Atypical Pityriasis Rosea with Unilateral Presentation
Hoda Badakhsh1, Fahameh Fadaei2, Mahin Badakhsh3, Abbas Balouchi4
1 Resident, Department of Dermatology, Kerman University of Medical Science, Kerman, Iran.
2 Resident, Department of Dermatology, Kerman University of Medical Science, Kerman, Iran.
3 Lecturer, Department of Midwifery, Zabol University of Medical Science, Zabol, Sistanvbalouchistan, Iran.
4 Student, Department of Nursing, Student Research Committee, School of Nursing and Midwifery, Iran University of Medical Science, Tehran, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hoda Badakhsh, Afzalipour Hospital, Kerman, Postal Code-9993139146, Iran.
E-mail: ganjresearch@gmail.com
Pityriasis Rosea (PR) is a common skin disease and characterized by generalized scaly eruptions typically on the trunk and proximal extremities. Atypical presentations of PR are common and can be a diagnostic challenge for clinicians. Here we present a case of a 26-year-old female who presented with a sudden onset of several asymptomatic, erythematous and scaly plaques on her trunk. Plaques sized 0.5-1cm in diameter that were distributed unilaterally (right side) on her chest, back and axilla. Atypical cases of PR are fairly common and less readily recognized. Careful history, clinical evaluation and follow-up are important to avoid misdiagnosis of PR and physicians should be aware of PR variants so that appropriate management and reassurance can be offered. For atypical eruptions without a definite diagnosis, it is safer to consider lesional skin biopsy.
Skin biopsy, Skin disease, Scaly eruptions
Case Report
A 26-year-old female presented with a sudden onset of several asymptomatic, erythematous and scaly plaques on her trunk. Plaques sized 0.5-1cm in diameter that were distributed unilaterally (right side) on her chest, back and axilla. In close observation some of the lesions displayed annular morphology with peripheral collaret scaling. The rash preceded an upper respiratory tract infection 10 days prior. There was no history of asthma, urticaria, drug allergies and she was not taking any medication. The left side of trunk, face, neck, upper and lower extremities, genitalia and mucous membranes were not involved [Table/Fig-1]. Her systemic examination was unremarkable.
Unilateral distribution of skin eruptions and peripheral collaret scaling of the lesions.

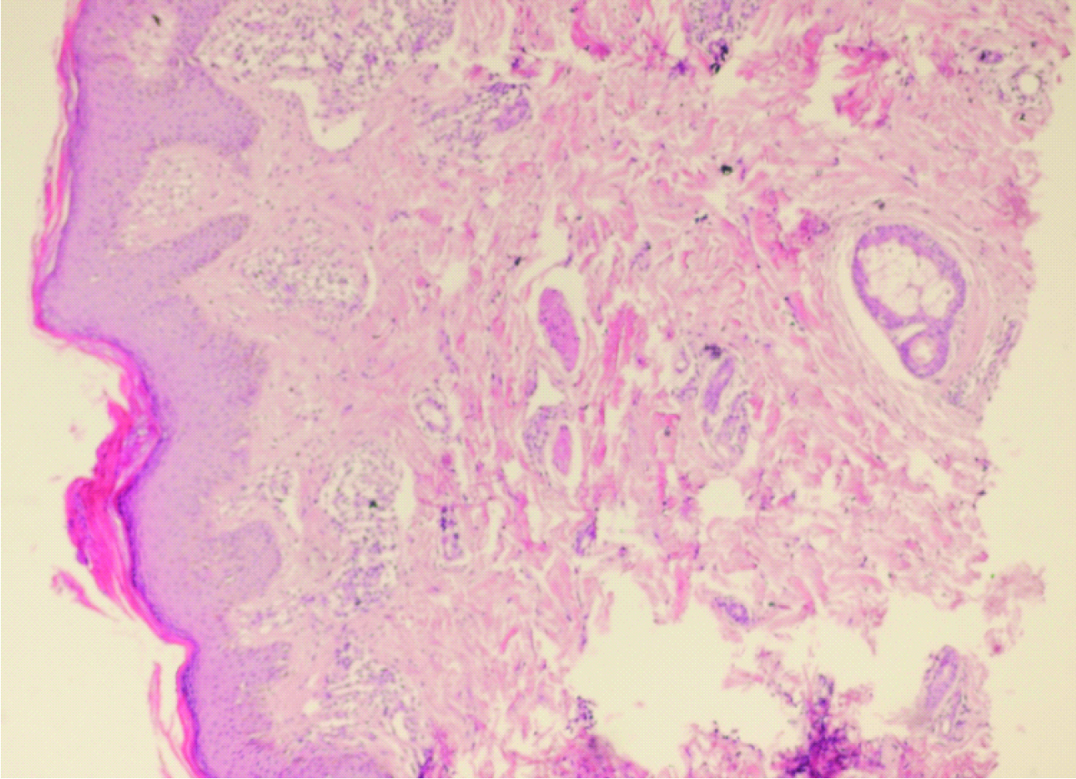
Complete Blood Count (CBC), liver and renal function tests and urine analysis were in normal ranges. In a patient who has a pityriasis-type rash and risk factors for sexually transmitted diseases (e.g., intravenous (IV) drug use, HIV infection, or promiscuity), syphilis should be considered to be present until proved otherwise. Similarly, if there is no herald patch, one should consider syphilis. Rarely, herpes zoster infection is confused with the vesicular variant of PR. Persistent PR has been linked with and attributed to persistent reactivation of HHV-6 and/or HHV-7 with higher viral loads than in typical PR in a study of 12 patients [1]. Biopsy from representative lesions showed focal parakeratosis, mild epidermal hyperplasia and spongiosis, extravasation of RBC around superficial vascular structures and mild perivascular lymphocyte infiltrate [Table/Fig-2].
Histologic picture. Skin tissue is seen with mound of parakeratosis, mild acanthosis/ Dermis shows edema, mild perivascular lymphocytes infiltrate and extravasated RBC (H&E staining 10X).
According to clinical and histopathological findings atypical PR was diagnosed. The patient was treated with oral erythromycin (500mg) and Topical Corticosteroid Agent for two month. The lesions were resolved within one month. This case is interesting because the skin lesions were localized on right side of the trunk.
Discussion
PR is characterized by the initial eruption of a Herald patch, which is followed by generalized scaly oval eruptions typically on the trunk and proximal extremities along the Langer’s lines of cleavage, giving the characteristic “christmas tree appearance” [2]. PR maybe atypical in the lesions or in its course [3]. Atypical case of PR are fairly common and less readily recognized than typical eruptions and may pose a diagnostic challenge [4]. PR is a common cutaneous disease reported in all races with an incidence of 6.8 per 1000 dermatological cases [5]. It is an acute, self-limiting disease, affecting mainly children and young adults [3]. Most cases of PR occur between the ages of 10 and 35 years it is uncommon in infancy, early childhood or old age. It is slightly more common in females [5]. The typical eruption lasts 6 to 8 weeks, though exceptionally it can persist for 5 month or longer. Some authors report a modest seasonal variation with peaks in the spring and fall [6]. Aetiology is probably viral, Human Herpesvirus (HHV6) and Human Herpesvirus (HHV7) have been suspected [7]. Although it has remained controversial [8]. PR classically presents with a singular, large scaling plaque that commonly appears on the trunk and gradually enlarges over a few days. The initial plaque is referred to as herald patch or mother patch and is often misdiagnosed as tinea corporis. The herald patch is estimated to occur in 80% of cases [4]. This initial lesion is followed by a squamous macular or papular eruption of the trunk and proximal limbs, with a christmas-tree distribution, usually non-itching. Classically lesions are covered by fine, dry, silvery-gray scales, with a marginal collaret of scale attached peripherally, with the free edge of the scale internally [5]. In darkly pigmented skin the lesion tend to be more papular and hyperpigmented [9]. Though diagnosis of PR is straight forward in its classic form, atypical cases may be missed easily and misdiagnosed. Atypical presentations of PR are observed in about 20% of the patients [10]. Atypical types can be differentiated by size (PR gigantea of Darier, Papular PR), distribution (cephalic PR, inverse PR, unilateral PR, localized PR and pityriasiscircinada et marginata of Vidal), sites involved (face, scalp, hands and feet fingers, toe tips, eyelids, penis and oral cavity), severities (PR irritate with severe itch, pain and a burning sensation), cause of the lesions (like relapse, recurrent PR, annual relapse) and morphology [11]. Papulovesicular, vesicular, purpuric, erythema multiform-like lesions and even pustular forms may rarely occur [5]. Unilateral presentation of PR is rare [10].
Histopathological findings in PR are not pathognomonic for the disorder [4]. It consist of superficial perivascular infiltrate of lymphocytes and extravasated erythrocytes that extend to the epidermis, where there is moderate acanthosis, spongiosis, decreased granular layer and mounds of parakeratosis [12]. Scaly annular, larger eruptions are known to occur in another rare variant known as PR of Vidal, which presents at limb girdles involving axilla and inguinocrural areas [13] But, a detailed history and follow-up in our patient did not point to other alternative diagnoses such as drug eruption, dermatophytosis, and contact dermatitis. The histopathological features are generally not diagnostic in PR and these usually presents with non-specific dermatitis. Skin biopsy is not routinely performed for diagnosis of PR in India but was possible in our case [14]. It may be helpful to rule out other diagnosis when in doubt. In our experience, in the absence of skin biopsy, a meticulous follow-up of clinical course in the given patient is helpful in arriving at a proper diagnosis [15].
Conclusion
Atypical cases of PR are fairly common and less readily recognized. Careful history, clinical evaluation and follow-up are important to avoid misdiagnosis of PR and physicians should be aware of PR variants so that appropriate management and reassurance can be offered. For atypical eruptions without a definite diagnosis, it is safer to consider lesional skin biopsy.
[1]. Drago F, Broccolo F, Ciccarese G, Rebora A, Parodi A, Persistent pityriasis rosea: an unusual form of pityriasis rosea with persistent active HHV-6 and HHV-7 infectionDermatology 2015 230(1):23-26. [Google Scholar]
[2]. Chuang T-Y, Ilstrup DM, Perry H, Kurland LT, Pityriasis rosea in Rochester, Minnesota, 1969 to 1978: A 10-year epidemiologic studyJournal of the American Academy of Dermatology 1982 7(1):80-89. [Google Scholar]
[3]. Tony B, Stephen B, Neil C, Christopher G, Rook’s textbook of dermatology 2004 United KingdomBlackwell Publishing Ltd [Google Scholar]
[4]. Ermertcan AT, Özgüven A, Ertan P, Bilaç C, Temiz P, Childhood pityriasis rosea inversa without herald patch mimicking cutaneous mastocytosisIranian Journal of Pediatrics 2010 20(2):237 [Google Scholar]
[5]. Gloster Jr HM, Gebauer LE, Mistur RL, Pityriasis RoseaAbsolute Dermatology Review 2016 Springer:31-2. [Google Scholar]
[6]. Atzori L, Pinna AL, Ferreli C, Aste N, Pityriasis rosea-like adverse reaction: review of the literature and experience of an Italian drug-surveillance centerDermatology Online Journal 2006 12(1) [Google Scholar]
[7]. Balci DD, Hakverdi S, Vesicular pityriasis rosea: an atypical presentationDermatology Online Journal 2008 14(3) [Google Scholar]
[8]. Tehranchi-nia Z, Rahimi H, Atypical pityriasis rosea with a target-shape herald patchIranian Journal of Dermatology 2010 13(1):24-26. [Google Scholar]
[9]. Vano-Galvan S, Ma D-L, Lopez-Neyra A, Perez B, Muñoz-Zato E, Jaén P, Atypical Pityriasis rosea in a black child: a case reportCases J 2009 2:6796 [Google Scholar]
[10]. Zawar V, Unilateral pityriasis rosea in a childJournal of Dermatological Case Reports 2010 4(4):54 [Google Scholar]
[11]. Gutte RM, Pityriasis rosea: two cases with uncommon presentations of common diseaseEgyptian Dermatology Online Journal 2011 7(2):12 [Google Scholar]
[12]. Jacyk WK, Pityriasis rosea in NigeriansInternational Journal of Dermatology 1980 19(7):397-99. [Google Scholar]
[13]. Drago F, Broccolo F, Rebora A, Pityriasis rosea: an update with a critical appraisal of its possible herpesviral aetiologyJournal of the American Academy of Dermatology 2009 61(2):303-18. [Google Scholar]
[14]. Zawar V, Giant Pityriasis RoseaIndian Jouranal of Dermatology 2010 55(2):192-94. [Google Scholar]
[15]. Robati R, Toossi P, Plantar herald patch in pityriasis roseaClinical and Experimental Dermatology 2009 34(2):269-70. [Google Scholar]