up in India with 1044 admissions with a median gestational age of 34 weeks (IQR 31; 38 weeks) and median birth weight of 1780 grams (IQR 1310; 2494 grams) per year.
Major advances in management of sick preterm infants have lead to increased rates of survival but issues related to discharge timing have not been studied well. Early home discharge of preterm infants is a priority for us for two equally important reasons-shortage of beds and poor socio-economic status of the parents who mostly come from remote places. Given the socio-economic and medico-legal importance of the issue, we aimed to study the outcomes of our ex-preterm infants discharged home ‘early’, to guide our clinical practice.
Materials and Methods
This was an analysis of retrospectively collected data on all ex preterm infants (gestation <34 weeks at birth) discharged home from our NICU between 1st February 2014 to 31st January 2015. The 235 enrolled infants were stratified into two groups based on gestation at birth: Group I (n=54): 26-29 weeks, Group II (n=181): 30-34 weeks. Approval from the Hospital’s Ethics Committee was obtained before starting the study.
Discharge policy: All infants with gestation <34 weeks at birth were discharged home during the study period when they fulfilled the following criteria: (1) Stable haemodynamic and respiratory status; (2) Maintaining axillary temperature; (3) On all breast-feeds or spoon feeds; (4) Weight gain of 20-30g/day for three days; (5) Mother confident to look after her baby at home.
Support systems: Oral feeds were started when the infant was cardio-respiratory stable. Readiness to feed was determined by infant’s feeding cues i.e., mouthing, rooting and bringing hand to mouth. Apart from supporting breast feeding we encouraged KMC and spoon feeding for all infants in the NICU as soon as feasible.
Estimation of gestation (at birth) was based on the first ante-natal ultrasound and the modified Ballard’s Score [14]. Weights were measured to the nearest gram using an electronic digital scale. For each group, data on neonatal demographic characteristics and morbidities till discharge home were recorded for all eligible infants. The data were expressed as number (%), or mean±Standard Deviation (SD), and median (Interquartile range: IQR). Statistical analysis was performed using SPSS software (Version 11.0; SPSS Inc., Chicago, IL).
The outcome measure was re-admission and/or mortality within 4 weeks after discharge of all the eligible infants. The reasons for re-admission or mortality were also recorded. The outcome data was obtained by a telephonic enquiry with all parents regarding the well-being of the infants after the first month of discharge.
Results
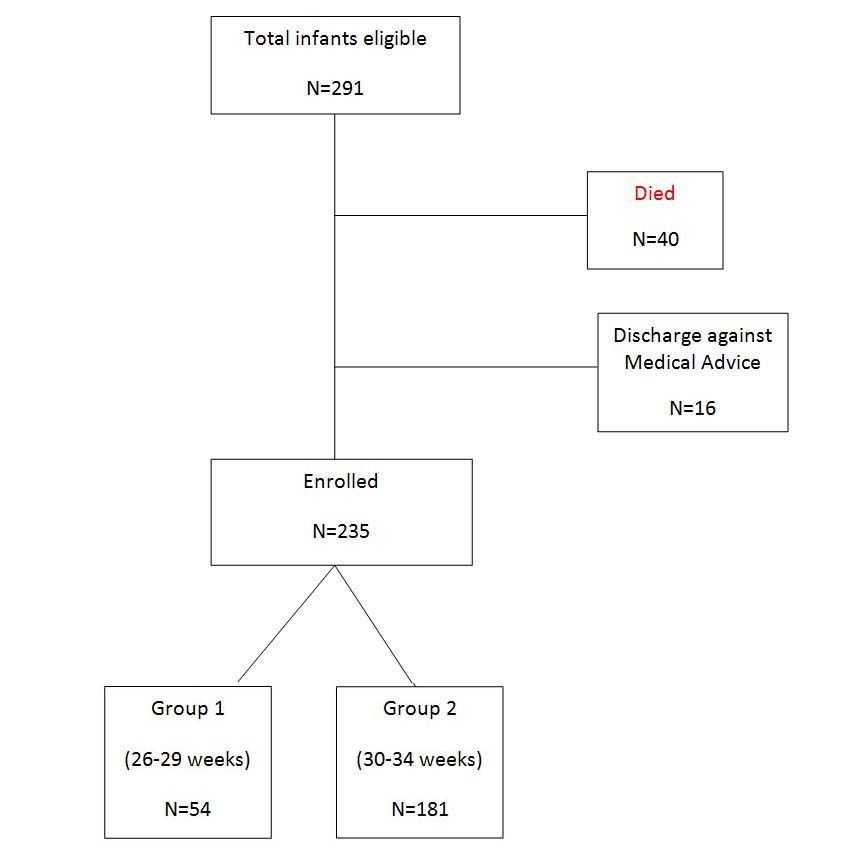
A total of 291 infants were eligible for the study; 40/291 infants died and another 16 were discharged against medical advice. A total of 235 infants were therefore, enrolled for the study [Table/Fig-1].
Participant flow diagram.
The median (IQR) birth weight was 1010 (872, 1113) and 1300 (1170, 1415) grams in group I and group II respectively [Table/Fig-2]. The mean (SD) duration of nursery stay was 42(19) days in group I compared with 19(14) days in group II infants. The median (IQR) gestational age and weight at discharge was 35 (34, 37) weeks and 1380 (1258, 1461) grams in group II infants. Various morbidities in both the groups are shown in [Table/Fig-3].
Neonatal demographic characteristics.
| Variables | 26-29 weeksN=54Median(IQR) | ≥30 weeksN=181Median(IQR) |
|---|
| GA at birth (weeks) | 28 (27.25, 28.75) | 32 (31, 34) |
| Birth weight (grams) | 1010 (872.5, 1113.75) | 1300 (1170, 1415) |
| GA at discharge (weeks) | 33 (32, 35) | 35 (34, 37) |
| Weight at discharge (grams) | 1338 (1212, 1443.25) | 1380 (1258, 1461) |
| Duration of stay (days) | 43.5 (30, 53.75) | 16 (11, 24) |
| Re-admission rates (%) | 0 | 5 (2.7%) |
| Variables | 26-29 weeksN=54 | ≥30 weeksN=181 |
|---|
| Blood culture positive sepsis | 6 (11.11%) | 8(4.42%) |
| NEC stage ≥2 | 2 (3.7%) | 5 (2.76%) |
| IVH | 5 (9.25%) | 4 (2.21%) |
| ROP | 9 (16.67%) | 1 (0.53%) |
| BPD | 17 (31.48%) | 7 (3.86%) |
Abbreviations: NEC, Necrotising Enterocolitis; IVH, Intraventricular Hemorrhage; ROP, Retinopathy of Prematurity; BPD, Bronchopulmonary Dysplasia
There were 5 (2.7%) re-admissions in the first four weeks after discharge in group II whereas, none in group I; 2 were re-admitted for anemia and received blood transfusion and the other 3 were admitted for suspected sepsis, feed intolerance and poor weight gain after discharge. There were no deaths in the month after discharge in either group of infants.
Discussion
South Asia and sub-Saharan Africa account for more than 60% of preterm births [15]. It has been found that 12.8 million babies were born small for gestational age in India in 2010 [16]. Due to constraints of bed availability and poor socio-economic status of the parents, early home discharge of pre-mature infants becomes a priority. Balancing the benefits versus risks of discharging ex-preterm (gestation <34 weeks) infants home especially after a prolonged stay in the NICU, is a tough task in a resource limited set up given the poor access to healthcare after discharge and the socio-economic status of the parents. Most neonatologists tend to be conservative in discharging such infants. Our results indicate the short term safety of early discharging ex-preterm infants (gestation<34 weeks at birth) home in our set up.
The birth weight and gestation and corrected gestation and weight at discharge for group I (26-29 weeks at birth), and group II (30-34 weeks) infants and their duration of NICU stay are shorter than that reported from previous studies in similar set ups. Mokhachane et al., (South Africa, 2006) assessed the outcomes of preterm Very Low Birth Weight (VLBW) infants discharged early at weight ≥1650g (n=62) compared with ≥1800g as per routine practice (n=62) in a Randomized Controlled Trial (RCT) [17]. Of the total 120 infants who were followed, the rate of gain in weight (mean 30 vs. 33g/kg/day, p=0.06) and head circumference (38.9 vs. 39.5cm, p=0.10) were similar in both groups. The number of re-admissions (9 vs. 4, p=0.17) and mortality {1 (1.6%) vs. 3 (5.2%), p=0.27} after discharge were also similar among the two groups. It was concluded that, if home circumstances are adequate, it is as safe to discharge well, singleton VLBW infants from hospital at a weight of ≥1650g or ≥1800g [17]. Singer et al., reported that, even in under developed communities, singleton infants born outside the winter months and with reasonable clinic or home visiting facilities can be discharged at a weight of ≥1800g [18]. In their study, 495 LBW infants were discharged based on the following criteria: a) no clinical evidence of disease; (b) satisfactory feeding by breast or bottle or both; and (c) stable temperature control under normal room conditions. Of the 495 infants 264 fulfilled these criteria when they weighed 1801-1900 g (Group 1), 99 when they weighed 1901-2000g (Group 2) and 132 (Group 3) when they weighed 2001-2500g. The overall follow-up rate was 85.5%. Re-admission rates for group 1, 2 and 3 infants were 9.5%, 1% and 0.8%, respectively with the commonest single reason being bronchopneumonia with hypothermia. Altogether 60% of the re-admissions occurred during winter when hypothermia played a significant part in morbidity and mortality. Twins, particularly in group 1, had a 3 fold higher mortality than singletons in the same group. Cruz et al., conducted a RCT, discharging VLBW infants at 1300 vs. 1800gm [19]. Eligible infants (n=43) were entered into the study at 1300 to 1350gm when they met behavioral criteria for discharge and the family home was approved. Follow-up showed no differences in weight gain or incidence of infection in the home vs. hospital group infants. A significant saving in hospital stay and costs was realized for the home group. Family co-operation was more in the home group.
Studies reporting on discharge policies for preterm infants from developed nations are limited. Altman et al., assessed the Post-menstrual Age at Discharge (PMAD) for moderately preterm infants (n=2388, gestation at birth: 30-34 weeks) and its relation to peri-natal risk factors and the organization of care in Swedish perinatal network units [20]. The mean PMAD was 36.9 (1.7) weeks. High (≥35 years) maternal age, multiple birth, small for gestational age, respiratory distress syndrome, infection, hypoglycaemia and hyperbilirubinemia were significantly associated with higher PMAD, but could explain only 13% of its variation. Mean PMAD differed by up to 2 weeks between hospitals. Infants cared in units without fixed discharge criteria had 4.7 days lower PMAD and those receiving domiciliary care had 9.8 days lower PMAD. Breastfed infants had lower PMAD (mean 2.7 days lower) than those not breast fed. They concluded that, perinatal risk factors had small overall impact on length of hospital stay in moderately preterm infants, whereas, organization of care was probably an important factor. A study from Singapore (2008) audited the discharge patterns of 36 preterm infants. The underlying causes leading to and the root causes of discharge delays were identified as requiring goal weight of 2 kg, even when medically fit, delayed delivery of discharge plan to parents, delayed discharge planning and no ownership in discharge planning [21]. The length of hospital stay was reduced 59.8%, primarily by improved discharge planning, revising discharging weight guidelines and mental and psychological preparation of parents for infant care at home.
A recent report from the Canada indicates that infants born at <34 weeks’ gestation are usually discharged at the PMA between 37 and 40 weeks [4,5]. In their system, 50% of preterm infants <37 weeks’ gestation at birth are discharged home directly from tertiary NICUs, and the remainder are transferred to community hospitals before discharge. Merritt et al., have reviewed professional guidelines, and standards of care for discharge of preterm infants. They point out that early discharge is clearly achievable for a large number of infants despite the variations in neonatal care practices that, influence NICU stay (e.g., management of apnea of pre-maturity, not discharging infants home as frequently on weekends vs. weekdays) [22]. The American Academy of Pediatrics (AAP 2008) recommends that, ‘It is prudent for each institution to establish guidelines that ensure a consistent approach yet allow some flexibility on the basis of physician and family judgment [8].’ It points out that the final decision for discharge is the responsibility of the attending physician, and must be tailored to the unique constellation of issues posed by each infant’s situation. Needless to say that in a resource poor set up, discharging an ex-preterm infant home before all physiologic competencies have been met, is a tough task, unless the team takes the easy approach to allow the parents a ‘discharge against medical advice’ to protect themselves from litigations.
Our study has shown feasibility and safety of early discharge in preterm babies below 34 weeks without any increased mortality or re-admissions in the first month of life. We acknowledge that this is retrospective study and doing a randomized trial is difficult in our scenario, however, an audit from more centers in developing as well as developed countries would definitely help in ascertaining the safety and feasibility of early discharge of preterm babies from the NICU.
Limitation
This is retrospective study and doing a randomized trial is difficult in our scenario. An audit from more centers in developing as well as developed countries would definitely help in ascertaining the safety and feasibility of early discharge of preterm babies from the NICU.
Conclusion
Our results indicate that early discharge of preterm neonates from the NICU at a much lower weight and post-natal age is feasible in a resource poor set-up. Developmental care interventions such as Kangaroo care, spoon feeding and parental participation that facilitate early discharge could be implemented in both, developing as well as developed countries for optimal use of resources and benefiting the parents from the socio-economic (reducing the time off work) and emotional bonding point of view. Early home discharge for preterm infants born before 34 weeks was safe in the resource poor set up of this study.
Abbreviations: NEC, Necrotising Enterocolitis; IVH, Intraventricular Hemorrhage; ROP, Retinopathy of Prematurity; BPD, Bronchopulmonary Dysplasia