Osseous Hydatidosis of Femur in a Patient with Fracture Non-union: An Uncommon Entity
Kiruthiga Kala Gnanasekaran1, Anne Jennifer Prabhu2, Shyjumon George3
1 Assistant Professor, Department of Pathology, Christian Medical College, Vellore, Tamil Nadu, India.
2 Associate Professor, Department of Pathology, Christian Medical College, Vellore, Tamil Nadu, India.
3 Senior Resident, Department of Radiology, Christian Medical College, Vellore, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kiruthiga Kala Gnanasekaran, Department of Pathology, 4th Floor ASHA Building, Christian Medical College, Vellore, Tamil Nadu, India.
E-mail: kalkikiru@gmail.com
Hydatid disease caused by the larval form of the parasitic tapeworm, Echinococcus granulosus, commonly affects the liver and lungs. Bone involvement by Hydatid is extremely uncommon and is reported in 1-3% of cases. It is often a dormant disease, presenting at a late stage with non-specific clinical and radiological findings. Usually they occur as an isolated entity without liver/lung involvement and a clinical suspicion of this disease is not possible. We report a rare case of Hydatid cyst of femur in a 25-year-old female, with unresolving non-union of fracture for five years. The occurrence of this disease in atypical locations and lack of a specific radiological sign makes the diagnosis challenging and it is important for the orthopaedicians and pathologists to be aware of this entity for a precise diagnosis.
Cystic echinococcosis, Cyst wall, Hydatid cyst
Case Report
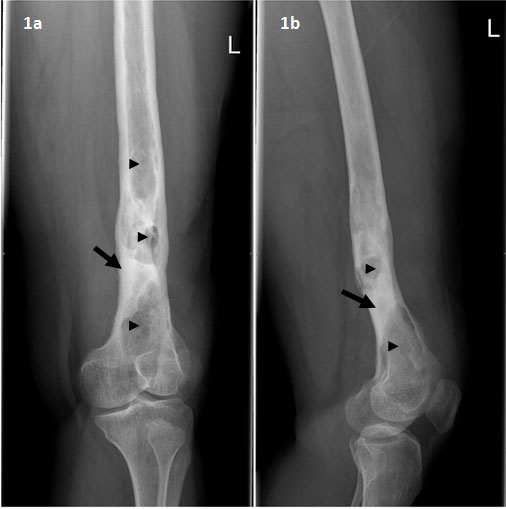
A 25-year-old female presented with complaints of pain and discharge from her left thigh since 5 years. She had a history of fall ten years back at her home and sustained fracture of the left femur. She was operated elsewhere and a plate was implanted. Six months after the surgery, she developed pain, swelling and discharging sinus from the wound site. She was treated with empirical anti-tuberculous treatment. Due to persistence of symptoms, the plate was removed one year later. Since then she has been complaining of discharging sinus on and off. On examination, she was found to have puckered scars and sinuses over the posterolateral aspect of distal third of left thigh. Plain X-ray revealed areas of cortical thickening and sclerosis with intervening cystic lucencies in the diaphysis. Mild periosteal reaction with contour deformity of the bone was also seen [Table/Fig-1a&b].
X-ray of left femur: Antero-posterior and Lateral view - Cortical thickening and sclerosis (arrows) with intervening cystic lucencies in the diaphysis (arrow heads). There is contour deformity of the bone.
Debridement, sequesterectomy and saucerisation were done and the specimen was sent to Department of Pathology for histopathological examination. Gross examination revealed multiple cysts folded like a membrane with a glistening grey white cut surface and many bony fragments.
Histopathological examination revealed viable and necrotic bone with parts of a cyst wall composed of acellular eosinophilic lamellated material surrounded by fibrosis and dense chronic inflammation with foreign body type of multi-nucleate giant cells [Table/Fig-2a&b]. A few protoscolices of Echinococcus granulosus with a chain of hooklets were seen in the germinal layer [Table/Fig-2c&d]. Hence a diagnosis of Hydatid disease was made and the patient was started on co-trimoxazole, praziquantel and albendazole. After 7 months, she presented to us with complaints of discharge from the wound site. Debridement from the left femur revealed necrotic spicules of bone, inflammatory granulation tissue and scolices of Echinococcus granulosus, suggestive of residual disease. Magnetic Resonance Imaging (MRI) of femur showed a few small pockets of T2 hyperintense lesions along the anterior, lateral and posterior aspects of mid and distal femur. A re-debridement was done with hypertonic saline wash and antibiotic laden cement was filled in the cortical window. Two strings of antibiotic beads, one in the soft tissue and one in the medullary canal was also inserted [Table/Fig-3]. The patient was adviced to continue praziquantel and albendazole for 6 months. After one year of follow-up, the patient is asymptomatic with good wound healing and no evidence of residual/ recurrent disease.
Acellular eosinophlic lamellated cyst wall surrounded by fibrosis and with foreign body giant cell reaction, (H&E, 20x and 40x).
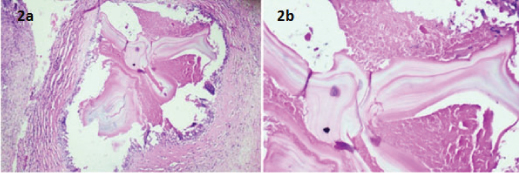
Protoscolices of Echinococcus granulosus with a chain of hooklets in the germinal layer, (H&E, 20x and 40x).
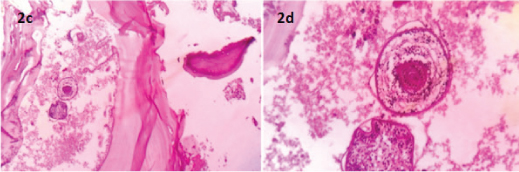
Post-operative X-ray: Strings with antibiotic beads in the medullary canal and soft tissue.

Discussion
Cystic Echinococcosis, commonly called Hydatid disease is caused by the larval form of the parasitic tapeworm, Echinococcus granulosus [1]. E. multilocularis causes alveolar hydatid disease, uncommon in man. Dogs and foxes act as definitive hosts, while sheep and cattle are the intermediate hosts. Man is a dead end incidental host, infected by ingestion of food that is contaminated by faecal matter of the definitive hosts [2]. The adult forms of the larva reside in the small intestine of the definitive host and release eggs and proglottids in the faeces. After ingestion by the intermediate hosts, the eggs hatch in the bowel, releasing oncospheres that have the capacity to penetrate the intestinal wall. They gain entry to the circulatory system and seed in various organs, most commonly the liver and lungs, by virtue of the rich vascularity of these organs [3]. Here the oncosphere will develop into a cyst which produces protoscolices and daughter cysts.
Around 55-70% of hydatid cysts occur in the liver and another 20-35% in the lungs. Extra-hepatic and extra-pulmonary involvement has been found to occur in 13% of cases of Hydatid disease by Adel et al., [4]. The other sites include spleen, kidney, eye and central nervous system. Bone involvement is very rare and account for <1% to 3% of all cases [5,6]. Osseous hydatid is common in adults with a mean age of 55 years [7] and the most common bones involved are the spine, long bones like femur, and tibia, ribs and pelvis [5]. Cystic Echinococcosis in the bone presents as an isolated lesion without involvement of the liver and lungs, unlike alveolar Echinococcosis where the bone lesions occur secondary to spread from the liver [8].
The most common presentation of Hydatid disease of long bones is pathological fracture [5]. Unlike the other sites like liver and lungs, growth in the medullary cavity of the bone is difficult because of the rigid architecture of the bone. Hence, the patient remains asymptomatic for a long duration. The primary lesion in the long bone is in the metaphysis or epiphysis, later spreading on to involve the diaphysis [9]. The cyst spreads through the medullary cavity and trabecular bone and often has a fragmented structure, due to the lack of adequate space for development of the cysts. Cortical erosion and periosteal reaction are not early features of osseous hydatidoses. As the cyst enlarges, it erodes through the cortex, producing lytic lesions, leading to weakening of the cortex and ultimately resulting in pathological fracture. The cyst also spreads along the periosteum and extends into the soft tissue. When this occurs, the lesion becomes calcified and can be easily diagnosed by imaging modalities. Invasion of the articular surface is rare, though sometimes extension into the joint space can occur.
Plain X-ray, computed tomography and MRI are the most commonly used imaging modalities to make a diagnosis of hydatid disease. On X-ray, Hydatid cyst appears as a multiloculated cystic lesion with no sclerosis or calcification. However, other conditions like osteomyelitis, arthritis, simple bone cyst, giant cell tumour, osteosarcoma, myeloma have similar clinical and radiological presentation and are more common in the differential diagnosis of osseous hydatid disease [7]. While CT is the investigation of choice for a diagnosis, MRI is a good choice to detect recurrences and soft tissue involvement [6,7]. In CT, there are three types of lesions that have been described, including osteolytic lesions, tumour like lesions and lesions that mimic infections [10]. However, Hydatid cyst of the bone is difficult to diagnose because of the non-specific findings and lack of the usual diagnostic signs [7]. Hydatid cysts of the bone do not show contrast enhancement or calcification. Daughter cysts and germinal layer are also very rarely seen in hydatid of bone, unlike in other parenchymal organs where the detachment of the germinal layer within a cystic structure gives the characteristic ‘water lily’ sign [7].
Hence, a pre-operative diagnosis becomes very difficult and the diagnosis is usually established at the time of surgery and confirmed by histopathological examination [9]. Other investigations like serum antigen- antibody assays and Casoni’s intra-dermal test are not sensitive and do not help in making a prompt diagnosis [6].
Wide local excision with a rim of healthy tissue, as for malignant tumours is the cornerstone of treatment for osseous hydatidoses [11]. A bone graft or PMMA (Polymethyl Methacrylate) can be used to fill the defects following excision, and the use of the latter has been shown to decrease the rate of recurrences [12]. Medical treatment using mebendazole and albendazole has also been tried often in combination with surgical excision, but with little benefit [2]. Most patients with osseous hydatidosis present at an advanced stage and complete cure is almost impossible as the disease is difficult to eradicate [5,9]. However, extensive resection of the involved bone with massive bone allograft has been proved to have better outcomes with no evidence of recurrence or relapse [13]. Our patient was also treated with massive bone allograft after the initial recurrence and is now free of disease at one year follow up. It is of paramount importance to follow-up these cases for a long duration, since, recurrences are not uncommon [14].
Conclusion
In conclusion, non-union of a fracture can be due to many causes like malnutrition, improper vascularisation, traction, persistence of infection etc. Infection as a cause of non-union has been found to occur in 30% of cases of non-union of femur in a recent study [15]. It is important for the clinicians and the pathologists to be aware of the rare occurrence of osseous hydatidosis, especially in a young patient presenting with unresolving non-union of fracture and non specific radiological features.
[1]. Bitar Y, Kanj SS, Zaatari G, Haidar R, Literature review and clinical presentation of solitary hydatid cyst in the tibia presenting with pathologic fractureEur J Orthop Surg Traumatol 2012 22(1):69-72. [Google Scholar]
[2]. Song XH, Ding LW, Bone hydatid diseasePostgrad Med J 2007 83(982):536-42. [Google Scholar]
[3]. Arik HO, Arican M, Cetin NK, Sarp U, Primary intraosseous hydatid cyst of femurIran Red Crescent Med J 2015 17(2):e21070 [Google Scholar]
[4]. Adel F, Ramia JM, Gijón L, de la Plaza-Llamas R, Arteaga-Peralta V, Ramiro-Perez C, Extrahepatic and extrapulmonary hydatidosisCir Cir 2016 :piiS0009-7411(16)30056-1 [Google Scholar]
[5]. Alldred AJ, Nisbet NW, Hydatid disease of bone in AustralasiaJ Bone Joint Surg Br 1964 46-B(2):260-67. [Google Scholar]
[6]. Walia JPS, Baldev Singh, Singh B, Kalaivanan K, Singh Sargun, Hydatid Disease of Femur - A Rare case ReportJ Int Med Sciences Acad 2011 24(1):37-8. [Google Scholar]
[7]. Tüzün M, Hekimoğlu B, CT findings in skeletal cystic echinococcosisActa Radiol Stockh Swed 1987 2002 43(5):533-38. [Google Scholar]
[8]. Merkle EM, Kramme E, Vogel J, Krämer S, Schulte M, Usadel S, Bone and soft tissue manifestations of alveolar echinococcosisSkeletal Radiol 1997 26(5):289-92. [Google Scholar]
[9]. Zlitni M, Ezzaouia K, Lebib H, Karray M, Kooli M, Mestiri M, Hydatid cyst of bone: diagnosis and treatmentWorld J Surg 2001 25(1):75-82. [Google Scholar]
[10]. Vasilevska V, Zafirovski G, Kirjas N, Janevska V, Samardziski M, Kostadinova-Kunovska S, Imaging diagnosis of musculoskeletal hydatid diseasePril Makedon Akad Na Nauk Umet Oddelenie Za Biološki Med Nauki Contrib Maced Acad Sci Arts Sect Biol Med Sci 2007 28(2):199-209. [Google Scholar]
[11]. Kural C, Ugras AA, Sungur I, Ozturk H, Erturk AH, Unsaldi T, Hydatid bone disease of the femurOrthopedics 2008 31(7):1-4. [Google Scholar]
[12]. Yildiz Y, Bayrakci K, Altay M, Saglik Y, The use of polymethylmethacrylate in the management of hydatid disease of boneJ Bone Joint Surg Br 2001 83(7):1005-08. [Google Scholar]
[13]. Muscolo DL, Zaidenberg EE, Farfalli GL, Aponte-Tinao LA, Ayerza MA, Use of Massive allografts to manage hydatid bone disease of the femurOrthopedics 2015 38(10):e943-46. [Google Scholar]
[14]. Raj DH, Dash PK, Hydatid disease of bone: a dangerous crippling diseaseBMJ Case Rep 2015 [Google Scholar]
[15]. Tsang STJ, Mills LA, Baren J, Frantzias J, Keating JF, Simpson AHRW, Exchange nailing for femoral diaphyseal fracture non-unions: Risk factors for failureInjury 2015 46(12):2404-09. [Google Scholar]