Secondary Aneurysmal Bone Cyst of the Scapula Treated by CT Guided Percutaneous Polidocanol Injection - A Case Report
Rahul Mohan1, Gopakumar Thanuvan Sreekumaran2
1 International Training Fellow, Wrightington Wigan and Leigh NHS foundation trust, United Kingdom.
2 Professor and Unit Chief, Department of Orthopedics, MES Medical College, Perinthalmanna, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rahul Mohan, House No. 30/990 A12, Prabha Apartments, MLA Road, Kovoor, Chevayur P.O, Calicut, Kerala-673017, India.
E-mail: rahulpidavoor@gmail.com
Aneurysmal Bone Cyst (ABC) is a rare benign tumour, usually affecting early age group and at the metaphysis of long bones. Scapular ABC’s are even more rare, especially successfully treated cases. Standard treatment methods like curettage have high recurrence rates hence, adjuvant therapy may be required to avoid recurrence. Polidocanol sclerotherapy is becoming popular because of its safety and efficacy and is being tried successfully for both active as well as aggressive primary ABC of size 3-5cm. We used the same principle in a large secondary ABC of the scapula, which to the best of our knowledge has not been yet reported. The index case is that of a 16-year-old girl who presented with severe pain and swelling of right scapula for 6 months duration with painful limitation of shoulder movements. After extensive evaluation, we diagnosed ABC of the scapula secondary to fibrous dysplasia which was successfully managed by CT guided percutaneous polidocanol sclerotherapy. One year after the injection, patient is asymptomatic with excellent radiological outcome. Polidocanol is an effective alternative to conventional methods since, it precludes functional disabilities like joint stiffness and shortening which are common with other methods.
Aneurysmal bone cyst, Benign tumour, Clinico-radiological outcome
Case Report
A 16-year-old girl presented with severe pain and swelling over the right scapula since, December 2014. She had visited a physician for the same about 6 months ago, who prescribed her analgesics. The pain subsided, but after 2 months she noticed a swelling over the right scapula which was gradually increasing in size. She had been bearing the pain and swelling since, the last 8 months. There was no history of trauma or constitutional symptoms. On palpation, swelling over the scapula was tender with local rise in temperature. Skin over the swelling was normal. It was a globular swelling with size 10x7cm, smooth surface, firm consistency and well defined margins. Shoulder joint palpated normally however, movements were painfully restricted. No breathing difficulties, lymphadenopathy and neurovascular deficits of right upper limb were marked.
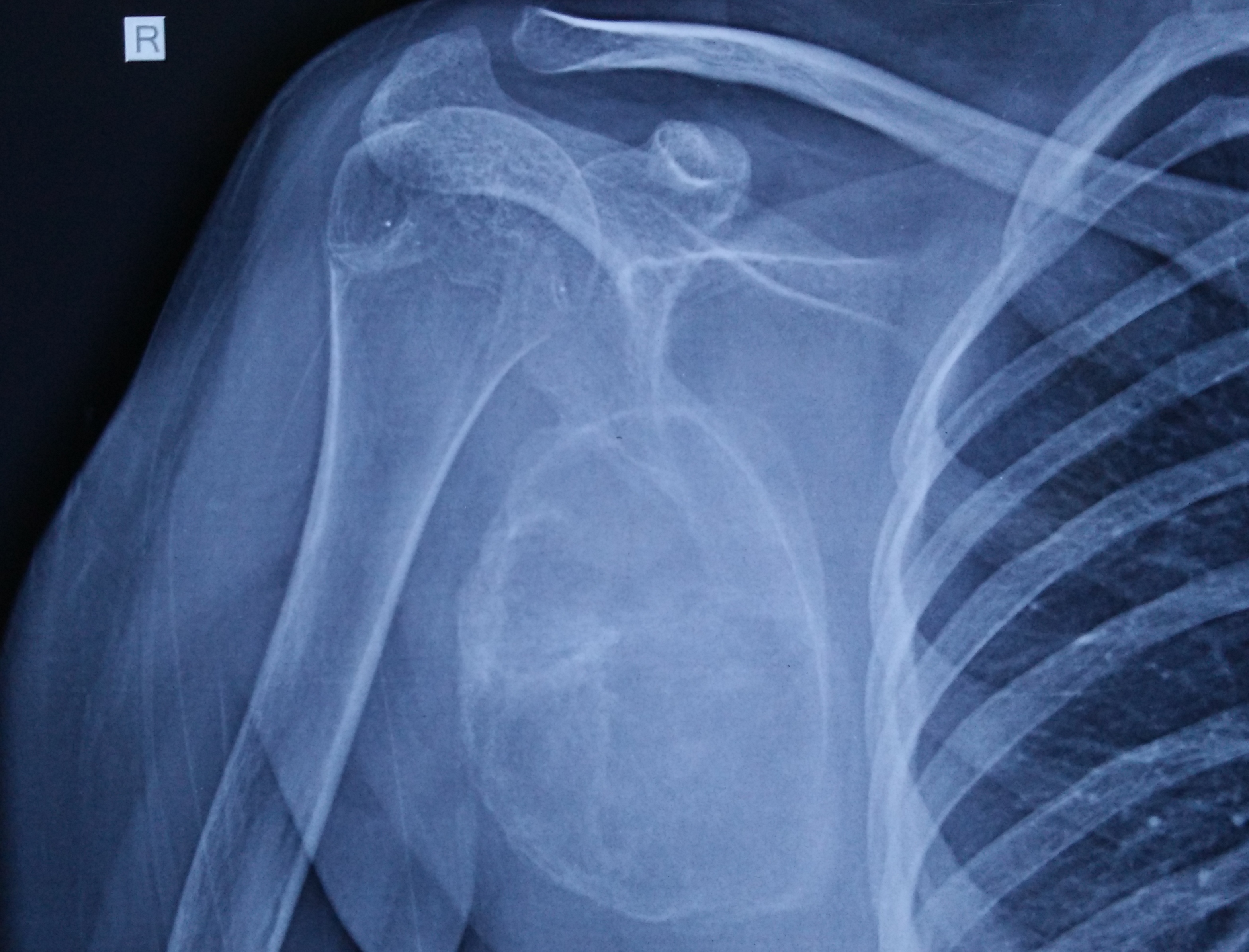
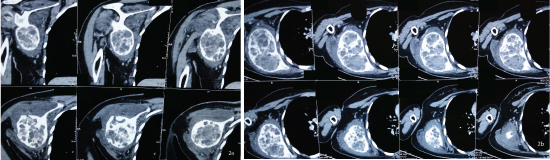
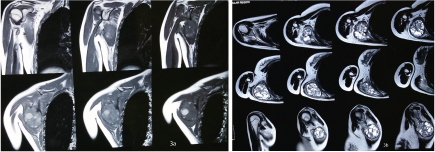
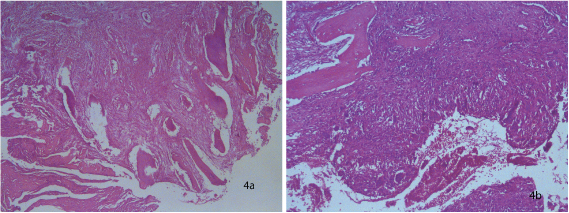
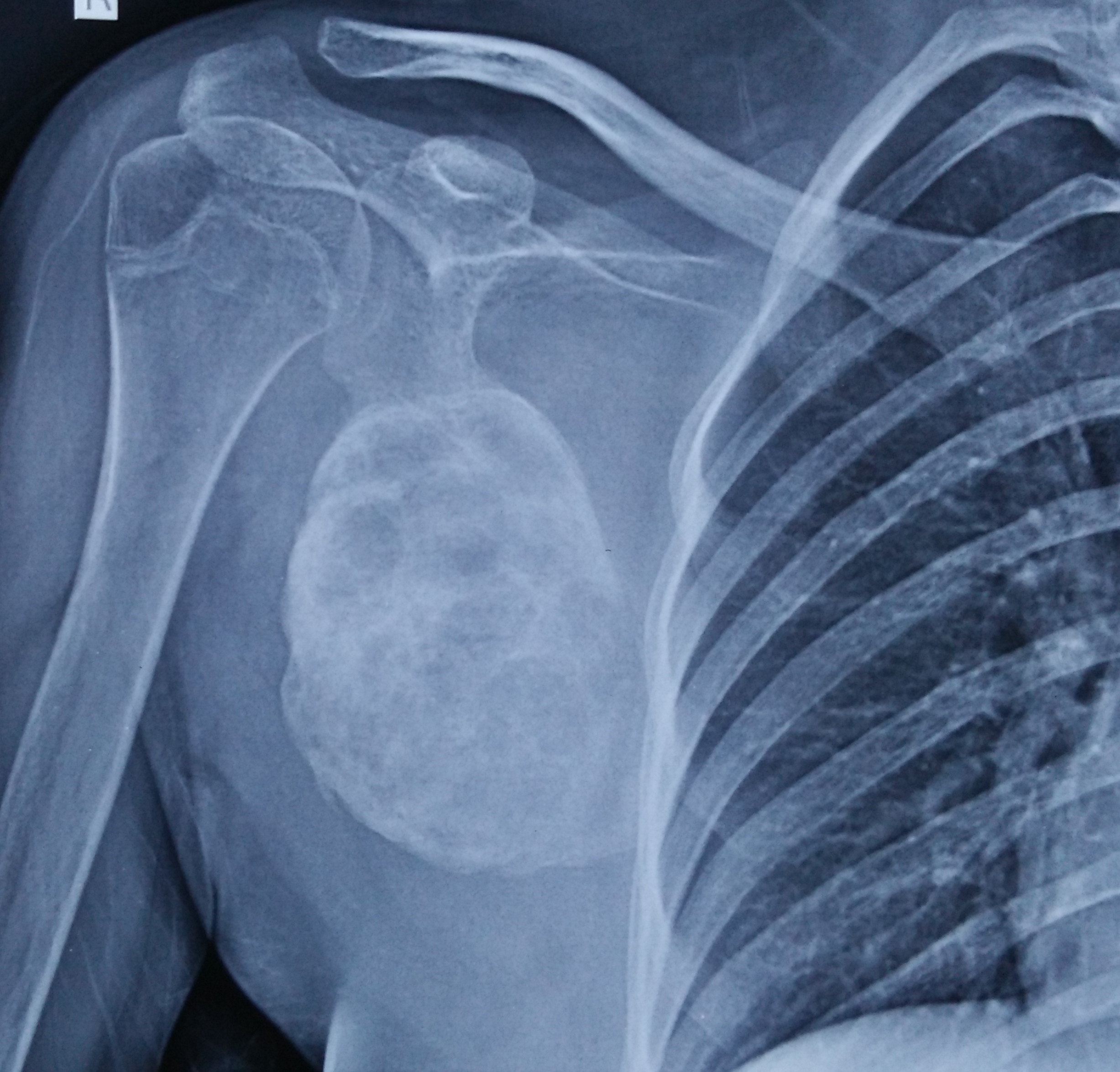
Blood investigations were normal except a raised ESR 64mm/hour. X-ray, AP view of right shoulder [Table/Fig-1] showed well defined, lytic, trabeculated, ballooned-out lesion outlined by subperiosteal bone formation of the lateral two thirds of the right scapula. Ultrasound scan revealed a large, cystic, hypoechoic, vascular and neoplastic lesion 6.3x5.4cm size from the posterolateral aspect of right scapula with cortical erosion. CT scan [Table/Fig-2a,b] showed expansile lytic lesion of approximate size 6x8.5x8cm affecting scapular wing with internal septations and sclerotic border. Focal areas of cortical break and multiple fluid levels were noted suggestive of ABC. Shoulder joint, acromioclavicular joint and clavicle were normal. MRI [Table/Fig-3a,b] showed well defined heterogenous mass with multiple fluid levels and surrounding soft tissue edema of size 6.5x4.3x5.3cm arising eccentrically from the lateral and lower half of the scapula. Axillary neurovascular structures were normal. MRI differentials were primary Aneurysmal Bone Cyst (ABC) or chondroid tumour. An aspiration was performed which yielded blood, that on cytological examination showed scattered osteoclastic giant cells. Trephine biopsy also revealed the same. The pain was unbearable for the patient and hence, an open biopsy was planned. An oblique incision 3cm long is made along the posterolateral aspect of the right scapula. Deep tissues are incised in the same plane till bone and a window is created over the scapula through which intra-cavitary tissues were scooped out along with a small piece of bone. The histopathological examination revealed mesenchymal tissue with woven bone suggestive of fibrous dysplasia, with features of secondary ABC [Table/Fig-4a,b].
X-ray right shoulder showing large expansile lytic lesion with trabeculations and surrounding host bone sclerosis involving almost entire scapula except medial and superior border.
CT scan showing expansile, lytic lesion of approximate size 6x8.5x8cm involving wing of right scapula with internal septations and sclerotic borders. Focal areas of cortical break and multiple fluid levels were noted.
MRI Scan showing a well defined mass of 6.5x4.3x5.3cm size arising eccentrically from the lateral and lower half of the right scapula and the lesion showed a heterogenous soft tissue mixed with multiple fluid levels and surrounding soft tissue edema.
Histopathology showing mesenchymal tissue with woven bone suggestive of fibrous dysplasia with features of secondary aneurysmal bone cyst like cavernous spaces filled with blood and haemosiderin deposits.
An extensive literature search was done and then we decided to manage her with 3% polidocanol injection. Treatment started after 14 weeks so that the biopsy site healed adequately. Volume of injection was determined from the tumour size measured by CT scan. Around 1ml of 3% polidocanol is required per cm3 volume of the tumour. CT measurement was 410cm3 hence, 410ml of polidocanol was required. Because this equation is applicable for small lesions less than 3cm and maximum dose at a time possible is 10ml [1], we decided to give 10ml (300mg) of polidocanol percutaneously under CT guidance. 2ml of 2% lignocaine with adrenaline was infiltrated to intended injection site followed by 10ml 3% polidocanol into the tumour through a 16G cannula. Injected fluid reflux was prevented by locking the cannula for some time and by injecting 1ml saline. Post-injection period was uneventful and the patient was discharged the next day with analgesics.
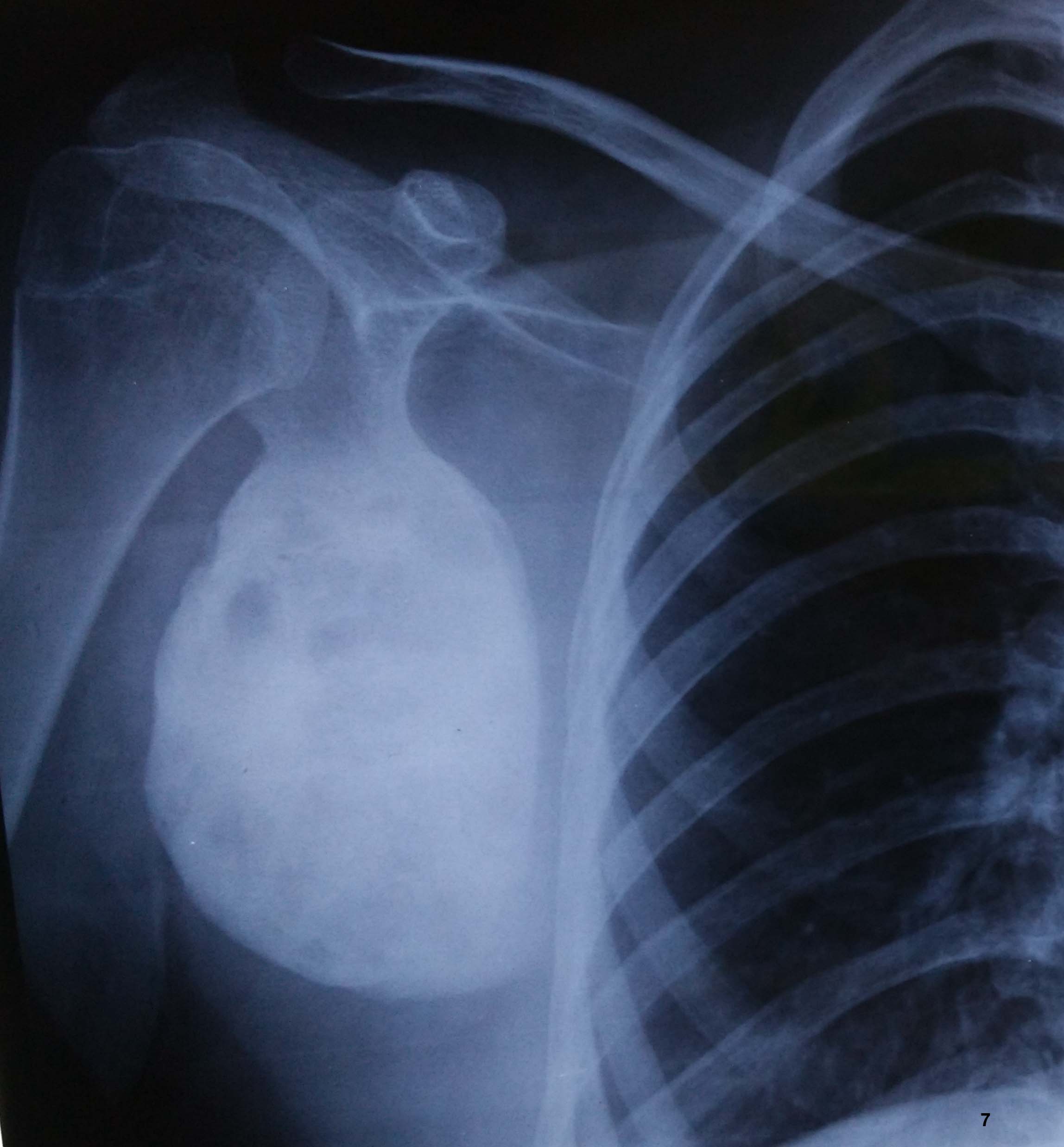
Patient was reviewed every two weeks. Eight weeks after the injection, she came with severe tenderness of right scapula with painful restriction of movements. Blood investigations were normal and X-ray showed mild sclerotic changes in the tumour [Table/Fig-5]. So, we repeated the injection and followed-up. After 2 months of second injection, pain subsided and range of shoulder movements improved [Table/Fig-6a,b]. After one year, she is absolutely painless with full range of shoulder movement. X-ray showed completely sclerotic lesion however, tumour size remained almost the same [Table/Fig-7]. According to the functional rating system of the Musculoskeletal Tumour Society for the upper limb, she had grade 5 functional score [2] and grade I radiological score (less than 25% of the residual lesion at one year) as per Rastogi et al., grading [1]. There was no complication except a hypertrophic biopsy scar.
X-ray right shoulder after eight weeks of injection showing mild sclerotic changes.
One year follow up showing excellent function with painless good range of motion of right shoulder.

X-ray at one year follow-up after injection showing complete sclerosis of the lesion however with mild reduction in size.
Discussion
Many cases of ABC have been reported after its first description by Jaffe and Lichtenstein in 1942 [1]. They represent only 1% of all primary bone tumours. Majority are between 5 and 20 years of age without any sex predilection. The common location of this tumour includes long bones, spine and pelvis [3]. Scapula accounts for 2-3% of all the locations [3]. Scapular ABC’s are rarely reported especially treated cases. ABC can either be primary neoplasm or secondary to an underlying primary tumour. Here, we are presenting a case of ABC of the scapula secondary to fibrous dysplasia, treated successfully with CT guided percutaneous polidocanol injection.
ABC’s are usually solitary, expansile, radiolucent lesions located at the metaphysis of the long bones. 70% of the ABC’s have been reported to be primary, while 30% secondary [3]. Secondary aneurysmal cysts are commonly associated with lesions like non-ossifying fibroma, fibrous dysplasia, chondroblastoma, giant cell tumour, telangiectatic osteosarcoma, chondrosarcoma and metastatic disease. Hence, when we consider the diagnosis of ABC, a thorough pre-operative evaluation and careful histopathologic studies are required to make sure that the ABC is not secondary [3].
Spontaneously healing of ABC’s are rare [4]. Conservative management should be considered only when the diagnosis is ascertained and the location and stage does not have any risk of fracture or destruction. Often, when the diagnosis of ABC is confirmed, active treatment is recommended. Without radical resection or amputation, ABC’s have a recurrence rate of 12% to 71% with different treatment options [5].
The origin and therefore, the management of ABC’s are controversial [6]. Different hypothesis has been put forward regarding its origin: arteriovenous fistula is the most classical. Post traumatic, de novo and venous impedance aetiologies are also proposed [1]. Many treatment modalities have been described. The most standard approach is curettage followed by bone grafting or cementation [7]. However, there is high incidence of local recurrence (more than 50%) after curettage [1] although Gibbs et al., reported use of mechanical burr, reduces the recurrence to 10% [8]. Adjunctive therapy like cementation, cryotherapy, or embolization, should be considered after curettage. Cementation followed by replacement bone grafting 4 to 6 months later, has been claimed to be more effective than curettage and bone grafting [9]. Cryotherapy as an adjunct to curettage and bone grafting also has been reported to reduce recurrence [10]. However, the probabilities of bleeding and injury are more with high speed burring and cryotherapy [1].
Embolization has been used earlier as the sole treatment [10]. Now it is commonly used pre-operatively to reduce the vascularity of the cyst and in locations of limited access, such as the spine and pelvis [11], however, it has a recurrence rate of 10.5% [1]. If the cyst is located in expendable bones like a rib or fibula, excision should be considered [12]. The bone destruction in ABC is mediated by RANK Ligand (RANKL) produced by the tumour cells. Denosumab, a human monoclonal antibody to RANKL, is effective in the treatment of ABC’s of bone [13].
Percutaneous methods for managing ABC, like doxycycline injection is being used effectively [4]. Percutaneous polidocanol sclerotherapy is becoming popular because of its safety and efficacy [1]. It’s use in active and aggressive small primary ABC’s are reported [1]. Sclerosants like polidocanol act by directly damaging endothelium, triggering coagulation cascade leading to blood vessel occlusion [14]. Polidocanol has been used safely in the treatment of venous malformations [15]. Since, most theories have some association with vascular origin, we decided to manage our case by sclerotherapy. Polidocanol is chemically hydroxypolyaethoxydodecan and is available in 2ml ampoules [1]. A 3% polidocanol is used for treating bone cyst, however, for treating venous malformations its 1%. Polidocanol for the treatment of secondary ABC’s proved to be a very effective alternative to conventional techniques since, it avoids functional disabilities like joint stiffness and shortening which are common with other methods [1].
Conclusion
The present case report further proves the effectiveness of polidocanol therapy. Polidocanol is an effective alternative to conventional methods since it precludes functional disabilities like joint stiffness and shortening which are common with other methods.
[1]. Rastogi S, Varshney MK, Trikha V, Khan SA, Choudhury B, Safaya R, Treatment of aneurysmal bone cysts with percutaneous sclerotherapy using polidocanol. A review of 72 cases with long-term follow-upJ Bone Joint Surg Br 2006 88(9):1212-16. [Google Scholar]
[2]. Enneking WF, Dunham W, Gebhardt MC, Malawer M, Pritchard DJ, A system for the functional evaluation of reconstruction procedures after surgical treatment of tumours of musculo skeletal systemClin Orthop 1993 286:241-46. [Google Scholar]
[3]. De Silva MVC, Raby N, Reid R, Fibromyxoid areas and immature osteoid are associated with recurrence of primary aneurysmal bone cystsHistopathology 2003 421:205-11. [Google Scholar]
[4]. Malghem J, Maldague B, Esselinckx W, Noel H, De Nayer P, Vincent A, Spontaneous healing of aneurysmal bone cysts: A report of three casesJ Bone Joint Surg Br 1989 71:645 [Google Scholar]
[5]. Shiels WE, Mayerson JL, Percutaneous doxycycline treatment of aneurysmal bone cysts with low recurrence rate: A preliminary reportClinical Orthopaedics and Related Research 2013 471(8):2675-83. [Google Scholar]
[6]. Dormans JP, Hanna BG, Johnston DR, Khurana JS, Surgical treatment and recurrence rate of aneurysmal bone cysts in childrenClinical Orthopaedics and Related Research 2004 421:205-11. [Google Scholar]
[7]. Papagelopoulos PJ, Choudhury SN, Frassica FJ, Bond JR, Unni KK, Sim FH, Treatment of aneurysmal bone cysts of the pelvis and sacrumJ Bone Joint Surg Am 2001 83:1674 [Google Scholar]
[8]. Gibbs Jr CP, Hefele MC, Peabody TD, Montag AG, Aithal V, Simon MA, Aneurysmal bone cyst of the extremities: Factors related to local recurrence after curettage with a high-speed burrJ Bone Joint Surg Am 1999 81:1671 [Google Scholar]
[9]. Ozaki T, Hillmann A, Lindner N, Winkelmann W, Cementation of primary aneurysmal bone cystsClin Orthop Relat Res 1997 337:240 [Google Scholar]
[10]. Cigala F, Sadile F, Arterial embolization of aneurysmal bone cysts in childrenBull Hosp Joint Dis 1996 54:261 [Google Scholar]
[11]. Koci TM, Mehringer CM, Yamagata N, Chiang F, Aneurysmal bone cyst of the thoracic spine: Evolution after particulate embolizationAJNR Am J Neuroradiol 1995 16:857 [Google Scholar]
[12]. Ramirez AR, Stanton RP, Aneurysmal bone cyst in 29 childrenJ Pediatr Orthop 2002 22:533 [Google Scholar]
[13]. Skubitz KM, Peltola JC, Santos ER, Cheng EY, Response of aneurysmal bone cyst to denosumabspine (Phila Pa 1976) 2015 40(22):E1201-04. [Google Scholar]
[14]. Aho HJ, Aho AJ, Pelliniemi LJ, Ekfors TO, Foidart JM, Endothelium in aneurysmal bone cystHistopathology 1985 9:381-87. [Google Scholar]
[15]. Guex JJ, Indications for the sclerosing agent polidocanol (aetoxisclerol dexo, aethoxisklerol kreussler)J Dermatological Surg Oncol 1993 19:959-61. [Google Scholar]