Functional Outcome of Conservatively Treated Bilateral Neck of Femur Fracture in an Elderly: A Case Report
Prateek Sunil Joshi1
1 Assistant Professor, Department of Orthopaedics, Pramukhswami Medical College, Karamsad, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Prateek Sunil Joshi, Assistant Professor, Department of Orthopaedics, Pramukhswami Medical College, Karamsad, Gujarat, India.
E-mail: prateekortho@yahoo.com
Bilateral Neck of Femur (NOF) fractures is relatively rare. Surgery, either osteosynthesis or hemireplacement arthroplasty, is the mainstay of treatment. Significant complications are known to occur in such cases. In this case report, we present the functional outcome of a conservatively treated bilateral NOF fracture at one year, in a 93-year-old man.
Our patient, a 93-year-old gentleman, sustained right side NOF fracture in May 2014 and left side NOF fracture in May 2015, both after trivial fall. He did not give consent for surgery considering high operative risk. Now, at one year follow-up he has no true or apparent limb length discrepancy. He is ambulant with walker, self reliant for toilet care and other personal needs. Harris hip score is 75.80 and 69.65 after 1 year from right and left NOF fracture respectively.
In view of high mortality after surgery for NOF fracture in high risk patients or unavailability of resources, conservative treatment for bilateral NOF fracture can achieve satisfactory functional outcome in selected patients.
Bilateral femoral neck fracture, Conservative treatment, Harries hip score, Hip fracture
Case Report
A 93-year-old gentleman, non alcoholic and non smoker, presented to our hospital in May 2014 with chief complain of pain around right hip with difficulty in bearing weight after slip and fall at home. He was diagnosed to be having right hip neck of femur Garden type II, sub capital fracture [Table/Fig-1]. He was advised cemented hemireplacement arthroplasty after pre operative work up. ASA grade 4 consent was given for the surgery considering past history of Ischemic heart disease and hypertension. He had undergone angioplasty in 2008 and was diagnosed to be having hypertension since 2008. In view of high cardiac risk, patient refused for the surgery. He was treated conservatively with skin traction to reduce pain. As skin traction was intended for pain relief and not for reduction of fracture, it was continued for 4 weeks by which his pain subsided significantly. His blood investigations were normal. Bone Mineral Density analysis suggested severe osteoporosis which was treated with calcium and vitamin D3 supplements. Bed sore prevention was explained to the relative of patient and he was provided with water bed for the same. Mobilization with walker was started at 3 weeks from injury. Patient walked partial weight bearing till 3 months and then onwards full weight bearing. Patient was self reliant for all personal needs. He noticed progressive shortening of left lower limb from 6 months onwards following which his lurch increased. Four cm sole raise was prescribed for 5 cm shortening. At one year from right NOF fracture patient was ambulant with stick, was self reliant for toilet needs and all other personal needs. He could climb stairs one at a time and sit on a chair for one hour but could not sit cross legged or squat. On examination, he had 5 cm supra-trochanteric shortening, fixed adduction deformity of 10 degree with 40 degree of further adduction possible. There was fixed flexion deformity of 10 degree with further flexion present till 70 degrees. There was 20 degree of fixed external rotation deformity with further rotation of 60 degrees. Harris hip score for right hip was 75.8 at one year from injury.
Radiograph showing right side Garden type II sub capital NOF fracture.

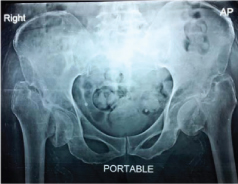
In May 2015, patient sustained another trivial fall at home following which again he was unable to bear weight on the lower limbs. He was diagnosed to be having left side garden type 4 trans-cervical NOF fracture [Table/Fig-2]. Proximal migration of right femur was also noted. Again, due to ASA grade 4 consent patient refused operative intervention. He started full weight bearing on left side at 6 weeks. At one year post left NOF fracture, X-ray revealed proximal migration of left femur [Table/Fig-3]. Patient was ambulant with walker with waddling gait. True and apparent lengths were equal bilaterally. Right hip movements were as before and left hip was in 15 degrees fixed flexion, 20 degrees fixed external rotation and 10 degrees fixed adduction deformity with further flexion till 60 degrees, adduction till 50 degrees and external rotation till 40 degrees [Table/Fig-4a,b]. Harris Hip score was 69.65. Patient could not climb stairs, could not sit cross legged or squat but he was ambulant with walker and was able to take bath and use toilet independently.
Radiograph showing left side Garden type IV trans-cervical NOF fracture with proximal migration of right proximal femur.

Radiograph of pelvis with both hips at one year from left NOF fracture showing proximal migration of left femur.
Range of motion of both hips at one year post injury to left hip.

Discussion
Unilateral NOF fracture is one of the most common fractures encountered in orthopedic practice. The frequency of NOF fractures will increase enormously in the developed as well as developing countries, as the number of old people is growing very rapidly. Melton estimated the global incidence of hip fractures to be 1.6 million in 1990 [1]. This figure is expected to rise to 4 million per year in 2025 and to 6.3 million in 2050. Bilateral NOF fractures, as such a rare type of injury, are also likely to increase in near future. Bilateral NOF fractures are extremely rare and have been associated with high-energy trauma [2], repetitive minor trauma, abnormal anatomy [3], seizure [4], electrical injury, electroconvulsive therapy, primary or secondary bone diseases such as osteomalacia [5], hyperparathyroidism [6], chronic renal failure [7] or severe osteoporosis, especially after corticosteroid or other corticosteroid like drug therapy. It is said that the non-operative treatment is acceptable for nondisplaced femoral neck fracture. In a prospective study, 170 impacted femoral neck fractures were treated by early mobilization and weight-bearing. Out of 170, 143 fractures (86%) got united [8]. It is general conscience that displaced NOF fracture requires operative treatment, either fixation of fracture or replacement surgery but there is significant risk of multiple life threatening complications, especially in elderly patients with NOF fracture. This is predominantly due to their co-morbid illnesses and compromised cardio-respiratory function. Eiskjaer et al., recorded mortality rate of 20% at 6 months and 28% at one year [9]. Surgical risk and complications increases substantially in surgically treated bilateral NOF fracture. Whereas Faraj study conducted by Adnan concluded that 2 out of 16 patients treated non-operatively died within 4 months of injury (12.5%) and the overall mortality at 4 years was 25% [8]. The mortality rate therefore is not any worse than that reported in the literature for patients whose fracture was treated surgically [10-12]. Hence, when there is high surgical risk or nonwillingness of the patient to get operated, conservative treatment such as traction, de-rotation boot and early mobilization should be considered as better option of treatment. There are many articles describing outcome of operative intervention for bilateral NOF fractures. However, we could not find any article describing outcome of conservatively treated bilateral NOF fracture, occurring either sequentially or simultaneously. Our case report describes outcome of conservatively treated bilateral NOF fracture in a 93-year-old man. In our case, patient’s unwillingness was the reason for conservative treatment. During both occasion of NOF fractures, he was treated with skin traction to alleviate pain and was mobilized as soon as possible to prevent complication of long term recumbent position. We noticed good functional outcome with Harries Hip Score of 75.8 and 69.65 after one year from individual NOF fracture. Our patient was able to walk with walker while bearing full weight without much pain as fractured trochanter with neck migrates proximally and gets stabilized against outer concavity of ilium acting as pseudo acetabulum.
Conclusion
Our case-report suggests that we should consider option of conservative treatment for bilateral NOF fracture patient if there is high risk for surgery. With appropriate physiotherapy and positive reinforcement, highly motivated and compliant patient with bilateral NOF fracture can achieve acceptable outcomes even after conservative treatment.
[1]. Melton LJ, Hip fractures: a worldwide problem today and tomorrowBone 1993 14:S1-8. [Google Scholar]
[2]. Schroder J, Marti RK, Simultaneous bilateral femoral neck fractures: case reportSwiss Surg 2001 7:222-24. [Google Scholar]
[3]. Annan IH, Buxton RA, Bilateral stress fractures of the femoral neck associated with abnormal anatomy: a case reportInjury 1986 17:164-66. [Google Scholar]
[4]. Suh KT, Kang DJ, Lee JS, Bilateral intertrochanteric fractures after surgical treatment of bilateral femoral neck fractures secondary to hypocalcemic convulsions with chronic renal failure: a case report and review of the literatureArch Orthop Trauma Surg 2006 126:123-26. [Google Scholar]
[5]. Chadha M, Balain B, Maini L, Spontaneous bilateral displaced femoral neck fractures in nutritional osteomalacia-a case reportActa Orthop Scand 2001 72:94-96. [Google Scholar]
[6]. Chen CE, Kao CL, Wang CJ, Bilateral pathological femoral neck fractures secondary to ectopic parathyroid adenomaArch Orthop Trauma Surg 1998 118:164-66. [Google Scholar]
[7]. Madhok R, Rand JA, Ten year follow-up study of missed, simultaneous, bilateral femoral-neck fracture treated by bipolar arthroplasties in a patient with chronic renal failureClin Orthop 1993 291:185-87. [Google Scholar]
[8]. Faraj AA, Non-operative treatment of elderly patients with femoral neck fractureActa Orthop Belg 2008 74:627-29. [Google Scholar]
[9]. Eiskjaer S, Ostgard SE, Risk factors influencing mortality after bipolar hemiarthroplasty in the treatment of fracture of the femoral neckClin Orthop Relat Res 1991 (270):295-300. [Google Scholar]
[10]. Kyo T, Takaoka K, Ono K, Femoral neck fracture. Factors related to ambulation and prognosisClin Orthop 1993 292:215-22. [Google Scholar]
[11]. Raaymakers EL, Marti RK, Non-operative treatment of impacted femoral neck fractures. A prospective study of 170 casesJ Bone Joint Surg 1991 73-B:950-54. [Google Scholar]
[12]. Tidermark J, Zethraeus N, Svensson O, Törnkvist H, Ponzer S, Quality of life related to fracture displacement among elderly patients with femoral neck fractures treated with internal fixationJ Orthop Trauma 2002 16:34-38. [Google Scholar]