A Rare Association of Pentalogy of Fallot with Situs Inversus Totalis Complicated by Brain Abscess in an Adolescent–Case Report
Muhammed Basheer1, Sunil Kumar Agarwalla2
1 Junior Resident, Department of Paediatrics, MKCG Medical College, Brahmapur, Odisha, India.
2 Associate Professor, Department of Paediatrics, MKCG Medical College, Brahmapur, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Muhammed Basheer, Room No: 5, PG Hostel-2, MKCG Medical College, Brahmapur-760004, Odisha, India.
E-mail: drbasheerkt@gmail.com
Tetralogy of Fallot (TOF) is the most frequently diagnosed congenital cyanotic heart disease. It is often associated with additional findings, such as atrial septal defect (i.e., pentalogy of Fallot) or right sided aortic arch. Association of this pentalogy of Fallot with situs inversus totalis is rarely reported in paediatric literature and it can cause technical challenges to intracardiac repair. We report the case of pentalogy of Fallot with dextrocardia and situs inversus presenting as parieto-occipital abscess in a 12-year-old child. Complicated cardiac malformation like this when associated with brain abscess pose several challenges to the anaesthetist due to the altered haemodynamics and warrant a meticulous anaesthetic as well as surgical plan.
Atrial septal defects, Dextrocardia, Heart defects/congenital, Tetralogy of Fallot
Case Report
A 12-year-old boy was admitted with complaints of fever, headache and vomiting of 20 days duration. There was no history of loss of consciousness or focal neurological involvement. There was a history of infrequent episodes of cyanotic spell and exercise intolerance since 3 years of age. No history of palpitation or chest pain was there. He was not taken to any tertiary care centre due to financial constraints.
On general examination there was plethoric conjunctiva, marked central cyanosis and grade 3 clubbing. Neurological examination revealed neck stiffness and positive Kernig’s sign. There was no focal neurological deficit. On cardiovascular examination, apex was in right 6th intercoastal space 2cm lateral to mid-axillary line. On auscultation grade 3/6 ejection systolic murmur was heard, best at the right upper sternal border without any radiation. Respiratory system examination was within normal limits and per-abdomen no organomegaly was detected.
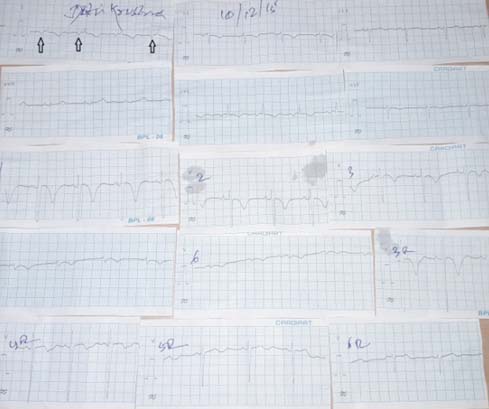
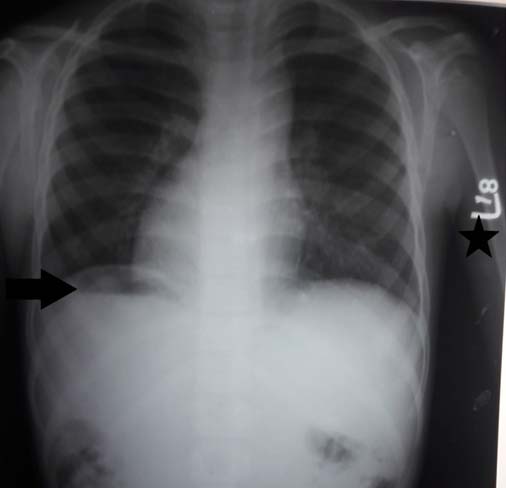
Blood tests revealed a haemoglobin level of 20.4 g%, haematocrit, of 59.3% and a raised Total Leucocytes Count (TLC) of 17,200cells/cmm. Other serum biochemical parameters were within normal limits. A 15-lead electrocardiogram yielded results consistent with dextrocardia [Table/Fig-1]. Chest radiograph showed dextrocardia with total situs inversus, without any apparent cardiomegaly [Table/Fig-2].
ECG consistent with dextrocardia. Inverted p-waves in Lead- 1 (arrow marks) and upright p-waves in Lead-aVF suggest situs inversus. Non progression of QRS complexes from V1 to V6 suggest dextrocardia.
Chest radiograph showing dextrocardia and situs inversus totalis. Arrow mark indicates fundic gas on right side and star mark indicates left side marked by radiologist.
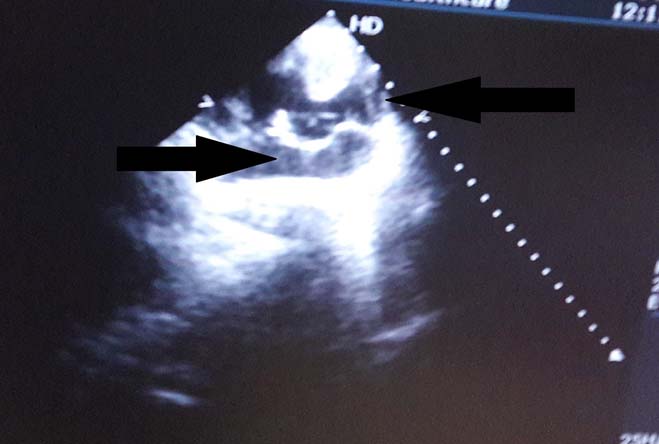
Transthoracic 2D echocardiogram revealed the anatomy of dextrocardia with situs inversus and Pentalogy of Fallot (POF): Ostium primum ASD, Inlet Ventricular Septal Defect (VSD) with Right Ventricular (RV) outflow tract obstruction [Table/Fig-3]. There were no other anomalies like right sided aortic arch.
Transthoracic Echocardiogram showing components of pentalogy of Fallot.
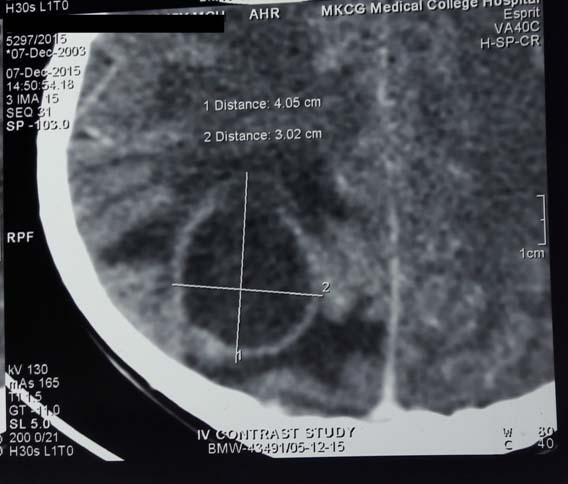
Computed Tomography (CT) scan of the brain revealed a well defined thin walled ring enhancing lesion in the right temporo-parietal lobe region (size 4.05cm× 3.02cm) without mass effect, probably pyogenic abscess [Table/Fig-4].
CECT-Brain magnified film showing ring enhancing lesion possibly abscess of size 4.05cm× 3.02cm.
The patient was treated with parenteral antibiotics empirically (Ceftriaxone, Vancomycin for 6 weeks; Metrogyl for 10 days) and steroids. After obtaining informed consent from parents, he was posted for emergency craniotomy and drainage of right temporo-parietal lobe abscess. Craniotomy was performed successfully and abscess was completely drained. Culture was sent and report showed Enterococcus species (sensitive to vancomycin, linezolid). Child is now asymptomatic with stable neurological picture. Patient was planned for surgical repair.
Discussion
The POF is a variant of the more common Tetralogy of Fallot (TOF), comprising the classical four features with the addition of an atrial septal defect. Though it was mentioned by Niels Stensen and Edward Sandifort; later, a detailed analysis and description was made by the French physician Étienne-Louis Arthur Fallot in 1888, after whom it is named [1]. Situs inversus (also called situs transversus or oppositus) is a congenital condition in which the major visceral organs are on the opposite side as compared to their normal positions. In the most common situation, situs inversus totalis, there is complete transposition of all organs. Dextrocardia refers to a condition where heart is located on right side of the chest [2-4]. The estimated prevalence of congenital heart disease in individuals with situs inversus totalis is around 5–10% and the most common lesion is transposition of great vessels [5]. Ostium secondum type of Atrial Septal Defect (ASD) is found commonly with POF than Ostium primum type [6]. Interestingly our patient had an ostium primum type of ASD.
After the initial diagnosis of dextrocardia we can treat patients with TOF and dextrocardia like any isolated TOF, with use of similar surgical procedures and postoperative monitoring. Old concept was, initial palliative systemic-to-pulmonary arterial shunt surgery, followed by definite repair surgery (usually when the patient was 3–5-year-old) to close the Vetricular Septal Defect (VSD) and resection of the Residual Volume (RV) outflow musculature [7,8]. But current school of thought is to go for a complete single-staged repair as early as 3 to 6 months of age, or even sooner if symptoms develop [7,8]. Decreased chance for development of aneurysm, ventricular dysfunction and rhythm changes make transatrial-transpulmonary approach a superior one as compared to transventricular approach [7].
Here, the altered spatial orientation of the cardiac structures is the major concern as far as patch closure of the VSD is concerned. The surgeon has to approach the VSD at a different angle in dextrocardia as compared to levocardia. Hence, there is a high chance for postsurgical heart block. Patients with cyanotic CHD are prone to developing brain abscesses and TOF is the leading cause for brain abscess [9]. This fact can be explained by the lack of filtering of blood by lung (due to right to left shunt) and hence organisms get an entry to brain. These septic foci later coalesce to form abscess.
Ideal anaesthesia management for a child with POF presenting for non cardiac surgery is very difficult. Ratio of Systemic Vascular Resistance (SVR) to Pulmonary Vascular Resistance (PVR) determines the amount of blood through R-L shunt. Greater the PVR and lesser the SVR, greater will be the shunt [9,10]. Therefore, the aim should be to reduce peri-operative test spells due to infandibular spasm, as it will worsen R-L shunt. Increased heart rate and effective myocardial contractility escalates the spasm, while hypotension (systolic BP <60mmHg) decreases the infandibular spasm. Similarly, hypotension (BP < 60mm Hg) can decrease SVR. Therefore, certain anaesthetic goals have to be aimed so as to avoid peri-operative cyanotic spells [10]. A case reports the incidence of a five-year-old child with brain abscess and an uncorrected POF, who underwent a successful emergency craniotomy [11].
Conclusion
Situs inversus totalis (situs inversus plus dextrocardia) can be very rarely associated with pentalogy of Fallot. In such a scenario altered spatial orientation of cardiac structures complicates the cardiac surgery and unfavourable hemodynamic complicates the non-cardiac surgeries like craniotomy for brain abscess.
[1]. Evans W.N, Tetralogy of Fallot and Etienne-Louis Arthur FallotPediatr Cardiol 2008 29(3):637-40. [Google Scholar]
[2]. Cotran RS, Kumar V, Robbins SL, Robbins Pathologic Basis of Disease 1989 4th edPhiladelphia, PaWB Saunders Co:777 [Google Scholar]
[3]. Fraser RS, Muller NL, Colman NC, Pare PD, Fraser and Pare’s Diagnosis of Diseases of the Chest 1999 Vol 34th edPhiladelphia, PaWB Saunders Co:2281-83. [Google Scholar]
[4]. Gutgesell HP, Cardiac malposition and heterotaxy. Garson AG Jr, Fisher DJ, Neish SR, edsScience and Practice of Pediatric Cardiology 1998 Vol 22nd edBaltimore, MdWilliams & Wilkins:1539-61. [Google Scholar]
[5]. Hagler DJ, O’Leary PW, Cardiac malpositions and abnormalities of atrial and visceral situs. Emmanouilides GC, Riemenschneider TA, Allen HD, Gutgesell HP, edsMoss and Adams’ Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adult 1995 Vol 25th edBaltimore, MdWilliams & Wilkins:1307-36. [Google Scholar]
[6]. Singh SP, Chauhan S, Talwar S, Sinus venosus atrial septal defect in a patient with Pentalogy of FallotAnn Card Anaesth 2012 15:166-68. [Google Scholar]
[7]. Apitz C, Webb GD, Redington AN, Tetralogy of FallotLancet 2009 374(9699):1462-71. [Google Scholar]
[8]. Starr JP, Tetralogy of Fallot: Yesterday and todayWorld J Surg 2010 34(4):658-68. [Google Scholar]
[9]. Pandian JD, Moosa NV, Cherian PJ, Radhakrishnan K, Brainstem abscess complicating tetralogy of Fallot successfully treated with antibiotics aloneNeurol India 2000 48:272 [Google Scholar]
[10]. Naqash I, Ahad B, Zargar J, Kirmani A, Wani M, Anaesthetic management of a case of tetrology of fallot for drainage of brain abscess: A case reportThe Internet Journal of Anesthesiology 2002 7(1) [Google Scholar]
[11]. Marulasiddappa V, Raghavavendra BS, Anesthesia for a rare case of uncorrected pentalogy of fallot undergoing craniotomy and drainage of brain abscessJ Clin Diagn Res 2015 9(7):UD01-UD02. [Google Scholar]